Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
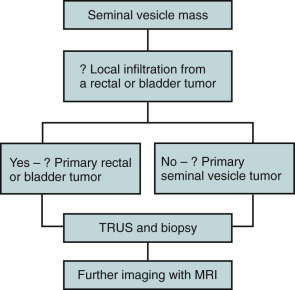
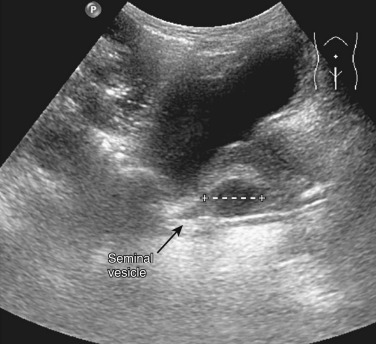
Traditionally, the seminal vesicles were evaluated with seminal vesiculography. This has largely been replaced by computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound ( Figure 74-1 ).
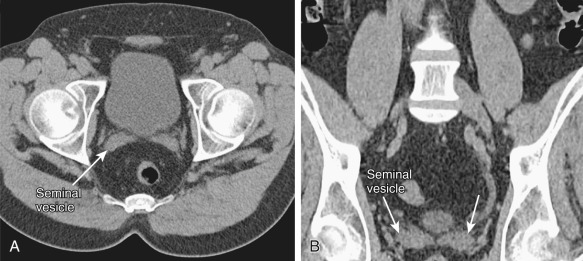
The seminal vesicles are of soft tissue attenuation ( Figure 74-2 ). Cysts and small masses that do not deform the seminal vesicle are not well seen. Large masses or inflammatory change associated with infection or abscess can be appreciated. Calcification is clearly seen.
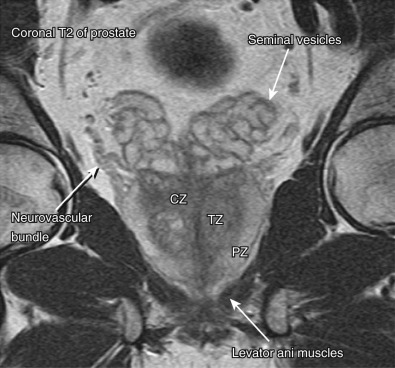
MRI is a valuable tool in evaluating the seminal vesicles owing to its multiplanar imaging capabilities and superb soft tissue contrast resolution ( Figure 74-3 ). It clearly demonstrates cystic lesions and is more accurate for staging of solid neoplasms than CT or ultrasound.
Transrectal ultrasound (TRUS) is rapid, inexpensive, and generally well tolerated. It is superior to CT because it better delineates the internal structure of the seminal vesicles. It also does not require the administration of ionizing radiation and can be used to guide seminal vesicle biopsy or aspiration.
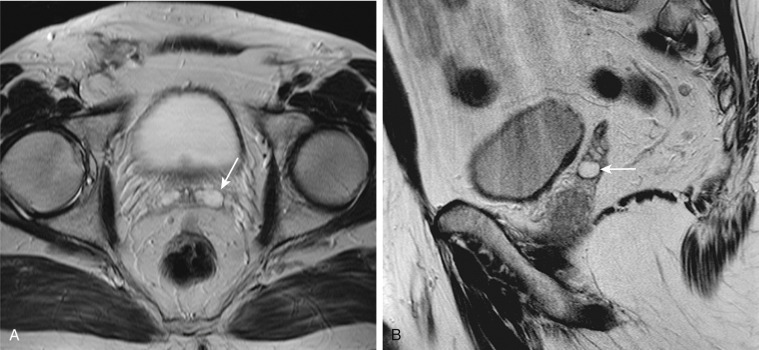
Seminal vesicle cysts may be congenital or acquired. They manifest as a mass between the rectum and base of the bladder and may be associated with ejaculatory duct dilation. They are usually unilateral, unilocular, and resemble dilated seminal vesicles ( Figure 74-4 ). Congenital cysts are often associated with ipsilateral genitourinary anomalies. An acquired cyst is usually associated with ejaculatory duct or seminal vesicle inflammation or obstruction such as prostatitis, seminal vesiculitis, or prostate surgery.
Associations with seminal vesicle cysts include the following:
Autosomal dominant polycystic kidney disease in which the seminal vesicle cysts are usually bilateral
Invasive local tumor or primary tumor of the seminal vesicle
Infection or chronic prostatitis
Benign prostatic hypertrophy
Ejaculatory duct obstruction
Seminal vesicle cysts usually are asymptomatic but may manifest as obstruction, recurrent urinary tract infections (including epididymitis), and hematospermia.
Seminal vesicle cysts can occur in any part of the gland. They vary in size and are benign. Superimposed infection may be seen.
Cysts are well-defined hypoattenuating lesions on CT.
The MRI features of seminal vesicle cysts are similar to those of cysts in other locations, with low signal intensity on T1-weighted images and a unilocular smooth-walled lesion with uniform high intensity and a well-defined margin on T2-weighted images (see Figure 74-4 ). Hemorrhagic cysts have high signal intensity on both T1- and T2-weighted images.
Cysts are seen as anechoic masses ( Figure 74-5 ). TRUS can be used to guide needle placement for drainage or contrast studies to more fully delineate the lesion.
The main differential diagnosis is müllerian duct cyst.
No medical treatment is required for seminal vesicle cysts. When seminal vesicle cysts are large, they may cause pain and local obstruction. Draining such cysts may relieve discomfort.
Seminal vesicle obstruction is defined as a seminal vesicle with an anteroposterior diameter of more than 15 mm, length longer than 50 mm, and large anechoic areas containing sperm on aspiration. Seminal vesicle obstruction may be congenital because of an ectopic ureter or acquired secondary to a local mass. It is important to recognize because it is associated with pain and male infertility.
The obstruction may be asymptomatic or painful when the gland becomes enlarged.
When seminal vesicle obstruction is due to congenital causes, it is most often unilateral. When acquired, it may be unilateral or bilateral. The seminal vesicles are usually normal histologically but may become secondarily infected.
CT will show an enlarged seminal vesicle.
The enlarged seminal vesicle is of normal signal intensity unless infected or infiltrated by tumor.
Ultrasound will show an enlarged seminal vesicle.
No clinical or laboratory data aid in the diagnosis. Tumor marker levels may be elevated when the obstruction is caused by a malignant mass.
There is no medical treatment for seminal vesicle obstruction. Surgery or image-guided aspiration may be required to treat symptomatic obstruction.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here