Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In memory of Axel Perneczky. The authors and the editors thank Dr. Shaan Raza and Dr. Rodrigo Ramos-Zuniga for their contribution in the previous edition.
The fundamental basis of “keyhole” neurosurgery lies in the fact that, if designed and tailored to the lesions, deep lesions can be approached via smaller incisions and craniotomies providing essentially the same anatomic visualization as the larger, more traditional cranial base approaches. The supraorbital craniotomy is the prime example of this trend in neurosurgery; with increased emphasis on maximizing cosmetic outcomes, minimizing tissue morbidity, and reducing hospitalization stays, there is now increased importance in understanding minimally invasive approaches (i.e., supraorbital craniotomy, keyhole craniotomies in general, and endoscopic endonasal approaches).
Paramount to the success of these approaches is a thorough understanding of the anatomy, because they can be difficult for novice surgeons who do not have a solid grasp of microsurgical corridors and cranial base anatomy/compartments. Anatomically relevant is the orbital bone because it forms the roof of the orbital cavity and a strategic part of the anterior floor of the skull base. The orbital ridge intersects with the zygomatic bone laterally and the ethmoid medially; the orbit is further contiguous with the anterior fossa and sphenoid bone. Consequently, it is an anatomic structure that is intimately associated with the orbital cavity and its structures, as well as with the intracranial region.
The supraorbital craniotomy and its variants essentially provide a combined subfrontal-anterolateral microsurgical approach. Anatomic structures such as the anterior clinoid, sphenoidal plane, and sellar region are keys to this corridor extending toward the region of the sylvian fissure. Therefore these anatomic structures are critical in planning any microsurgical trajectory to the anterior fossa floor, the middle fossa, the smaller wing of the sphenoid, and the sellar/parasellar region. , In following this outlined corridor, the supraorbital approach can give the surgeon access to ipsilateral anterior cranial fossa, basal frontal lobe and frontal pole, medial temporal lobe, lateral wall of cavernous sinus, ipsilateral proximal Sylvian fissure, opticocarotid cistern, suprasellar region, superior sella, lamina terminalis, perimesencephalic/interpeduncular cistern, and medial/superior aspect of contralateral optic nerve, chiasm, and carotid artery. In addition, adjunct use of an endoscope may help particularly with ensuring total tumor removal, reaching deep aneurysms and accessing surgical regions such as the anterior olfactory groove, supra and intrasellar space, inferior space directly under ipsilateral optic nerve, interpeduncular/perimesencephalic cistern, ipsilateral medial middle fossa, medial temporal lobe, and the anterior third ventricle. , , , ,
Previous anatomic studies have critically evaluated anatomic corridors in this region and their utility in treating a variety of neurologic lesions; these studies have subsequently resulted in potential surgical alternatives. Such historical and fundamental contributions have been made by Durante, Krause, Frazier, Cushing, Heuer, Dandy, Yasargil, Brock and Dietz, Al-Mefty, Zabramski, and Perneczky. Although the supraorbital approach is not a new strategy (initially described by Frazier with his epidural approach described in 1913), technological innovations have enhanced its applicability. This technique has continued to be refined over the past 20 years and routinely demonstrates comparable safety and efficacy to standard approaches. The introduction of new tools (e.g., endoscopy) and new approaches (i.e., orbital ridge osteotomy) has improved access to and visualization of cranial base lesions and, while the operative corridor is smaller in keyhole craniotomies, they still produce adequate deep exposure and maneuverability. Ultimately, neurosurgical and technological innovations have aimed to reduce morbidity under the concept of minimally invasive neurosurgery. , , , ,
It is important to consider the orbital region as an anatomic compartment bound superiorly by the frontal bone, medially forming a close angle with the ethmoid bone, lacrimal bone, and lacrimal fossa. In addition, there are connections to the nasal region.
In the inferior medial region, we find the adjacent palatine bone and in the lower border the maxillary bone, where the infraorbital foramen is located. Going toward the midlateral inferior region, we find the area of the zygomatic bone which in turn extends through the zygomatic arch toward the posterolateral aspect and going in an anterolateral location we find the facial zygomatic foramina. In the internal cavity of the orbital region the origin of the great wing of the sphenoid in its posterolateral portion is found—giving way to a virtual space between the small wing and the great wing of the sphenoid, known as the superior orbital fissure. Adjacent to the posterior medial portion are the optic canal located inferiorly and the inferior orbital fissure. ,
The ethmoid bone represents a complicated component of the craniofacial skeleton with several critical components. Medially, the ethmoid presents a lamina to the nasal cavity while superiorly it presents the cribriform plate. In addition, the ethmoid bone articulates with the sphenoid bone and sphenoid sinus along several surfaces posteriorly and inferiorly. Furthermore, a majority of the volume of the ethmoid bone consists of trabeculated air spaces creating the ethmoid air cells.
The posterosuperior orbital cone is made of the superior margin of the orbital fissure and the extension of the small wing of the sphenoid. The intracavitary foramina are the lacrimal foramen, the optic canal, the superior orbital fissure, the inferior orbital fissure, and in the extracavitary portion we find the notch or foramen for the infraorbital nerve and the orbital zygomatic foramen ( Fig. 26.1 ).
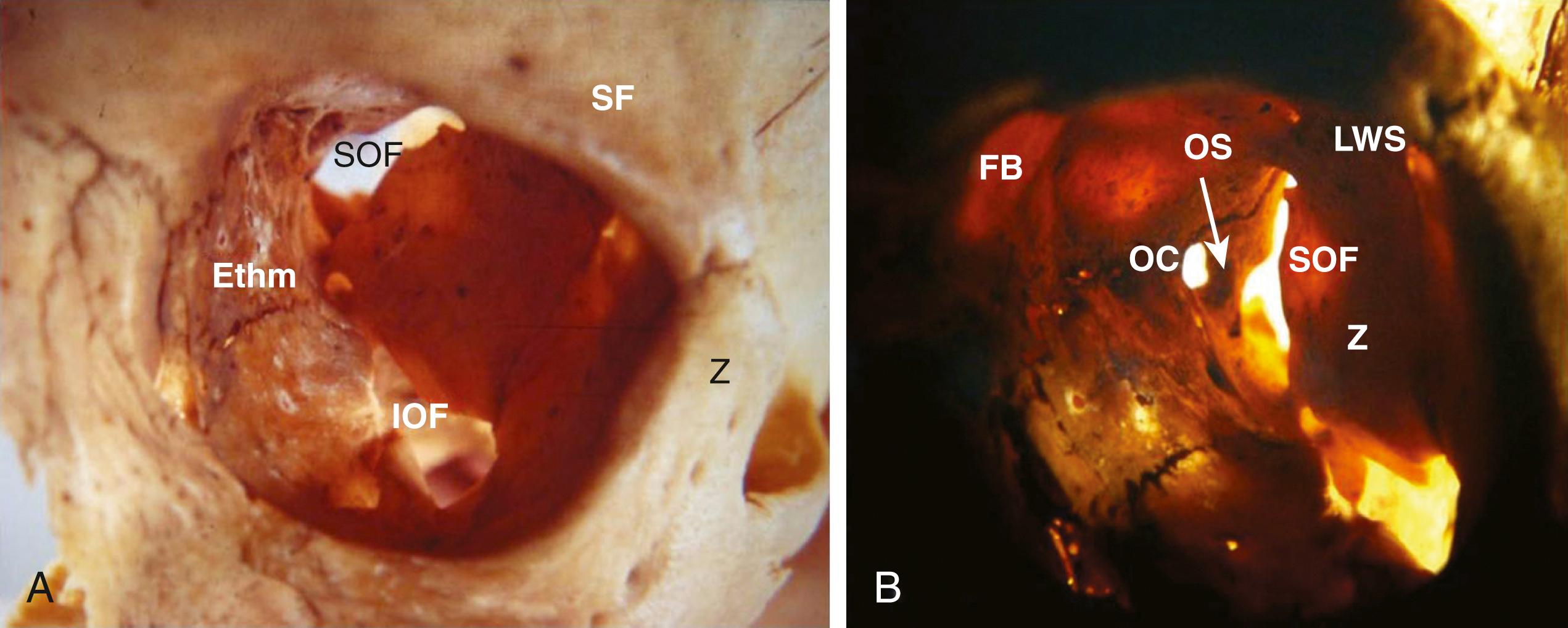
The optic canal and the anterior clinoid process are closely located and associated with the origin of the small wing of the sphenoid bone; the superior orbital fissure is divided by a bone strut (optic strut) supporting the anterior clinoid process. The most important structures involved in this region looking above (from the intracranial frontal floor perspective) are the anterolateral floor or the platform and the orbital arch. Toward the anterior medial portion, the crista galli and the cribriform plate of the ethmoid bone are found. The sphenoid plane and the wing of the sphenoid that meets the optic foramen are located in the deep plane ( Fig. 26.2 ). ,

The anatomic intraorbital structures are basically represented by the extraocular muscles, predominantly the rectal and medial and lateralis muscles, such as the levator muscle for eye movement. We also find the periorbital fat or periorbit and the globe itself, the optic nerve, and other nerve structures from the ophthalmic branch of the trigeminal nerve, such as the frontal, nasociliary, and lacrimal nerves. The rest of the ocular motor nerves—III, IV, and VI—converge in a particular anatomic site after passing through the cavernous sinus ( Fig 26.3 ).

The most important arterial structures are the ophthalmic artery, its variants in the lacrimal artery and its connections to the ciliary artery, and the central retinal artery, whose venous return flows through the ophthalmic vein. The anterior ethmoidal artery is a significant vessel in the anteromedial region. It is closely related with the nasolacrimal region and the irrigation of the nasal mucosa, frequently managed in surgical procedures to control nose bleeds. , ,
This specific anatomy gives way to the possibility of removing the orbital roof to have wide access to all the orbital area and ocular contents, nerve structures, muscles and vessels, and additionally have an intracranial access. An important anatomic structure from the surgical perspective is the lacrimal gland, located in the superior external area of the orbit. This is a region that can be compromised when using a surgical approach where the orbital roof is removed.
From the surgical perspective as well, it is important to emphasize the orbital surgical triangle, represented by a geometric figure that, from its lateral projection, the base is the anterior part of the frontal bone and the orbital arch, the upper part is outlined by the base of the frontal lobe, and the inferior part is outlined by the periorbit. This triangle, with an anterior base and a posterior vertex, may offer several options for deep resection (also representing the angle of bone removal described in the transsupraorbital approach; Fig. 26.4 ). ,

A series of cadaver specimens were studied to assess the variations described for the supraorbital craniotomy to evaluate the extent of surgical access in identifying different anatomic landmarks. , , , The conventional supraorbital keyhole approach was used to examine the optic nerve, ipsilateral anterior clinoid, sphenoidal plane, and the dorsum sellae. This approach, compared with the transsupraorbital approach, showed some benefit with regard to accessibility and visualization. , , ,
Subsequently, possible variants of this approach were analyzed in another experimental cadaveric study. In a series of 15 adult skulls, the differences between anatomic targets and the space around the sellar region were evaluated for these variants. Access to the following regions was assessed: the anterior clinoid process (ipsilateral), the chiasmatic sulcus, the optic canal, the center point of the sella turcica, and the dorsum sellae. Table 26.1 presents measurements for the classical supraorbital approach versus the supraorbital craniotomy combined with removal of the orbital arch.
| Technique | Anterior Clinoid Process Ipsilateral | Chiasmatic Sulcus | Optic Canal | Pituitary Fossa | Dorsum Sellae |
|---|---|---|---|---|---|
| Classical supraorbital approach | 5.57 ± 0.06 | 5.5 ± 0.09 | 5 ± 0.09 | 6.5 ± 0.09 | 6.97 ± 0.08 |
| Supraorbital craniotomy with orbital ridge osteotomy | 4.5 ± 0.09 | 4.5 ± 0.09 | 4 ± 0.12 | 5.4 ± 0.09 | 6 ± 0.12 |
Recognizing that the approach can be tailored, the craniotomy can be extended in different anatomic directions specific to the target pathology/region. For example, the supraorbital nerve can be mobilized in order to create a craniotomy more toward the midline. This modified approach facilitates a more comfortable and direct route to the prechiasmatic region, as well as other structures such as the crista galli, ethmoid lamina, olfactory bulb, sphenoidal plane, and anterior clinoid. ,
On the other hand, lateral extension, as with the supraorbital-pterional approach, permits greater pterional access. This modification permits greater access to the lateral targets in the frontotemporal neurosurgical corridor and their neurovascular structures. , , , ,
Finally, if the principles of minimally invasive surgery and skull base surgery are combined, using the supraciliary incision, it is possible to remove the orbital arch in a block in the medial and lateral portion, which provides an average of 1.5 cm more space to work in the craniotomy site, according to the anatomic studies of the transsupraorbital approach. ,
All of these variations of the supraorbital approach provide greater versatility and several possible adaptations to meet the surgical goal under the concept of supraselective craniotomy, which is the fundamental basis of the “keyhole” craniotomy. There are six basic variants of the supraorbital approach ( Fig. 26.5 ):
Supraorbital medial
Supraorbital anterolateral (classical)
Supraorbital pterional
Transsupraorbital
Eyelid (transpalpebral) supraorbital
Eyebrow supraorbital

The development of finer, more accurate, and angled instruments has been critical for success of the supraorbital approach and its variants. Likewise, a major breakthrough was the use of the surgical microscope complemented with endoscopy-assisted microneurosurgery. The concept of keyhole microsurgery set forth by Perneczky was based on this new technology that contributed to providing several new options. Although seemingly contradictory, keyhole cranial base surgery advocates maximal resection through the use of current surgical technology and methodology taking into consideration the patient’s condition and pathology. Thus variations in the orbital approach itself have led to improved extension and use in various surgical spaces granting access to the most important accessible structures. , , ,
Synonymous with the development of keyhole surgery has been the increasing acceptance of using smaller incisions, such as the eyebrow incision. The use of smaller incisions can have cosmetic, functional, and even psychological benefits for the patient. However, this fact should not limit the final surgical plan in view of the surgical goal. For example, a displaced frontal scalp flap/craniotomy can also be chosen to apply the principle of selective craniotomy. In other words, minimally invasive surgery does not simply mean a minimal incision or minicraniotomy; instead, the goal is to spare craniofacial and neurovascular structures using a tailored approach as broad as necessary and as selective as experience allows, with every possible manipulation of a conventional procedure. , ,
For example, disadvantages of the brow approach can include potential posterior alopecia of the eyebrow or frontalis weakness that occurs as a result of damage to the frontal branch of the facial; however, this may be ameliorated with preoperative mapping using a nerve conduction study. Another advantage of this approach is preservation of the temporalis muscle in comparison to other anterolateral-based approaches (i.e., pterional). Even with lateral extension of this approach, the soft tissue dissection involves only minimal mobilization of the superior and anterior most aspect of the temporalis—in this process the deep neurovascular supply is preserved. , , , , , , ,
To truly benefit from minimally invasive strategies, cases must be carefully selected upon consideration of the surgical objective, the patient’s individual anatomic variations, and the experience and comfort level of the surgical team. This strategy allows proper evaluation and ultimately helps the surgeon to identify the most adequate and beneficial approach for the patient.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here