Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
No single conceptual development has had as profound an impact on the field of hand surgery as the advent of microsurgical techniques. The ability to microscopically repair blood vessels led to an accelerated phase of discovery and innovation that continues to this day. The availability of microsurgical techniques has expanded the extent and type of injuries that can be considered reconstructible and have made these interventions relatively commonplace.
After the coaptation of blood vessels was first performed by Dr. Alexis Carrell in 1902, modifications followed in techniques for suturing and instrumentation and their applications. The great pioneers of microsurgery developed instrumentation and other techniques that allowed the anastomosis of blood vessels. After the techniques were deemed feasible experimentally, their initial applications were in treatment of the traumatized hand, with replantation being one of the earliest milestones.
In 1962 Malt and McKhann performed the first replantation of a completely severed arm in a 12-year-old boy in Boston. In 1963 Chen and colleagues performed the first successful replantation of an amputated hand in Shanghai, China. In 1968 the first replantation of an individual digit, a thumb, was achieved by Drs. Komatsu and Tamai in Japan. As centers became increasingly more familiar with the technique and as experience around the globe expanded, replantations of increasing complexity were performed. This has led us to the current day, in which the initial procedures for replantation have been adapted, refined, and extended and include repair of distal tip amputations, ectopic banking of amputated parts, , and, ultimately, vascularized composite allotransplantation.
Few studies have evaluated the impact of amputations and replantations on society. A study from Sweden determined the incidence to be 1.9 per 100,000 person-years (males 3.3, females 0.5). Eighty-six percent occurred in males and 9% in children (age 0 to 14 years). The majority occur in males 45 to 54 years of age. Factory workers (26%) and carpenters (14%) were most commonly injured. A large national database study of upper extremity amputation and replantation cases in the United States demonstrated that the patients undergoing replantation were younger (average age 36 years) than those suffering amputation but not undergoing replantation (average age 44 years). Replantation was most often performed in teaching hospitals and larger urban hospitals.
The patient sustaining an upper extremity amputation should be rapidly and efficiently transported to a specialty center capable of replantation. The patient’s candidacy for replantation should be determined after he or she has been assessed in the emergency department. The field trauma care of such a patient should follow the principles of global trauma management. It may be easy to overlook more urgent basic trauma protocols in the setting of the distracting, and sometimes dramatic, appearance of extremity amputations. The ABCs of trauma management should never be neglected.
Specific management of the amputated parts should include collection of all amputated parts in the field, regardless of the degree of contamination or quality of tissue. These parts should be wrapped in a sponge saturated with saline, placed in a plastic bag, and subsequently placed in a bag of ice or on a bed of ice. The goal is to cool the part but avoid freezing of the tissue. The bag should be labeled with the patient’s demographic information and transported with the patient to the hospital setting. The amputated stump should be treated with pressure dressings and elevation to control bleeding. Tourniquets should be avoided as well as attempts at ligation of blood vessels in the field, if possible.
In the emergency department, the amputated parts and the amputated stump should be evaluated for the purposes of operative planning and decision making. The patient’s limb and amputated parts should be evaluated radiographically. Tetanus prophylaxis should be provided.
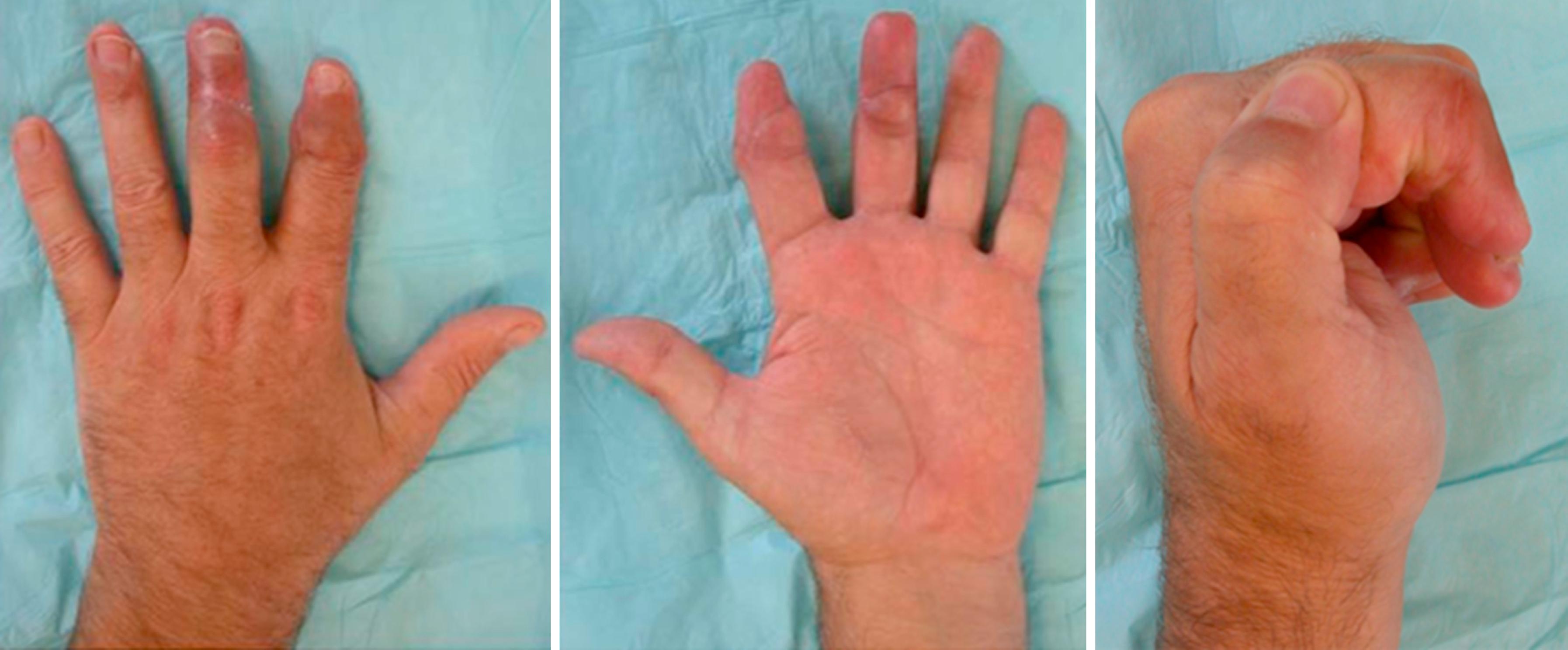
Very few indications or contraindications for replantation are absolute. The most compelling indications for replantation include thumb amputations at any level ( Fig. 42.1 ), multiple-digit amputations ( Fig. 42.2 ), any amputation in the pediatric population, and amputations through the wrist, forearm, and elbow. Contraindications for replantation include medical instability that would make lengthy surgical intervention excessively risky. Relative contraindications include single-digit amputations through zone 2 of the flexor tendon sheath, multilevel segmental amputations, and ring finger avulsion amputations. These are felt to be relative contraindications because the procedures are difficult to perform and satisfactory functional results are difficult to achieve. Reports of series of patients in these categories have been published demonstrating surprisingly good results, with authors questioning whether these conditions should be considered relative contraindications.
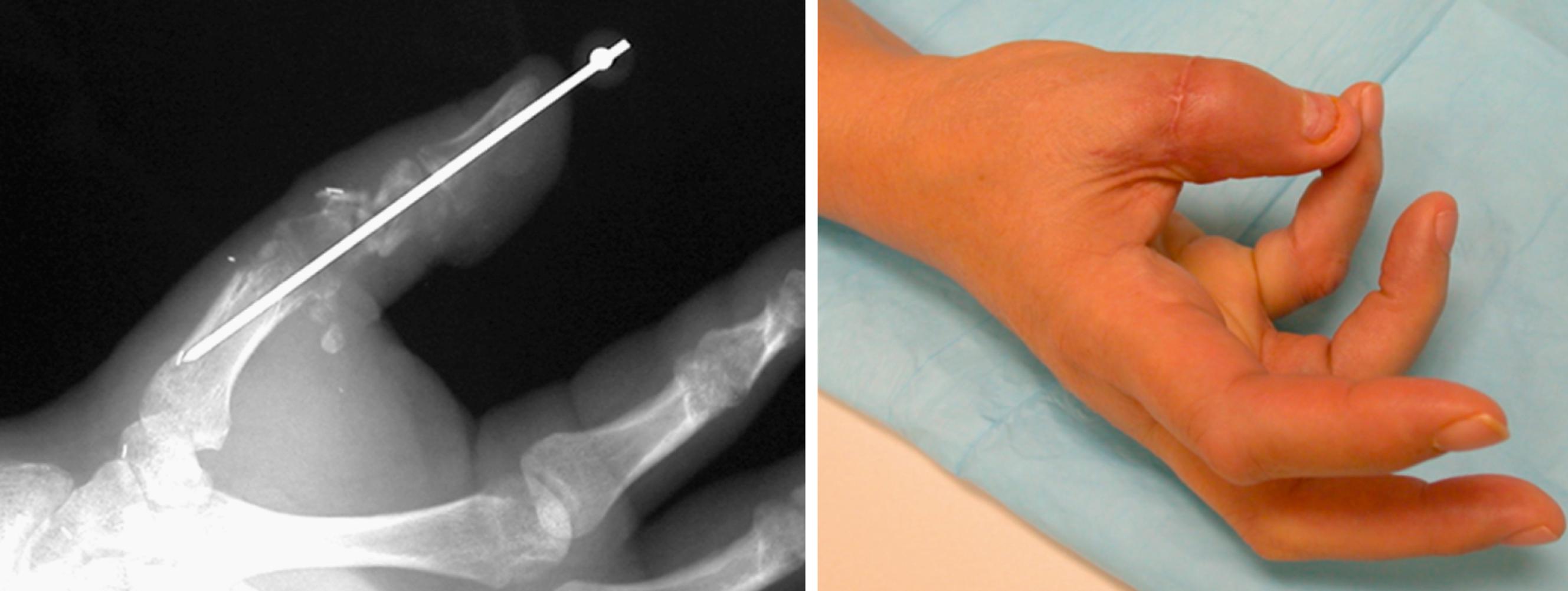

A relative indication for replantation is a single digit distal to the flexor digitorum superficialis (FDS) insertion. Although the functional loss from such an amputation in a digit other than the thumb is not great, surgical replantation of such an amputated digit can be performed quite speedily and the functional outcomes are good. Lack of involvement of the proximal interphalangeal joint and preservation of the FDS insertion will likely provide good proximal interphalangeal motion and an overall satisfying functional result even without significant return of distal interphalangeal flexion. For this reason, amputations at this level are felt to have a more favorable prognosis than those through zone 2 ( Fig. 42.3 ).
In a recent large study comparing 310 single digit revascularization/replantation cases with 710 revision amputations, authors Zhu et al. assessed outcomes at a minimum 1-year follow-up using the Michigan Hand Outcomes Questionnaire. The study subdivides the cases according to digit involved and level of injury. Significant functional benefit was noted in the revascularization/replantation subgroups over the revision amputation subgroups for all levels of single digit injuries involving the thumb and index finger. However, revascularization/replantation demonstrated no functional benefit over replantation in the subgroup of injuries occurring (1) distal to the flexor digitorum profundus (FDP) insertion in the middle finger, (2) distal to the FDS insertion in the ring finger, and (3) all levels of small finger. This study suggests that single digit replantation indications and contraindications should be assigned with specific consideration given to the level and digit involved. The study also provides useful data comparing costs, length of hospitalization, and time out of work for the two groups.
Special consideration should be given to major replantation cases. Good functional outcomes can be achieved with replantation through the midpalm, wrist, and forearm. The more proximal the amputation, however, the less promising will be the result because of the amount of nerve regeneration needed to achieve protective sensation and the potential for stiffness of the elbow joint; also, myonecrosis may occur in proximal replantation cases with a prolonged ischemia time.
The length of the ischemia time is a much less critical issue in digit-level amputations because muscle sensitive to ischemia is not present. At the level of the midpalm or wrist, the intrinsic muscles may be debrided if injured. If they are uninjured and are left intact despite a prolonged ischemia time, the resultant fibrosis and dysfunction may be manageable. In more proximal injuries, however, the muscle burden of an amputation through the proximal forearm or transhumeral level is quite significant. In these cases, the ischemia time becomes paramount.
Digit replantation is considered feasible if the warm ischemia time is limited to 6 to 12 hours. With a well-preserved, cooled part, cold ischemia can likely be tolerated for up to 24 hours after digital amputation prior to replantation. Sporadic cases of delayed digit replantation have been reported after 33 hours and 94 hours of warm and cold ischemia, respectively. , Successful hand replantation has been reported in one case after 54 hours of cold ischemia. The limits of tolerated ischemia time in distal amputations are thus poorly defined. Recent metaanalyses have suggested that ischemia time does not have a significant influence on replanted digit survival. , Indeed, Lin and colleagues studied ischemia time in 31 cases of hand and finger replantation that exceeded 24 hours and found no correlation between ischemia time and postoperative outcome. In the largest single center study to date, Cavades et al. examined a retrospective series of 456 consecutive replantation cases. Ischemia-sensitive cases were immediately replanted. These included amputations proximal to the palmar digital crease, lower extremity amputations, heavily contaminated/crushing injuries, agriculture-related amputations, and digit amputations with cold ischemia time in excess of 12 hours or warm ischemia time in excess of 6 hours. All other digit amputations ( n = 185 or 31%) were kept cooled between 4°C and 6°C overnight and replanted as the first case the following morning, with a goal of not exceeding 24 hours of cold ischemia before reestablishing arterial inflow. The survival rate of the immediate replantation group (91.2%) was not significantly different than the survival rate of the delayed replantation group (93.4%). There was no significant effect of age, level of replantation, or multiple digit replantation on the survival rate in either group. This study clearly demonstrates the feasibility of delaying digital replantation to the more optimal daytime operating room environment in the setting of experienced high-volume replantation centers.
In amputations involving the forearm, even 2 to 3 hours of warm ischemia time can result in substantial muscle necrosis, which can produce a coagulopathy after reperfusion. Venous outflow from the reperfused extremity contains toxic compounds such as oxygen-free radicals that can cause tissue damage and vasospasm. In these cases, cooling the amputated part (to 4°C) can dramatically prolong the time between injury and successful replantation. Cooling must be performed to the appropriate level because excessive cooling below 4°C can cause formation of intracellular crystals that can cause tissue damage similar to frostbite.
Properly cooled parts have been replanted up to 36 hours after the time of injury; however, the survival rate of an amputated part decreases with the delay to replantation.
It is these considerations of muscle burden, ischemia time, distance of required nerve regeneration, and degree of skeletal injury, as well as the mechanism of injury, that need to be considered in every case of major replantation.
Whether at the digit level or transhumeral level, replantation is best performed with a team effort. The efficiency, speed, and quality of replantation are enhanced using a team approach. Two teams enable simultaneous work on the amputation stump and the amputated parts. In lengthy cases (such as multiple-digit amputations), the team model allows surgeons to work in shifts; each shift of well-rested surgeons works with a fresh perspective and relieves the fatigued surgeons on the shift before them.
This approach should be used as soon as the decision to operate has been made. The amputated parts should be brought to the operating room so that debridement, dissection, and preparation can begin before the patient arrives in the operating room. This will minimize the patient’s anesthesia time and allow the surgical team to assess the quality of the part and thus the likelihood of replantation or technical requirements.
Much of the discussion that follows presents technical steps of replantation with considerations given to efficiency with an interest in minimizing tourniquet and anesthetic duration. However, a recent report demonstrated the safe use of the wide awake local anesthesia no tourniquet (WALANT) technique in eight successful cases of digital replantation. They list advantages of better assessing the tendon repairs and minimizing the anesthesia risk to patients with significant medical comorbidities. This technique may garner more interest in the field of replantation as the WALANT technique becomes more commonplace.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here