Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In 1922, Hone first described human infections “closely resembling typhus fever.” Since 1926, when Maxcy successfully identified murine typhus as a distinct clinical and epidemiologic entity, and 1931, when Dyer isolated a new typhus group named Rickettsia from rats and fleas, murine typhus has been recognized as a worldwide zoonotic problem. Often underrecognized and believed to be clinically mild, murine typhus may occur in epidemics or with high prevalence in certain geographic regions. Illness may be severe, particularly in the elderly, with death occurring in a small proportion of individuals. The association with both rat and cat fleas is now well established.
Rickettsia typhi, the causative agent of murine typhus, is an obligately intracellular bacterium that infects endothelial cells in mammalian hosts and midgut epithelial cells in the flea hosts. A new rickettsial agent, Rickettsia felis, has been recognized as sharing some antigenic and genetic components with R. typhi but is best phylogenomically characterized as a transitional group bacterium between typhus and spotted fever group rickettsiae. As typical for the genus Rickettsia, R. typhi contains rickettsial outer membrane protein B (OmpB) and the autotransporter Sca4, but its lack of rickettsial outer membrane protein A (OmpA), a characteristic of spotted fever group rickettsiae, resembles the typhus group. In addition to ompB, three other autotransporters— sca1, sca2, and sca3 —are expressed. OmpB mediates adhesion and entry events for other Rickettsia spp., and Sca2 also functions as an adhesin in spotted fever rickettsiae. In addition, the R. typhi genome encodes genes for several potentially membranolytic proteins ( tlyA, tlyC, pldA, and two phospholipase A2 genes) and RalF, a type IV secretion system effector that could facilitate cell invasion or endosomal escape. These organisms are well adapted for intracellular life because they lack enzymes for carbohydrate metabolism, lipid biosynthesis, nucleotide synthesis, and amino acid metabolism and a complete tricarboxylic acid cycle but possess several ATP-ADP translocase genes that likely mediate host energy parasitism. The genome encodes Sec, TolC, and type IV secretion system components. As in the case of TolC-dependent secretion of an ankyrin repeat–containing protein, Rickettsia ankyrin repeat protein 1 (RARP-1), these secretion system components suggest delivery of effector proteins into the host cell to influence cell function and fate. Unlike the situation for spotted fever group rickettsiae, R. typhi lacks rickA, which encodes a protein promoting intracellular motility via actin polymerization.
Murine typhus is found worldwide and is especially prevalent in tropical and subtropical seaboard regions, where the most important rat reservoirs ( Rattus spp.) and flea vectors ( Xenopsylla cheopis ) are found ( Fig. 190.1 ). Urban ports, often rife with rats, have been associated with a higher prevalence of murine typhus. An important vector in some areas (southern Texas and southern California) is the cat flea ( Ctenocephalides felis ), and opossums have been implicated as a potential reservoir in these areas. Thus residents and visitors to these urban and suburban regions are at risk when flea-bearing animals bring infected fleas into close proximity to humans. The demonstrable seroprevalence to typhus group antibodies in areas where the disease is endemic, and in areas where the disease is not well recognized, indicates that murine typhus is likely vastly overlooked.
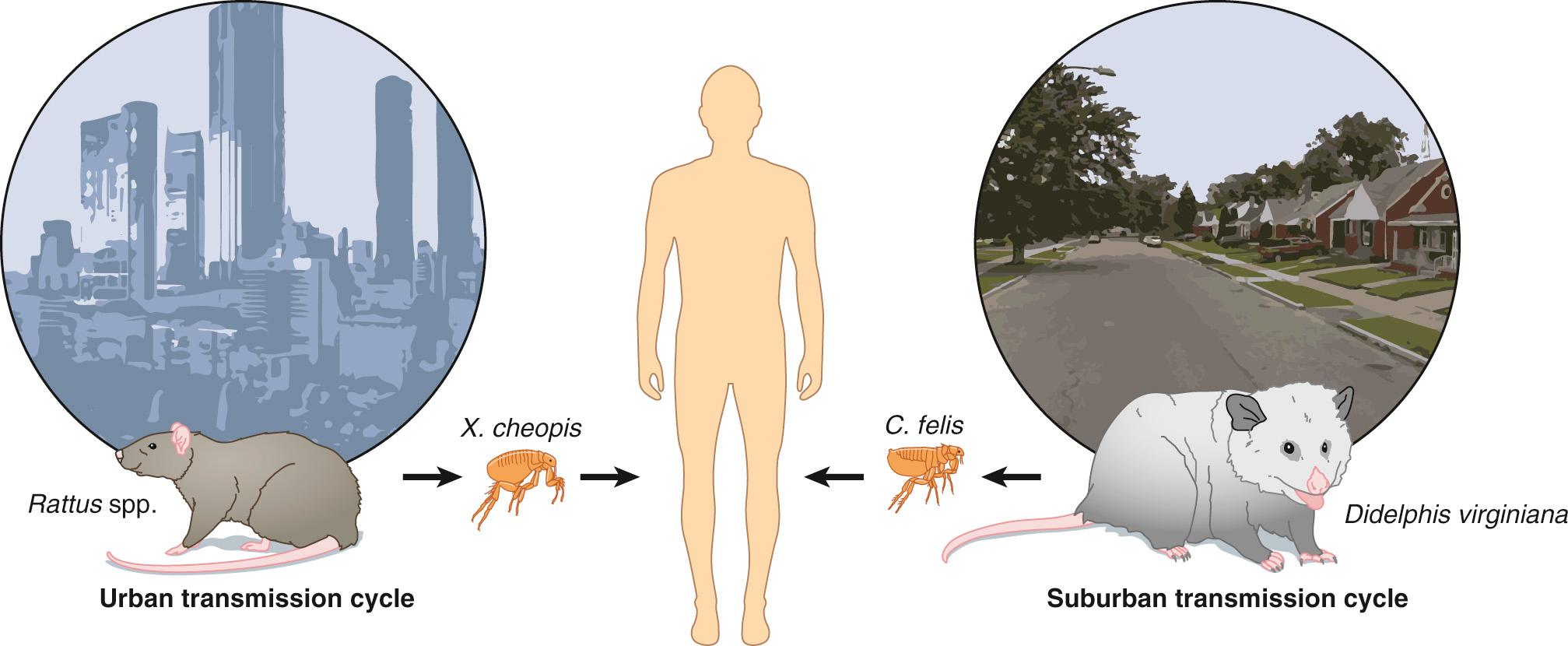
Murine typhus was once more prevalent in the United States, especially in the warm humid South. In 1944, at the peak of reporting, there were 5401 cases. Efforts to control rat populations, and more likely the strategic use of DDT on rat runs and harborages, made dramatic strides to break the rat-flea transmission cycle and decrease the prevalence of murine typhus. By 1956 fewer than 100 cases were reported in the United States. In the decades following this dramatic decline of murine typhus, there persists a low but increasing level of reported infections, with most cases seen in south Texas and southern California. In Texas, the last several decades have witnessed the majority of cases occurring in the southernmost counties along the Mexican border, but in the last 10 years there have been increasing reports of murine typhus occurring in more northern municipalities. Outbreaks in an urban area of central Texas, the northern Texas coast, and in Orange County, California, have been associated with opossums and R. typhi –infected Ct. felis. Epidemiologic observations have led to the hypothesis that cats, hosts for Ct. felis, play a role in the transmission of murine typhus. In addition, R. typhi has been isolated from Rhipicephalus sanguineus ticks collected from dogs. More studies are needed to elucidate the role domestic animals play in the transmission and maintenance of R. typhi.
Outbreaks throughout the world occur when there is inadequate vector and reservoir control. Among displaced Khmers at the Thailand-Cambodia border with unexplained fever, 70% were cases of murine typhus, with an attack rate of 172 per 100,000 adults. Murine typhus has been implicated in as many as 4% to 26% of cases of undifferentiated febrile illness in Nepal, 0.4% to 7% in countries of Southeast Asia, and as few as 0.5% in northern Tanzania. In northern Vietnam, when malaria, dengue, typhoid fever, and leptospirosis are excluded, R. typhi has been attributed to 33% of undifferentiated febrile illness. Most patients are adults, although persons of all ages may become ill. Cases are recognized year-round, with peak prevalence from April through June in Texas and during the warm months of summer and early fall elsewhere.
Murine typhus has been increasingly recognized as a febrile illness in travelers returning from endemic regions throughout the world. In an analysis of 3655 travelers considered to have acute and potentially life-threatening illnesses, murine typhus was the seventh most prevalent cause (identified in 16), and when excluding the diagnosis of Plasmodium falciparum malaria, occurred in 1.9% of febrile patients. Africa, Southeast Asia, South Asia, and the Americas have been reported as sites of disease acquisition in returning travelers.
The disease is transmitted after the inoculation of infected flea feces into a flea bite wound. The incubation period is 1 to 2 weeks, commonly 12 days. Because predominantly gut epithelial cells are infected in the flea vector, a reservoir of infected fleas is maintained mostly by horizontal transmission from flea to vertebrate host to uninfected flea. Once infected, the flea maintains the rickettsial infection for the duration of its life. Rickettsia typhi may also infect the flea reproductive organs, which explains the low levels of transovarial (vertical) transmission. The longevity of fleas is unaffected by gut epithelial cell or disseminated R. typhi infection.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here