Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Understanding and recognition of sex-based differences, with respect to both normal cardiac electrophysiology and the pathophysiology of arrhythmias, are important for the diagnosis and treatment of heart rhythm disorders in women. There are cellular and clinical electrophysiologic differences that have been identified between men and women. Although genetics and the sex hormones partially explain the morphologic differences in cardiovascular systems, there is limited understanding of the mechanisms of the sex-specific variations in cardiac electrophysiology. This chapter reviews current knowledge of sex differences in cellular and clinical electrophysiology, including the incidence and prevalence of arrhythmias, in addition to the clinical presentation and prognosis of rhythm disorders.
Since the observation of higher resting heart rates (HRs) and longer rate-corrected QT (QTc) intervals in women by Bazett a century ago, sex differences in the electrical properties of cardiomyocytes and the myocardial conduction system have been extensively studied. As summarized here, sex-based differences in clinical arrhythmias could potentially be explained by changes in ion channel function, expression patterns, ionic currents, action potential (AP) morphology, intercellular conduction, autonomic tone, and hemodynamics and by the effects of sex hormones and genetics.
Differences between female and male cardiomyocyte electrical properties have been documented in various species, including humans. In addition to genetics and sex hormones, many factors modify cardiomyocyte structure, cardiomyocyte function, ionic currents, and AP morphology. These factors determine susceptibility to arrhythmias by affecting the depolarization and repolarization process and by causing changes in conduction intervals. Sex-based differences in clinical arrhythmias are essentially based on these cellular dissimilarities.
Sex-based differences in function, structure, quantity, and currents of cardiomyocyte ion channels, including sodium (Na + ), potassium (K + ), and calcium (Ca 2+ ) channels and their components, have been defined ( Fig. 107.1 ). Sex hormones affect Na + channel function and the transmural distribution of Na + channel current (I Na ). In the canine left ventricle (LV), I Na amplitude is smaller in female epicardial and endocardial layers. In rabbit atria, there is a large difference in late I Na current in male and female cardiomyocytes. Nonhomogeneous transmural dispersion of I Na increases the risk for ventricular arrhythmias in females. In castrated male dog hearts, I Na amplitudes are similar to those in female hearts.
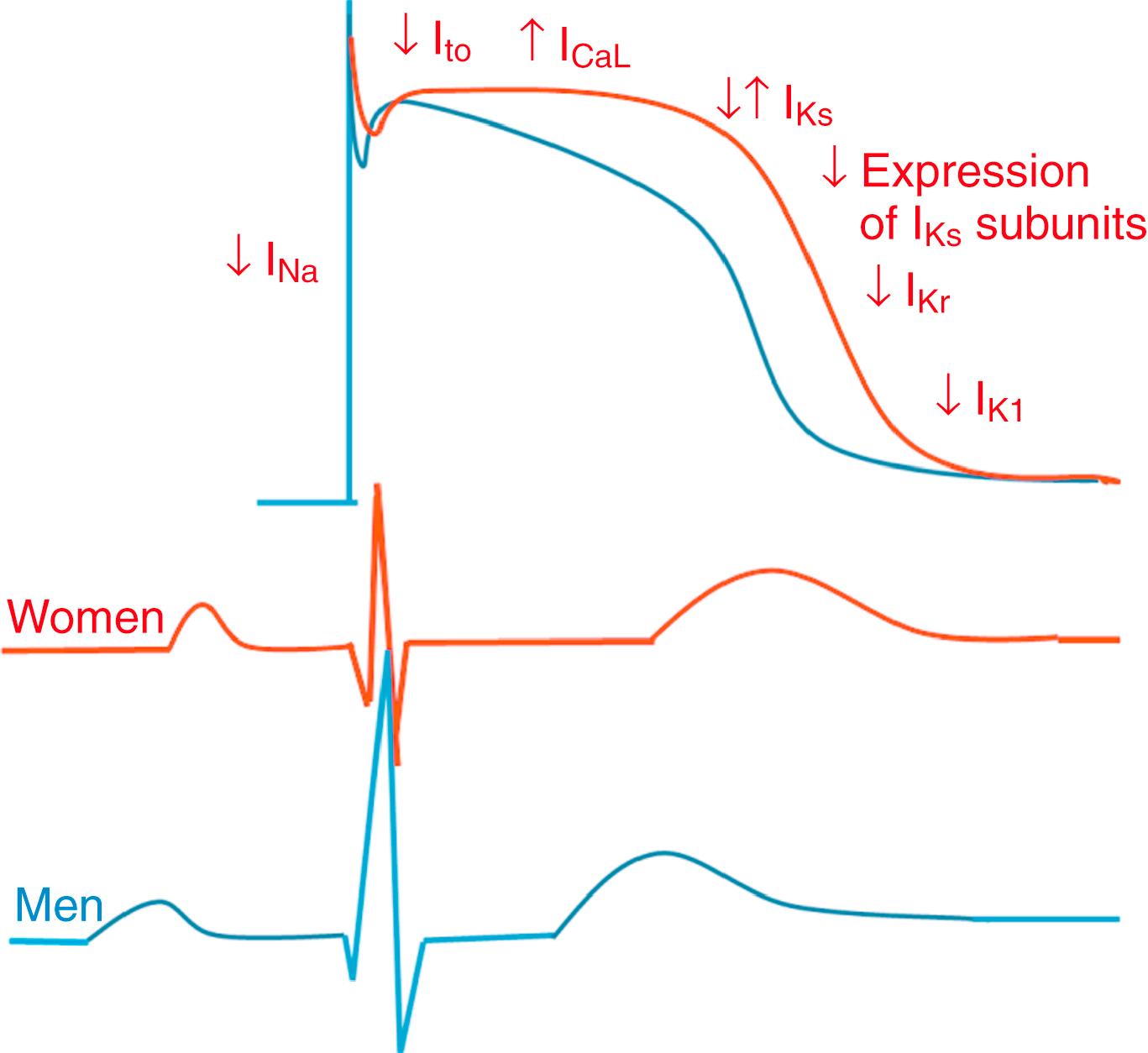
A study on healthy human transplant donor hearts showed reduced expression of a variety of delayed rectifier K + currents (I K ) subunits, including hERG, MinK, K ir 2.3, K V 1.4, KChIP2, SUR2, and K ir 6.2, in women compared with that in men. In female mouse hearts, total I K , transient outward K + current (I to ) and slow delayed rectifier K + current (I Ks ) densities are lower in a higher estrogen state, reflecting a direct effect of estrogen on K + currents. This lower current density is associated with downregulation of K V 4.3 and K V 1.5 transcript levels. In female canine ventricles, total densities of I to , I Ks , and L-type Ca 2+ (I CaL ) currents are different and lead to transmural variation in cardiac repolarization. This finding is species dependent. In guinea pig hearts, expression levels of the different K + channels are similar in both sexes. Larger I CaL currents are present in all layers of female canine ventricles compared with those in males. The required Ca 2+ for maximum contractile force is significantly lower in males. Cellular Ca 2+ transients have been measured in rat epicardial myocytes. Ca 2+ reuptake was smaller in magnitude and longer in duration, with greater local variability, in females. The rate sensitivity of Ca 2+ alternans was higher in females without significant heterogeneity in cellular responses.
The morphology of the cardiac AP plays an important role in the genesis of arrhythmias. The depolarizing inward and repolarizing outward ionic currents, intracellular ion concentrations, transmembrane potentials, and expression of ion channels determine AP morphology and the electrophysiologic properties of cardiomyocytes, and they are different in women compared with men (see Fig. 107.1 ). AP duration is longer in female ventricles than in male ventricles in various species, including humans (see Fig. 107.1 ). , , Ventricular cardiomyocytes in women have a longer AP duration, larger transmural heterogeneity of AP duration, and greater susceptibility to proarrhythmic early afterdepolarizations (EADs) than men. On the other hand, male cells have more prominent phase 1 repolarization and greater susceptibility to all-or-none repolarization. These differences are associated with altered I CaL , I to , and I Kr densities. Female sex hormones cause prolongation of AP duration. In one study, however, elevated estradiol levels were associated with enhanced KCNH2 membrane trafficking and shorter QTc intervals in healthy women. Slower restitution properties and repolarization alternans have been noted in female rat cardiomyocytes at slower HRs. Underlying ionic mechanisms of rate-dependent changes in AP morphology include variations in I to and I Ks in AP restitution and in I CaL and Na + -K + pump current (I NaK ) in AP accommodation. Transmural dispersion of cardiac repolarization is associated with I to , I Ks , and I CaL currents. Female M cells have longer AP durations with increased transmural heterogeneity.
Sex-based differences in baseline electrocardiographic (ECG) intervals and HR are summarized in Table 107.1 . Conduction intervals, as well as P wave and QRS morphology, have been noted to be different in men and women (see Fig. 107.1 and Table 107.1 ). Women have shorter PR intervals, QRS and P wave durations, and RR intervals than men but have longer QTc intervals. , P wave amplitude is greater in women than in men of all ages. The differences in PR interval and P wave duration progressively increase with aging, whereas P wave amplitude progressively decreases in both sexes with aging. The QRS complex is shorter in duration and lower in R wave amplitude in women after adjustment for LV mass and body weight. Thus the diagnostic accuracy of ECG criteria for LV hypertrophy is significantly lower in women than in men.
| Parameters | Women | Men | Reference |
|---|---|---|---|
| PR interval (ms) | 155 ± 24 | 163 ± 27 | 10 |
| P wave duration (ms) | 108 ± 12 | 111 ± 12 | 10 |
| P wave amplitude (μv) | 140 ± 45 | 131 ± 41 | 11 |
| QRS duration (ms) | 91 ± 13 | 98 ± 15 | 10 |
| QRS axis | 31 ± 35 | 26 ± 40 | 10 |
| R wave amplitude (μV) | 450 ± 334 | 480 ± 365 | 12 |
| QTc (ms) | 418 ± 24 | 406 ± 26 | 10 |
| QT-dispersion (ms) | 30 ± 11 | 37 ± 13 | 15 |
| Heart rate (beats/min) | 69 ± 12 | 67 ± 13 | 10 |
| Heart rate variability | Lower | Higher | 17 |
| Sinus node recovery time | Shorter | Longer | 18 |
| Atrial-His (AH) interval | Shorter | Longer | 19 |
| His-ventricular (HV) interval | Shorter | Longer | 19 |
| Atrioventricular (AV) block CL | Shorter | Longer | 20 |
| Slow pathway ERP | Shorter | Longer | 20 |
| AV nodal reentrant tachycardia CL | Shorter | Longer | 20 |
| Fast pathway ERP | Similar | Similar | 20 |
| Anterograde fast pathway ERP | Shorter | Longer | 21 |
| AV block CL | Shorter | Longer | 21 |
| Retrograde ventriculoatrial (VA) conduction | Longer | Shorter | 21 |
| Atrial ERP | Shorter | Longer | 18 |
| Ventricular ERP | Longer | Shorter | 20 |
Adult women have longer QTc intervals than men (see Fig. 107.1 and Table 107.1 ). QT prolongation is associated with sex hormones. , , During childhood, QTc intervals are similar in boys and girls, but they shorten in boys at puberty. Among adults, men with higher testosterone levels continue to have shorter QTc intervals than women. Athletes who take large doses of anabolic steroids have shorter QTc intervals too. In parallel, women with virilization syndromes have shorter QTc intervals than castrated men and healthy women. After the age of 65 years, QTc gradually increases in men and becomes comparable with that in women. Hormone replacement therapy, however, does not have an effect on the QTc intervals of postmenopausal women. Thus, compared with estrogen, testosterone modulates QTc more effectively. Significant seasonal variation in QTc intervals has been found among adult men but not in women. QT dispersion is greater in men than in women and demonstrates prominent circadian variation. Data derived from the Women’s Health Initiative Study show that nonspecific repolarization changes are more frequent in women and predict cardiovascular events. Repolarization inhomogeneity, as reflected in variations in the mean RR intervals and beat-to-beat QT intervals in an established time domain, is higher in women. Women adapt the QT interval to changes in RR interval faster than men. The QT/RR relationship is steeper and more curved in women.
Mean HR at rest is higher in women than in men by 2 to 6 beats/min. , This difference persists even after sympathetic and parasympathetic blockade, and it may be related to gender differences in exercise capacity, sex differences in HR and HR variability fluctuate on the basis of age, race, physical conditioning, and comorbidities. HR variability is a known sensitive index of cardiac autonomic regulation. It is greater in men than in women in the age range of 33 to 47 years. Men have higher values of frequency-domain parameters of HR variability (low-frequency power and total power) in the supine and standing positions. High-frequency power, however, is similar in both sexes. With autonomic blockade, atrioventricular (AV) nodal refractoriness and conduction time become shorter in women, and QT and JT duration and the refractory period of the right ventricle become shorter in men.
Intracardiac electrophysiologic measurements in men and women have demonstrated fundamental differences in the electrical properties of the heart, including sinus node function, AV conduction, and atrial and ventricular myocardium (see Table 107.1 ). Sinus node recovery time is significantly shorter in women than in age-matched men with structurally normal hearts. , Similarly, corrected sinus node recovery time remains shorter in young and adult women than in men.
AV conduction properties are also different in women, as reflected by shorter PR, atrial-His (AH), and His-ventricular (HV) intervals, as well as shorter AV block cycle lengths. Overall, men develop AV block more often than women. The incidence of dual AV nodal pathways is similar in both sexes, but women with symptomatic AV nodal reentrant tachycardia (AVNRT) have shorter slow pathway effective refractory periods (ERPs) and tachycardia cycle lengths than men. , The anterograde fast pathway ERP has been found to be similar to or shorter in women than that in men. During ventricular pacing in the absence of pharmacologic stimulation, women more often have ventriculoatrial (VA) conduction; men are more likely to exhibit VA dissociation. Also, women have shorter atrial ERPs but longer ventricular ERPs than men. The atrial ERP is similarly shorter in girls without structural heart disease than in age-matched boys. , ,
Women are more frequently affected by sick sinus syndrome, sinus tachycardia, inappropriate sinus tachycardia, postural orthostatic tachycardia syndrome, and sinus node reentry tachycardia than men. On the other hand, carotid sinus syndrome occurs more often in men ( Table 107.2 ). Inappropriate sinus tachycardia is diagnosed much more often in women younger than 40 years. Abnormal autonomic regulation of the sinus node or a related immunologic disorder involving cardiac β-adrenergic receptors has been speculated to be the cause of this condition in women.
| Supraventricular Arrhythmias | Ventricular Arrhythmias |
|---|---|
| Sinus node dysfunction: W > M | Left ventricular outflow tract ventricular arrhythmia: W < M |
| Carotid sinus syndrome: W < M | Verapamil-sensitive fascicular ventricular tachycardia: W < M |
| Inappropriate sinus tachycardia: W > M | Right ventricular outflow tract ventricular arrhythmia: W > M |
| Atrioventricular block: W < M | Sudden cardiac death: W < M |
| Atrial fibrillation: W < M | Long QT syndrome (acquired or congenital): W > M |
| Atrial flutter: W < M | Brugada syndrome: W < M |
| Atrioventricular nodal reentrant tachycardia: W > M | Arrhythmogenic right ventricular cardiomyopathy: W < M |
| Atrioventricular reentrant tachycardia: W < M | Catecholaminergic polymorphic ventricular tachycardia: W < M |
| Atrial tachycardia: W = M | Short QT syndrome: W < M |
| Paroxysmal atrial tachycardia: W > M | Early repolarization and idiopathic ventricular fibrillation: W < M |
| Incessant atrial tachycardia: W < M | Syncope: W = M |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here