Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Upper endoscopy is an important diagnostic tool in the care of patients with gastrointestinal (GI) diseases. Unfortunately, there is a certain amount of discomfort and patient intolerance associated with unsedated procedures. For this reason, physicians are hesitant to use unsedated endoscopy as a first-line of investigation in patients with various GI problems, including gastroesophageal reflux disease (GERD). Thus, proton pump inhibitors are often used as a diagnostic test or for prolonged periods before proceeding to endoscopy. Different approaches have been proposed to improve patient tolerance during upper GI endoscopy. The most common and most widely used approach is intravenous sedation. Most patients wish to be sedated for upper endoscopy to avoid discomfort, but sedation introduces the need for numerous guidelines not otherwise required during endoscopy. Pre-, intra-, and postprocedure monitoring and assessment are required. Sedation related issues are responsible for up to 40% of the total endoscopic cost (cost of medication, cost of specialized nursing care, work loss) and one-half of the risk. Most patients would prefer to return quickly to normal activities as afforded by unsedated endoscopy. In some countries, general anesthesia is used broadly, which seems extreme for routine upper endoscopy. Less intensive approaches to sedation include premedication, topical anesthesia, and more anecdotal methods (such as ambient music), but they are less effective than intravenous sedation. The goal of all these methods is to reduce the patient's level of sensation, but they fail to modify the nature of the examination itself.
Transnasal introduction has been widely employed for bronchoscopy and laryngoscopy. With the advent of thinner endoscopes, transnasal esophagogastroduodenoscopy (EGD, or upper endoscopy) was originally considered an alternate option when transoral intubation was not possible for anatomical reasons. With time, transnasal intubation appeared to be a logical alternative to standard peroral EGD on a routine basis, as oral intubation of the esophagus is a major source of discomfort for patients. The transoral route induces protective glottal reflexes as the endoscope passes the base of the tongue and is swallowed. With the transnasal route, the patient does not swallow and does not have protective reflexes; patients can control their laryngeal motility and do not feel any sensation of asphyxia, as illustrated by the fact that they are able to talk during the procedure, further decreasing symptoms associated with anxiety.
In this chapter, we will discuss two major topics: tolerance and performance. This association is essential to allow transnasal endoscopy to expand and potentially replace conventional oral endoscopy in certain situations.
Since the first publications in the 1990s, studies concerning patient tolerance of unsedated transnasal endoscopy have shown conflicting results. The authors of one study observed that the overall assessment of patients regarding transnasal endoscopy is worse than with standard endoscopy, whereas another study concluded exactly the opposite. Patient tolerance of transnasal endoscopy is a major issue. The majority of published studies to date are in favor of the transnasal approach. One study of 20 volunteers noted significantly less risk of gagging and vomiting during transnasal insertion. Another evaluated 24 patients who underwent sequential transnasal EGD (5.3-mm diameter scope) followed by standard EGD. The transnasal group had less choking, sore throat, discomfort, and a higher rate of acceptability than the peroral group. A randomized study with 181 patients found tolerance was better with transnasal EGD (5.3-mm diameter) compared to conventional, peroral EGD. This study found that only 3% of patients undergoing transnasal endoscopy desired sedation on a future exam versus 15% in the peroral group. Another study that enrolled 60 patients observed that patients undergoing transnasal endoscopy (5.3-mm diameter) rated the procedure only slightly less comfortable than those undergoing sedated conventional endoscopy. Unsedated transnasal endoscopy was associated with significantly less procedure and recovery room time. One researcher placed 150 patients into three groups to elucidate the respective effect of the nasal route versus the small endoscope diameter on the patient's level of tolerance. One group had an oral route with a 9.8-mm diameter endoscope, the second group had an oral route with a 5.9-mm diameter endoscope, and the third group had a transnasal route (5.9 mm). They found less choking and nausea in the transnasal route group and therefore concluded that the tolerance was dependent on the route and not the endoscope diameter. A similar study was conducted on 150 patients. The authors observed that an ultrathin instrument was better tolerated and required less sedation than conventional endoscopes. Whereas the transnasal route caused less gagging than the peroral route, the tolerance was more dependent on the diameter of the endoscope than on the route of passage. This was demonstrated by the improvement noted with transnasal scopes with only two-way tip deflection, which have a reduction in diameter from 5.5 mm (four-way tip deflection) to 4.9 mm. Finally, a comparative prospective study demonstrated that improved tolerance and less nasal pain was associated with the use of smaller diameter endoscopes when transnasal access was utilized. An example of a transnasal procedure is presented in .
Four randomized studies have compared the nasal route and the oral route using ultrathin endoscopes. One study used 5.3-mm and 5.9-mm diameter endoscopes in 170 unsedated patients. The authors found the tolerance similar in the two groups. In contrast, another author demonstrated better tolerance with a 4.9-mm two-way tip deflection scope versus a 5.5-mm nasal scope. One researcher enrolled 60 patients in a study comparing the unsedated transnasal and peroral routes using a 6-mm endoscope for both routes. Overall, tolerance was similar in both groups. The main difference found was that the transnasal group had significantly more nasal pain on insertion and thus 85% of the patients in the transoral group versus only 69% in the transnasal group were willing to undergo unsedated endoscopy in the future ( p = 0.07). In the fourth study, researchers randomized 260 patients undergoing EGD to have it performed with an ultrathin transnasal (6-mm videoendoscope), an ultrathin oral (6-mm videoendoscope), or standard endoscope (9.6-mm videoendoscope). The study results were not in favor of the transnasal route; the overall assessment was better for standard EGD. However, gagging was reduced in transnasal endoscopy. Of note, it is often gagging that makes oral intubation difficult, thus necessitating increased sedation. It is therefore important to note that all these studies have noted less gagging with the transnasal approach.
Optimal preparation of the patient is a key factor in achieving improved tolerance. First, a topical anesthetic (lidocaine) has to be administered with pledgets or by spraying deeply within the nostrils at least 5 minutes prior to endoscope insertion. Second, a topical vasoconstricting agent (naphazoline) should be administered as an adjunct to the anesthetic drug to enlarge the nasal passages. Finally, a pharyngeal local anesthetic should be administered at the same time. However, these preparation factors likely do not explain the differences observed. In fact, it is likely that the endoscopists themselves have a large influence on patient preferences. The method of presentation and explanation of the study, as well as the way the questionnaire is obtained, are probably decisive factors (e.g., in one study, patients were questioned by an assistant nurse who did not attend the endoscopy procedure), and the opinions of the patients could reflect the opinions of the endoscopists. Additionally, if patients are questioned after some time has elapsed since the procedure, their responses may change. The manner in which the patients are recruited may also explain the mixed results, and education is also an important factor. At some institutions, transnasal endoscopy has become the initial approach to EGD, and all patients receive transnasal endoscopy as the initial method of upper endoscopy. Patient age does not seem to affect tolerance of transnasal endoscopy, as demonstrated in a comparative study between young and older patients. In a recent meta-analysis including 6659 patients, the technical success of transnasal endoscopy was slightly reduced compared to transoral (−2% lower) but tolerance was significantly improved, with 63% of patients preferring transnasal endoscopy to oral endoscopy.
Several studies highlight the trade-off between the potential improved tolerance of transnasal endoscopy and the concomitant loss of diagnostic accuracy. One issue is the higher rate of failure to pass the endoscope into the second portion of the duodenum via a transnasal approach. These technical problems are related to the smaller scope diameter and increased flexibility. In one study, the failure rate was 18% with transnasal endoscopy versus 3% for peroral endoscopy. A higher transnasal failure rate was also found in a second study. The failure to intubate the duodenum via the transnasal route is due to a combination of factors. First, endoscopists are less familiar with this approach, as they are traditionally taught the peroral method. However, the technical success of transnasal endoscopy can be quickly improved with a rapid self-learning curve for experienced endoscopists. Second, due to its more flexible nature, looping occurs frequently in transnasal endoscopy, often making it impossible to reach the second duodenum. The final and likely most important factor is the size of the nasal passage compared to the oral passage. It is the diameter of the endoscope (5.3 mm vs. 5.9 mm) that accounts for the significantly higher proportion of failures (8 of 41 vs. 2 of 43 for the 5.9- vs. 5.3-mm scope, respectively). The larger diameter also accounted for the significantly higher proportion of epistaxis (12 of 33 vs. 4 of 41). The difference in diameter of the 5.3-mm fiberscope versus the 5.9-mm videoscope may account for the differing results seen in published studies. Similar results were demonstrated using a 4.9-mm endoscope compared to a 5.9-mm two-way tip deflection transnasal scope (Olympus, Tokyo, Japan), with a 97.6% success rate for the 4.9-mm scope versus an 88.8% success rate for the 5.9-mm scope ( p < 0.05). A meta-analysis has demonstrated the effectiveness of transnasal endoscopy, with a 95% technical success rate versus a 97.8% rate with the transoral route (difference: −2%, confidence interval [CI] −4% to −1%); however, this difference was not significant if a smaller endoscope (< 5.9 mm) was used (difference: −1%, CI −3% to 0.9%).
In two studies comparing the transnasal and transoral technique, the examination time was 2 minutes longer in the transnasal group than in the transoral group, but this was not observed in a third study. The reason for these differing results is ambiguous and the previously discussed meta-analysis did not analyze procedure time. On one hand, the transnasal approach could be longer, as suctioning of the gastric juice is more difficult and analysis of the mucosa is more challenging. Improved endoscope maneuverability using four-way 5.5-mm diameter endoscopes reduces procedure duration compared to two-way angulation 4.9-mm endoscopes in gastric cancer screening. This difference may also be explained, however, by improved patient tolerance via the transnasal route that permits a more comfortable and thus longer analysis of the mucosa, especially within the stomach, whereas with the transoral route, the operator may perform an expedited exam to reduce discomfort.
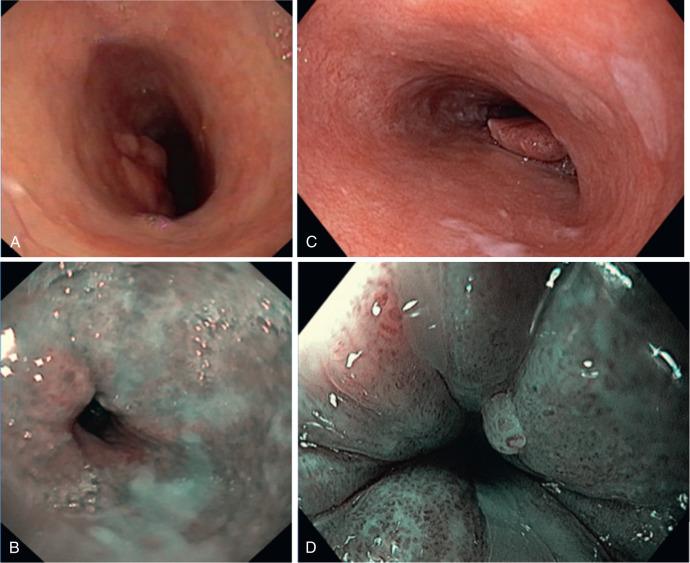
Despite the improved patient tolerance with the unsedated transnasal approach, decreased optical quality has been observed with the thin, 5.3-mm fiberoptic scope ( Fig. 11.1 ). This may lead to missed lesions. The authors of one study noted a sensitivity of 89% for the transnasal approach, and in another study using the ultrathin endoscope, 5 out of 59 endoscopic findings that were identified on standard endoscopy were missed. Due to the smaller channels, the air/water and suction were suboptimal when compared to present conventional upper endoscopes. Sacrificing optimal visualization for a small diameter is a challenging trade-off. Recently, image quality has been dramatically improved in transnasal video endoscopes with virtual chromoendoscopy (such as narrow band imaging [NBI; Olympus] and FUJI Intelligent Chromo Endoscopy [FICE; Fujinon, Fujifilm Medical Co., Saitama, Japan]). Nevertheless, transnasal endoscopy is typically used for evaluating upper GI symptoms, suspected portal hypertension, and screening for Barrett's esophagus ( Fig. 11.2 ), but not for the precise examination of preneoplastic lesions, for which upper GI scopes with zoom capability are preferred (see Fig. 11.1 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here