Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On completion of this chapter, you should be able to:
Define high-risk pregnancy
Describe the maternal and fetal factors for a pregnancy that are considered high risk
Discuss the role of sonography in the high-risk pregnancy
A high-risk obstetric patient is one who has the potential for or is at an increased risk for an adverse maternal or fetal pregnancy outcome. At its extreme, adverse would mean maternal or fetal injury or death. When identifying the high-risk pregnant patient, both the mother and the fetus must be considered. Therefore, this chapter discusses both maternal and fetal high-risk factors.
Screening tests, as opposed to diagnostic tests, are offered to low-risk populations to identify patients whose risk is high enough for them to be offered diagnostic testing.
There are a variety of tests that can be offered in either the first or second trimester. The first-trimester screen is performed by looking for the pattern of biochemical markers associated with plasma protein A (PAPP-A) and free β-human chorionic gonadotropin (β-hCG). These laboratory values are used in conjunction with an ultrasound (performed between 11 and 14 weeks) to measure the nuchal translucency and the presence of the nasal bone. Based on the patient’s PAPP-A and free β-hCG laboratory values, age, nuchal translucency measurement, and the presence or absence of the nasal bone, a more accurate risk calculation can be made for having a child with a chromosomal abnormality, congenital heart defect, skeletal dysplasia, or other syndromes. To offer this screening, sonographers must become certified for first-trimester screening. This requires the sonographers performing the test to take an online course and pass a written test. Upon receiving a passing score, a minimum of three ultrasound evaluations of the nuchal translucency must be evaluated for compliance with the certifying organization before the sonographer is certified to perform the examination. This evaluation is repeated annually. Laboratories performing the first-trimester screen will only accept samples and data from certified sonographers. The advantage to parents with first-trimester screening is that they can evaluate their risk for having a child with a chromosomal or syndromatic abnormality much earlier in pregnancy. They may then choose to undergo additional testing, including noninvasive prenatal testing (NIPT) or invasive testing such as chorionic villus sampling (CVS) or amniocentesis to obtain tissue for chromosomal analysis. Cell-free DNA is an advanced screening NIPT with a much higher detection rate for Down syndrome and trisomy 18 (99%), and trisomy 13 (91%) than the first-trimester screen or the quad screen, which is performed in the second trimester. NIPT can be offered as early as 10 weeks, and because it can also screen for abnormalities with the sex chromosomes, such as Klinefelter syndrome (XXY), triple X syndrome (XXX), and Turner syndrome (XO), it can identify the fetal sex. This test evaluates the chromosomes from small pieces of fetal DNA found within a maternal blood sample. NIPT is usually combined with ultrasound evaluation of the nuchal translucency for additional accuracy. Although this test is currently offered to populations of pregnant women with a high risk of abnormal findings only, it holds promise for the future as an alternative to current screening and invasive testing.
Second-trimester screening can be performed with the maternal serum quad screen laboratory value and/or a detailed fetal anatomic survey ultrasound examination. The maternal serum quad screen looks at four serum markers: alpha-fetoprotein (AFP), hCG, unconjugated estriol (uE3), and inhibin-A. If a first-trimester screening was performed, it would not include the AFP testing so it may be recommended to be done as a single test to screen for neural tube defects in the second trimester.
The detailed fetal anatomic survey ultrasound is a detailed evaluation of specified fetal anatomy and biometry that can be seen at the time of examination. Most ultrasound departments prefer to perform a detailed fetal anatomic survey examination between 18 and 20 weeks of gestation. This time period is chosen because it often yields the best view of fetal anatomy based on size, and the accuracy of the dating biometry is within 10 to 14 days of the expected date of delivery. The detailed fetal anatomic survey ultrasound examination includes, but is not limited to, the evaluation of the anatomy shown in Table 54.1 .
| Component | Basic | Detailed |
|---|---|---|
| Head and neck |
|
|
| Face | Upper lip | |
| Chest | Cardiac activity | Aortic arch |
| Heart and thorax |
|
|
| Abdomen |
|
|
| Spine |
|
|
| Extremities |
|
|
| Genitalia |
|
Sex a |
| Placenta |
|
|
| Standard evaluation |
|
|
| Maternal anatomy |
|
|
| Biometry |
|
Based on the results of the screening maternal serum quad screen and the detailed fetal anatomic survey ultrasound, patients’ risk for having a child with a chromosomal anomaly or neural tube defect can be reassessed. Parents are counseled with this information and can then choose to have NIPT or a diagnostic amniocentesis to obtain fluid for chromosomal analysis, if desired.
By definition, advanced maternal age (AMA) describes a patient who will be 35 or older at the time of delivery. AMA can be an indicator for high-risk pregnancy. For example, the incidence of Down syndrome increases with age. The risk of a 35-year-old woman conceiving a fetus with Down syndrome is 1 in 294, but the risk rises to 1 in 40 at age 40 years. Maternal age alone, however, fails to detect approximately 66% of fetuses with Down syndrome because these babies are being born to younger women without known risk factors for chromosomal abnormalities. In the United States, it is now standard practice to offer AMA women genetic counseling, screening options, or invasive prenatal testing for karyotypic analysis. The American College of Obstetricians and Gynecologists (ACOG) guidelines recommend that maternal serum screening for neural tube defects and Down syndrome be offered to all women.
Hydrops fetalis is a condition in which excessive fluid accumulates within at least two fetal body cavities. This fluid accumulation may result in anasarca , ascites, pericardial effusion, pleural effusion, placental edema, and polyhydramnios. There are two classifications of fetal hydrops : immune hydrops and nonimmune hydrops (NIH). By ultrasound evaluation, both types are characterized by extensive accumulation of fluids in fetal tissues or body cavities. NIH is unrelated to the presence of maternal serum immunoglobulin G (IgG) antibody against one of the fetal blood cell antigens.
Blood group isoimmunization is diagnosed on routine antenatal laboratory evaluation, which tests for the presence of a variety of antibodies. Any significant antibodies are evaluated for strength of antibody response, which is reported in a titer format (i.e., 1:4, 1:16). If an antibody titer is detected, the pregnancy should be monitored.
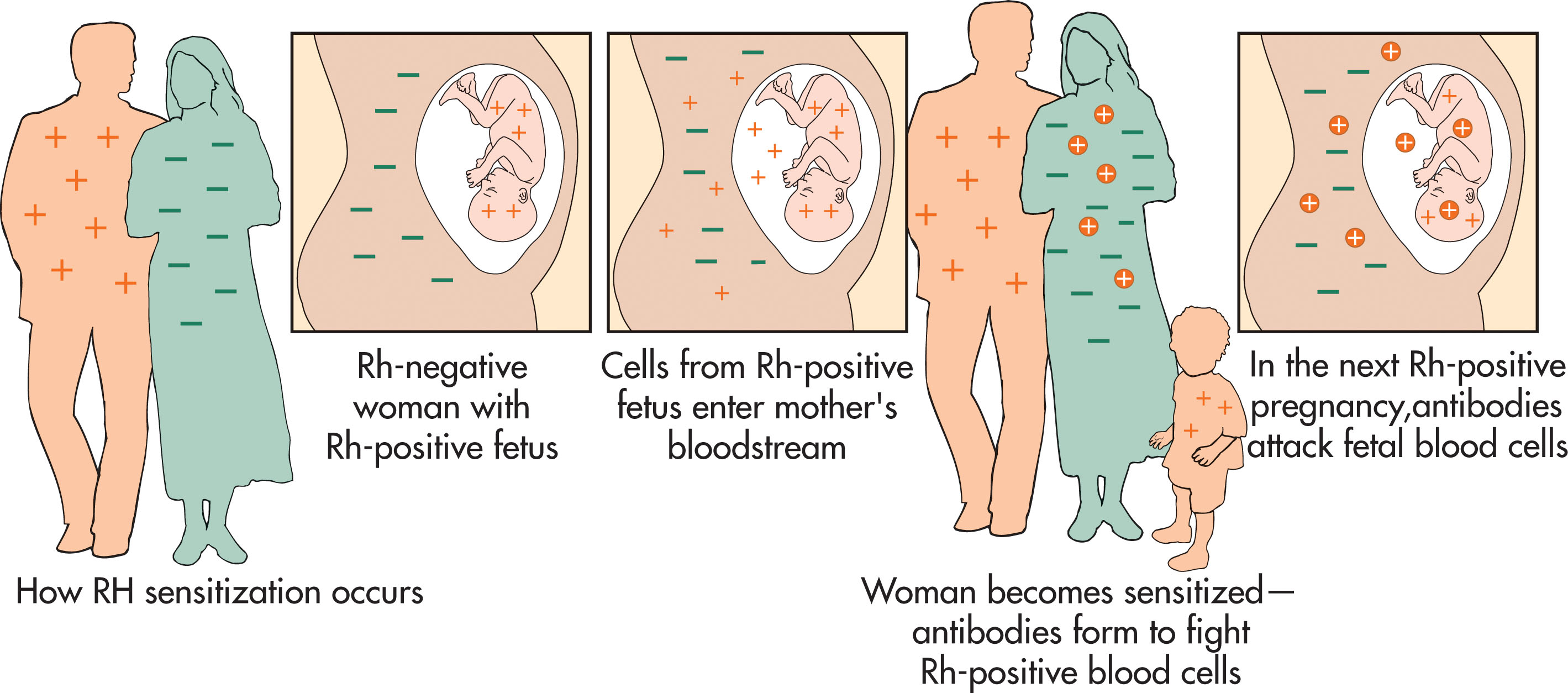
Immune hydrops is initiated by the presence of maternal serum IgG antibody against one of the fetal red blood cell (RBC) antigens in a process known as sensitization . An antigen is any substance that elicits an immunologic response such as the production of an antibody to that substance. In pregnancy, this can occur anytime a mother is exposed to RBC antigens different from her own. For example, if a father and fetus are Rh+ and a mother is Rh– and there is a maternal-fetal hemorrhage (mixing of blood), maternal antibodies can be produced against the Rh antigen. In subsequent pregnancies, these antibodies can pass through the placenta and destroy fetal blood cells, resulting in fetal anemia ( Fig. 54.1 ). Today, this condition is rare and can be prevented if RhoGAM is given any time there is potential mixing of the maternal and fetal circulation.
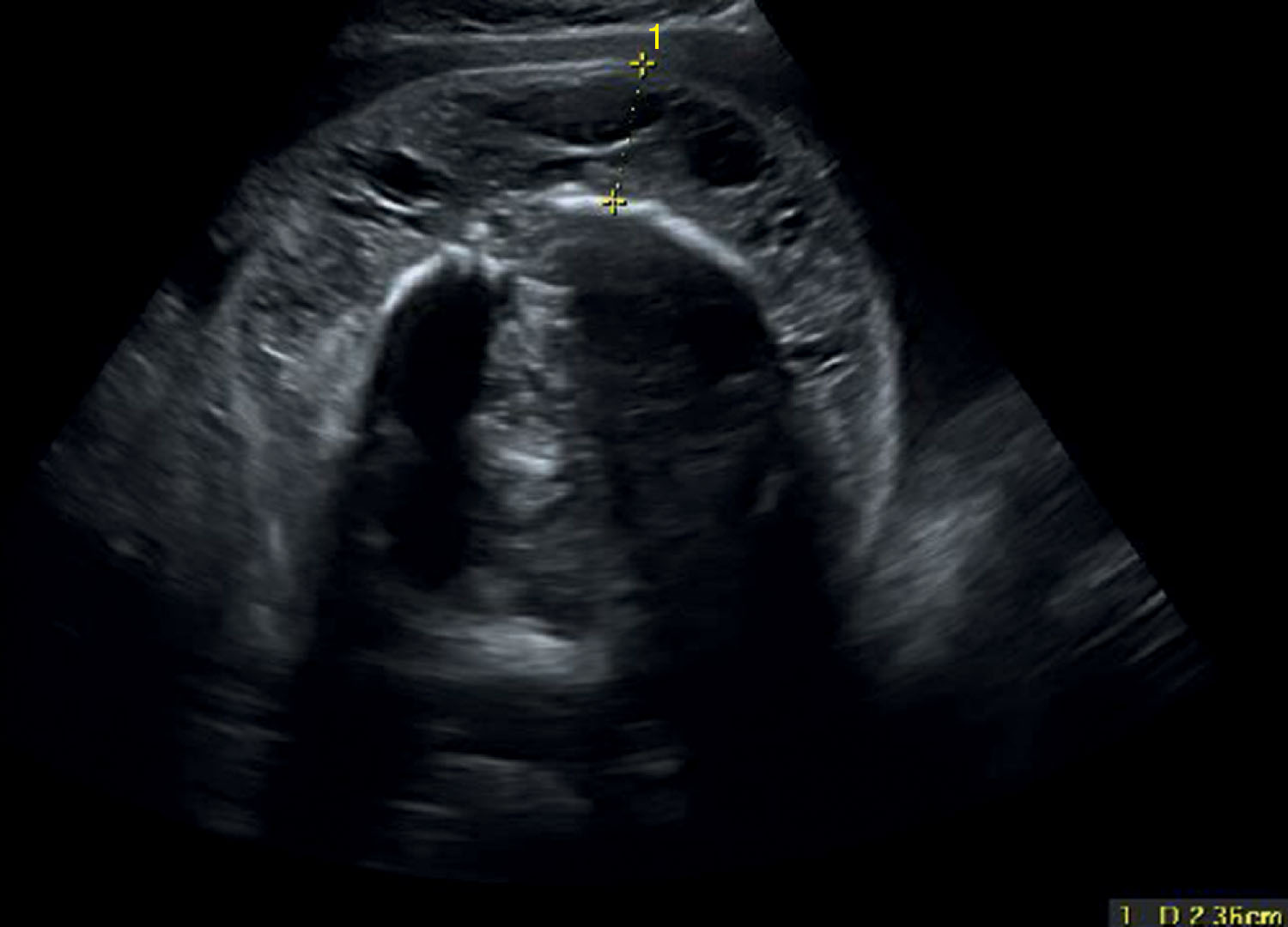
When a sensitized gravid uterus is not treated with RhoGAM, the mother develops an antibody called maternal IgG. This antibody is able to cross the maternal-fetal barrier and enter fetal circulation. It attaches to the fetal RBCs and destroys them in a process called hemolysis . Hemolysis can result in fetal anemia, leading to congestive heart failure and hydrops ( Fig. 54.2 ). The severity of fetal anemia can be determined by sonographic surveillance, amniocentesis, and cordocentesis.

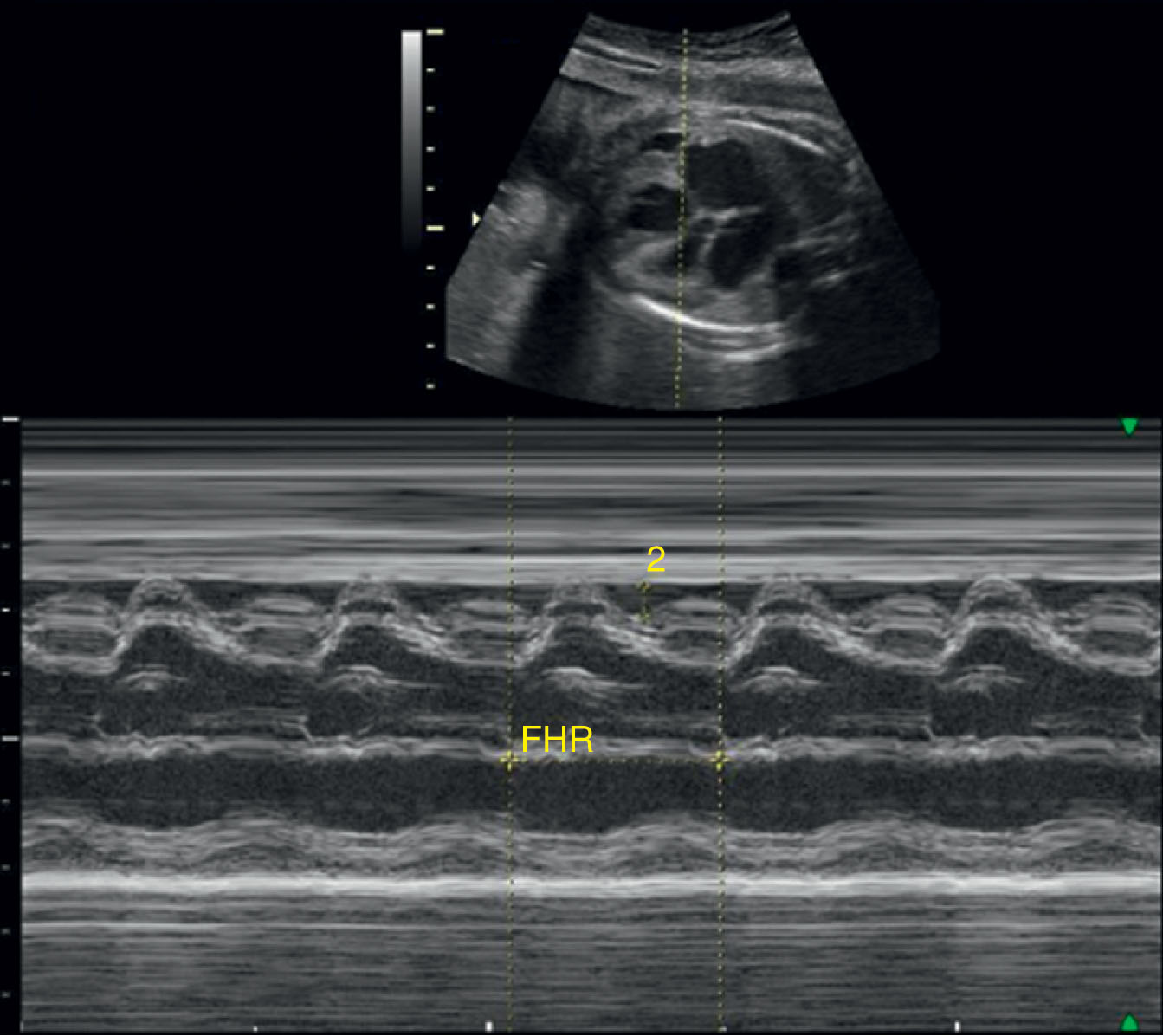
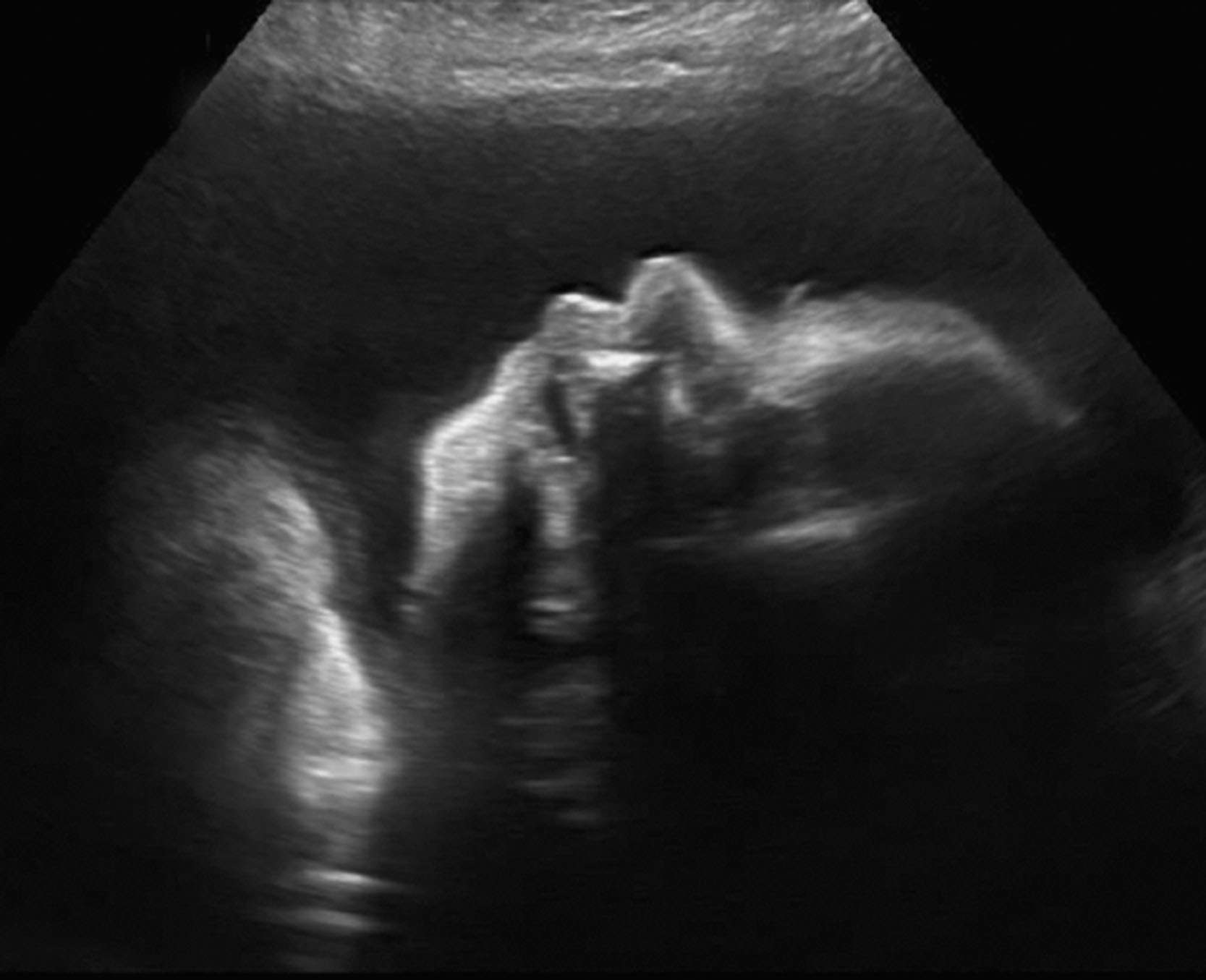
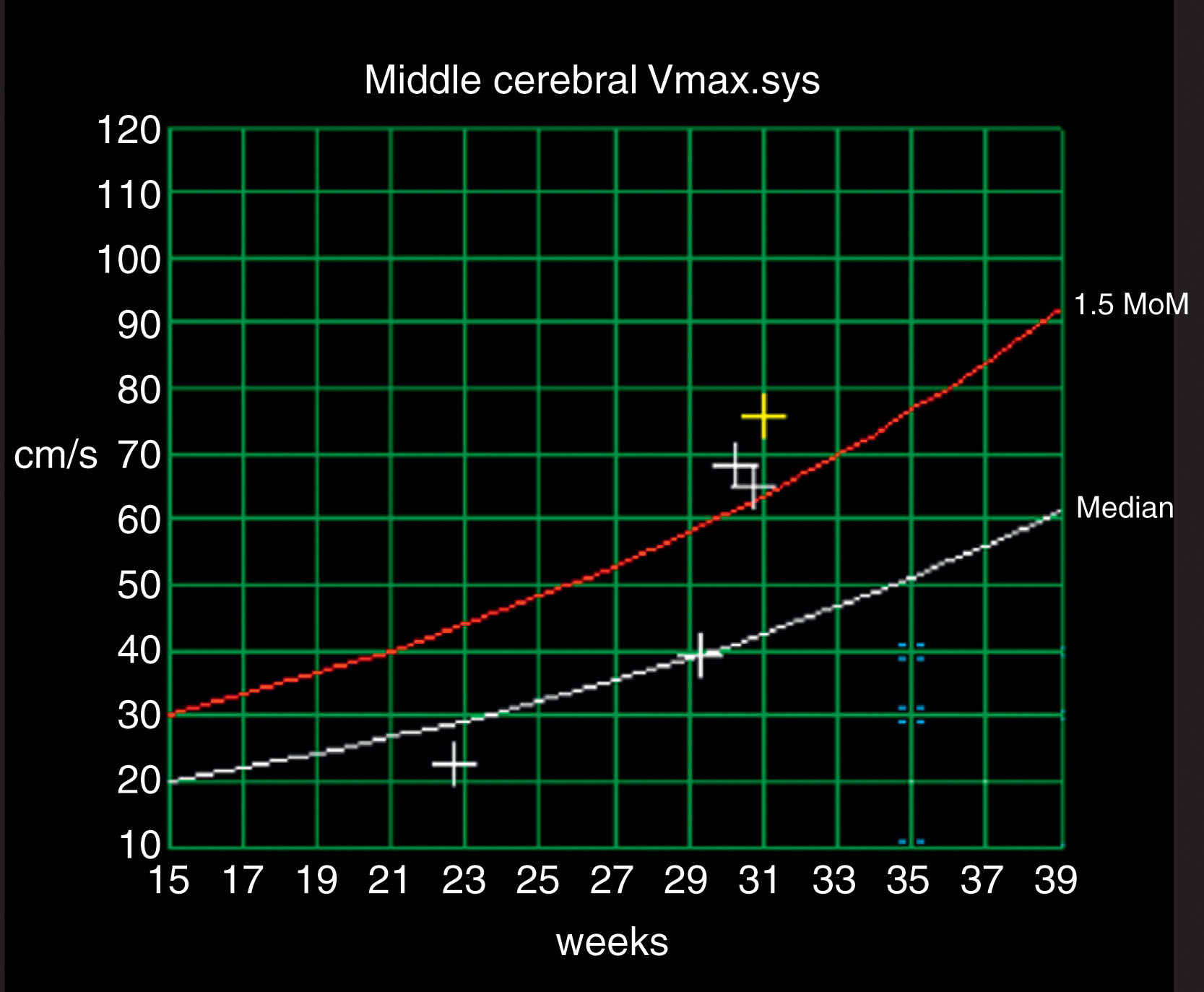
Sonographic surveillance for an isoimmunized pregnancy should include (but not be limited to) assessment for signs of hydrops. Sonographic findings of hydrops are scalp edema ( Fig. 54.3 ), pleural effusion ( Fig. 54.4 ), pericardial effusion, ascites ( Fig. 54.5 ), polyhydramnios ( Fig. 54.6 ), pericardial effusion ( Fig. 54.7 ), and thickened placenta. Hydrops can be due to fetal anemia. Another ultrasound tool available to predict fetal anemia is Doppler evaluation of the middle cerebral artery (MCA) ( Figs. 54.8 and 54.9 ). Because there are fewer RBCs with anemia, the viscosity of the blood is decreased. A decrease in viscosity results in a decrease in resistance to flow, which can be detected by an increase in velocity in the MCA. A peak systolic velocity of more than 1.5 multiples of the median is an indicator of severe fetal anemia and requires follow-up evaluation.


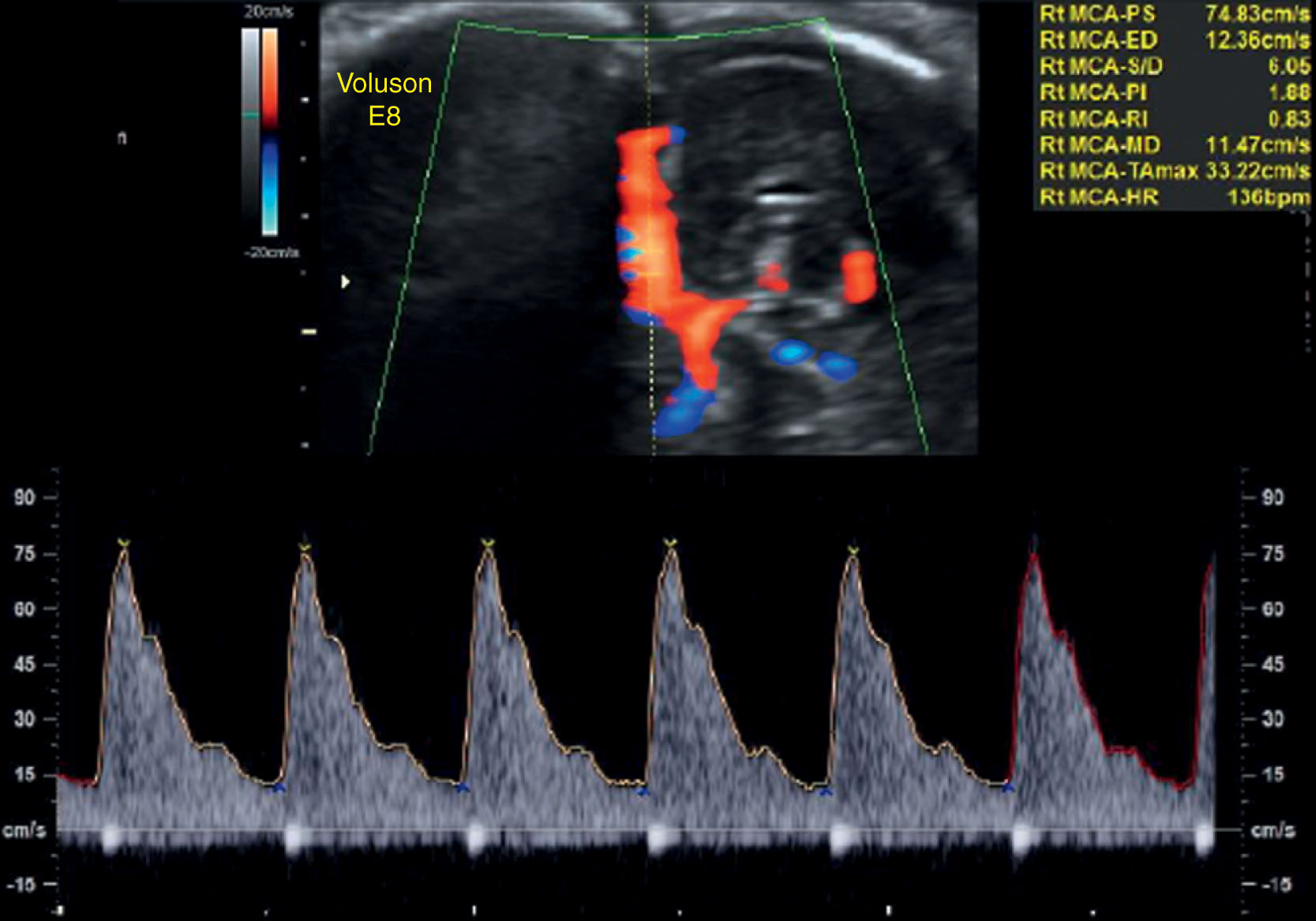
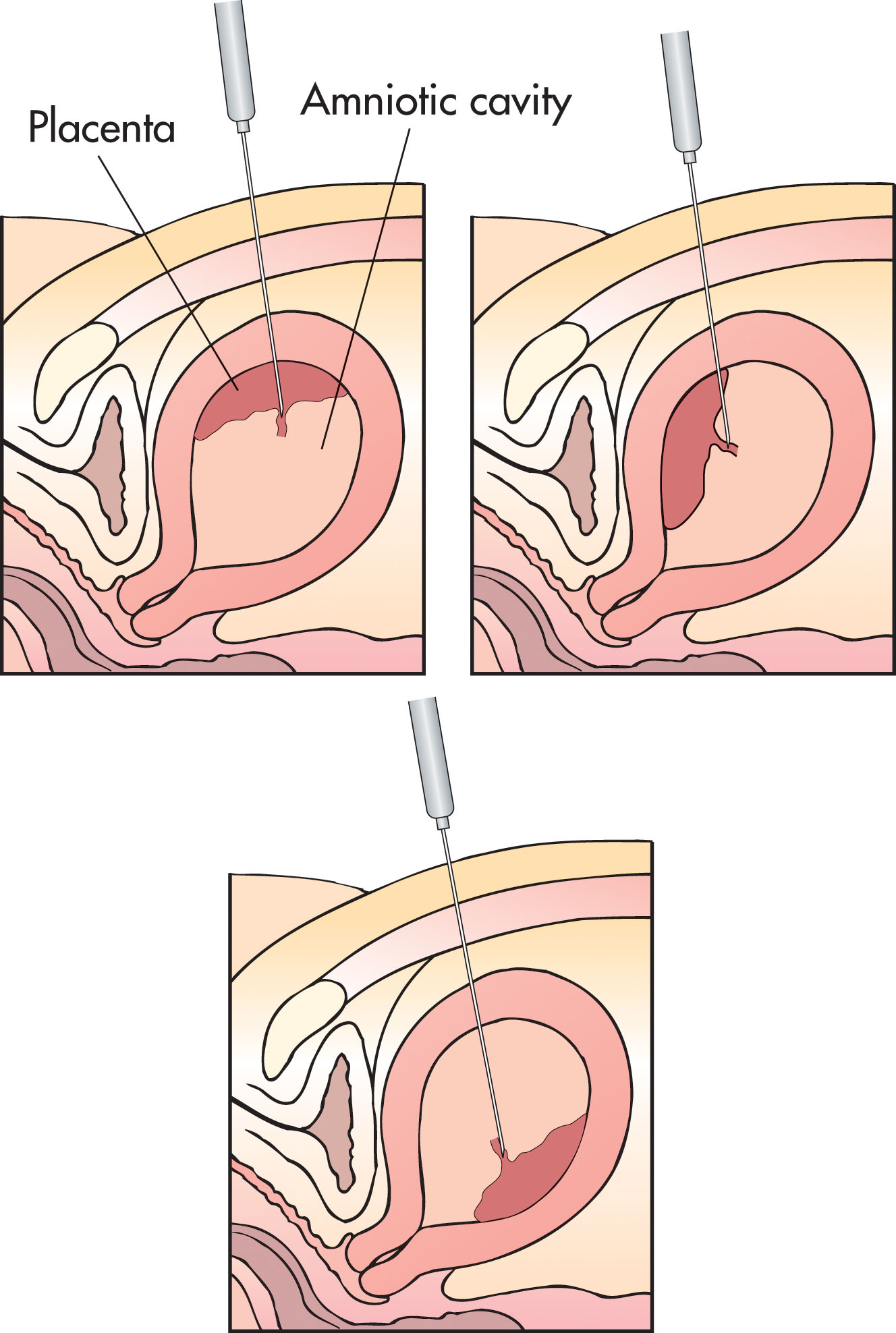
Cordocentesis is a procedure in which a needle is placed into the fetal umbilical vein to obtain a blood sample. The laboratory evaluates this sample for fetal blood type, hematocrit, and hemoglobin. If indicated, a fetal blood transfusion may be performed. There are two methods of transfusing a fetus. The first, intraperitoneal transfusion, uses ultrasound guidance to place a needle in the peritoneal cavity of the fetus. Blood is transfused into the peritoneal space where it is slowly absorbed by the fetus. The second method is direct intravascular transfusion via the umbilical vein (cordocentesis). Using ultrasound guidance, a fine needle is directed through the maternal abdomen toward the umbilical vein where it enters the placenta ( Figs. 54.10 and 54.11 ). RBCs are transfused directly into the umbilical vein. This method is preferred because a specimen of fetal blood can be obtained before transfusion to confirm that the fetus is truly anemic and isoimmunized. A specimen can be obtained after transfusion to document that the fetal hematocrit is adequate.

In a rare circumstance, a mother may develop an immune response to fetal platelets, much as one might develop an immune response to RBCs. When this occurs, she develops antibodies to the fetal platelets. The result can be a fetus with a dangerously low platelet count (thrombocytopenia). Infants born with this condition are at increased risk for intracerebral hemorrhage in utero and spontaneous bleeding. Cordocentesis is performed in these cases to document fetal platelet counts before vaginal delivery is attempted. Ultrasound can also be useful to look for evidence of in utero fetal intracerebral hemorrhage.
Nonimmune hydrops (NIH) describes a group of conditions in which hydrops is present in the fetus but is not a result of fetomaternal blood group incompatibility. Numerous fetal, maternal, and placental disorders are known to cause or be associated with NIH ( Box 54.1 ). The incidence of NIH is approximately 1 in 1700 to 1 in 3000 pregnancies, but NIH accounts for about 3% of fetal mortality. The exact mechanism for why it occurs is unclear, although the same processes described for the hydrops associated with Rh sensitization may apply to NIH.
Tachyarrhythmia
Complex dysrhythmia
Congenital heart block
Anatomic defects
Cardiomyopathy
Myocarditis
Intracardiac tumors
Trisomy 21
Turner syndrome
Other trisomies
XX/XY mosaicism
Triploidy
α-Thalassemia
Arteriovenous shunts
In utero closed-space hemorrhage
Glucose-6-phosphate deficiency
Obstructive uropathies
Congenital nephrosis
Prune-belly syndrome
Ureterocele
Diaphragmatic hernia
Cystic adenomatoid malformation of the lung
Tumors of the lung
Jejunal atresia
Midgut volvulus
Meconium peritonitis
Hepatic vascular malformations
Biliary atresia
Cytomegalovirus/parvovirus
Syphilis
Herpes simplex
Rubella
Toxoplasmosis congenital hepatitis parvovirus B19
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here