Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
© 2018 Elsevier Inc. All rights reserved. Please note that the copyright for the original figures submitted by the contributors is owned by Contributors.
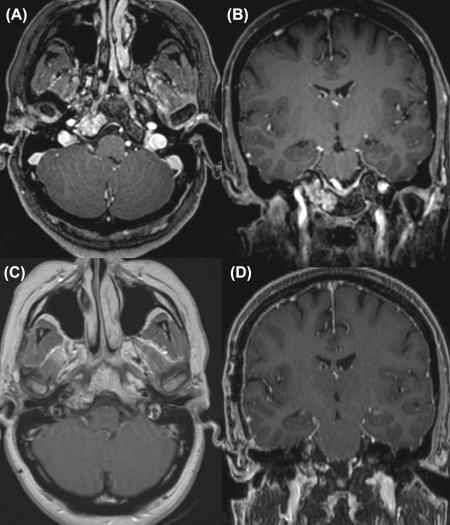
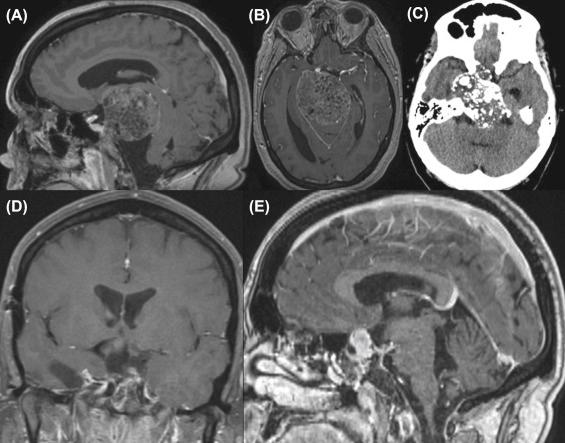
Chordomas and chondrosarcomas are rare skull base tumors, with an incidence of less than 0.03 per 100,000 persons. Although they have similar sites of origin, histologies (definitely distinguished only by immunohistochemical stain ), clinical presentations, and radiological features, they differ in natural history and clinical outcome. Surgical resection, with the aim of radical tumor removal, is recommended for most patients with skull base chordomas and chondrosarcomas. Although both tumors arise in the bone and infiltrate paths of least bony resistance until rupturing through the cortex and forming a mass in the soft tissue, chordomas originate in the midline and grow laterally in both directions, whereas chondrosarcomas arise laterally, from the petroclival syncohondrosis, and grow predominantly ipsilaterally. Because of this difference, surgical strategies differ. Chordomas commonly require multiple surgical exposures for radical resection [as depicted in illustrative cases 1 and 2 ( Figs. 20.3 and 20.4 )], as they frequently involve multiple anatomical areas inaccessible via only one approach. In contrast, chondrosarcomas, despite their frequent large size at the presentation, can be usually be removed by one operation ( Figs. 20.1 and 20.2 ). The surgeon who treats both types of tumor must master multiple skull base approaches. Also, each approach must be tailored to maximize exposure and facilitate dissection of tumor wherever it extends. The following anatomical classification based on the pattern of extension aids in the selection of surgical approach :
Type I: small, isolated (symptomatic or asymptomatic)—radical removal with bone margin in one surgical approach.
Type II: relatively large size in continuous areas—radical removal with only one surgical approach.
Type III: extending through the skull base—two or more skull base approaches to achieve radical removal.
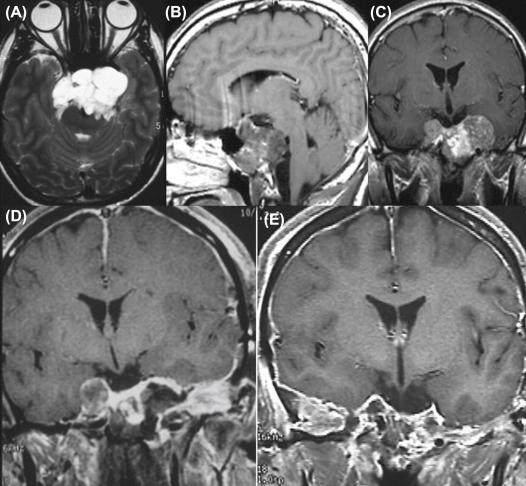
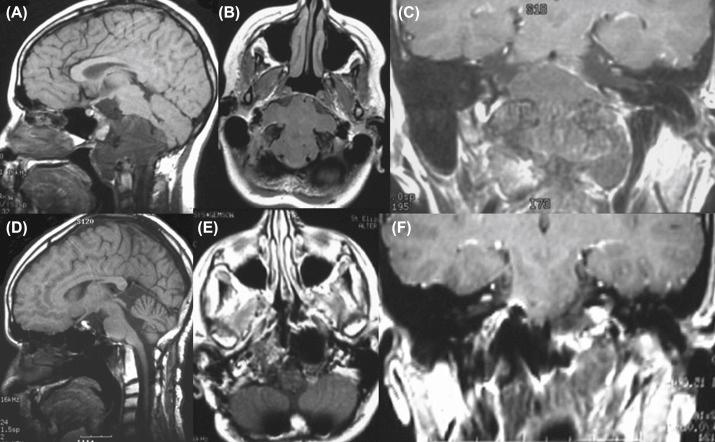
Dural invasion is another important consideration in the choice of operative approach. Direct dural invasion is a common pattern of extension, particularly of chordomas, and cavernous sinus invasion frequently arises from spread of the tumor along the sixth cranial nerve. All approaches first encounter the extradural tumor; any transdural extension is followed through the resulting dural defect to the intradural tumor. Primarily intradural cranial approaches should be avoided as the chordoma can be spread by the dispersion of cells in the cerebrospinal fluid (CSF). Tumor can also be seeded along the operative route and at donor sites for reconstruction ( Fig. 20.6 ). To minimize the former, before the tumor capsule is disrupted, the operative corridor wall is lined with cottonoids or other barrier material, contact of instrument with normal tissue is avoided, and the tips of the instruments are not touched by the surgical team. To avoid the last of these three, the fat or fascial graft is harvested from a totally separate, sterile field with clean instruments and a newly dressed surgical team. The instruments used in the main operation are considered to be tumor contaminated, as are the surgical drapes, towels, and gloves.
For almost all chordomas requiring multiple approaches, the anterior approach is performed first. Lateral extension often requires one or more lateral approaches, and inferolateral extension to the condyle may require a stabilizing occipitocervical fusion, which is often deferred to the final stage.
Recurrent cases present quite a challenge, particularly in reconstruction, in preventing CSF leakage (see Chapter 37 ). The challenge and risk increase markedly following radiation therapy, which promotes angiopathy that increases the risk of vascular injury. Extensive scarring from previous surgery and radiation may warrant the choice of an alternative approach. In this chapter, surgical strategies that include two or more approaches to achieve safe radical tumor removal will be discussed.
The anatomical localization and extension of these lesions warrant comprehensive clinical, ophthalmological, and endocrinological evaluations. Any symptoms, signs, or radiographic concern for lower cranial nerve dysfunction or involvement (cranial nerves IX, X, XI, and XII), such as swallowing difficulty or voice change, warrant formal assessment. Neuroimaging studies must include thin cuts of multiplanar magnetic resonance (MR) sequences with and without contrast and thin high-resolution computed tomographic (CT) scans with multiplanar axial, coronal, and sagittal reconstruction. Bone window CT is essential to understanding the destruction of surrounding bony structures and extension into the suprasellar, parasellar, and cavernous sinus regions, as well as the anterior, middle, and posterior fossae; the infratemporal fossa; petrous apex; foramen magnum; occipital condyle; air sinuses; and parapharyngeal spaces. Vascular imaging including both arterial and venous phases is obtained in all cases; vascular supply to the tumor and large vessel encasement or displacement should be noted in planning the surgical approach. Dynamic CT simultaneously depicts bony structure and cerebral vasculature. Cerebral angiograms an balloon test occlusion are rarely necessary, except in cases with high risk of carotid injury, such as a recurrent tumor extending into the cavernous sinus in a previously irradiated field ( Fig. 20.5 ).
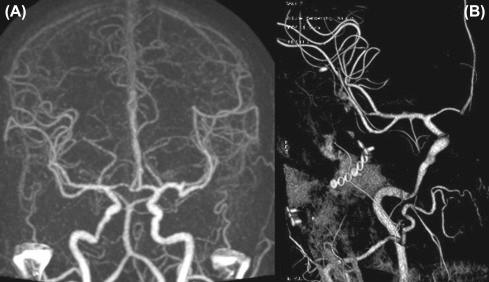

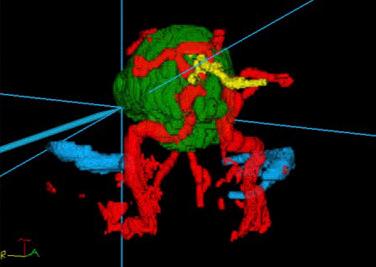
Stereotactic navigation, fixed or floating head, is used for intraoperative localization and to assess the extent of resection; segmentation aids depiction of the neurovascular structures displaced or encased by the tumor ( Fig. 20.7 ). The endoscope is routinely used, sometimes simultaneously and frequently alternating with the operating microscope, to visualize and remove tumor outside the view of the microscope ( Fig. 20.8 ). Intraoperative Doppler microultrasonography helps identify arteries and verify their permeability after manipulation. Intraoperative imaging with CT or MR may also be valuable ( Fig. 20.9 ). If they are not available, then immediate postoperative imaging should be performed to determine the extent of removal and the need for additional surgery.


Intraoperative neurophysiological monitoring of electroencephalographic patterns, somatosensory evoked potentials, auditory brainstem evoked potentials, and electromyography of cranial nerves III, IV, V, VI, VII, X, XI, and XII, as required by tumor extension, is essential and improves the surgical results. Anticipation of manipulation of the pituitary gland, which is often required, warrants administration of 100 mg of hydrocortisone at the beginning of surgery and subsequent tapering to any maintenance dose required postoperatively.
Harvey Cushing, in 1909 via a transsphenoidal route, was the first surgeon to successfully resect a chordoma; reoperation was performed a few months later for additional resection. The diagnosis of chordoma was made retrospectively by Bailey and Bagdasar in 1929. Subsequently, the routes for chordoma removal have expanded to include almost all skull base approaches (see Chapter 10 ). These can be grouped into two main categories: anterior and lateral. A combination of anterior and lateral approaches is recommended for type III tumors.
The anterior approaches provide the most direct trajectory to the clivus, thus allowing the surgeon to reach the tumor in a short time, with minimal bony and soft tissue dissection and limited manipulation or dissection of neural structures. Anterior approaches work along the most common direction (anterioposterior) of tumor growth and permit tumor removal with limited displacement and disruption of surrounding structures. Anterior approaches may be used in combination to expose clival lesions and include the following: transoral, transsphenoidal, transmaxillary, transfacial, and transbasal. Endoscopic techniques have fostered the trend toward less facial dissection.
Endoscopic surgery has flourished recently with applications beyond pituitary tumors as both the sole and a complementary visualization tool. The endoscope allows visualization of anatomy that would not be seen by the microscope without additional disruptive dissection. Its maneuverability, proximity to the field, and angled lenses can provide close-up, panoramic, although two-dimensional, views that include anatomy deep to structures that obscure the direct line of sight of the microscope. This better visualization can facilitate safer, more complete tumor resection. For instance, in removing the intradural component of a clival chordoma, 30 and/or 70 degree angled endoscopes permit visualization and removal of tumor peripheral to the dural opening.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here