Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Evaluate submental adipose tissue, skin elasticity, and platysma laxity/integrity.
Neck liposuction is appropriate for those with pre-platysmal fat, good skin quality, and absence of platysma bands.
Laser-assisted liposuction can be beneficial in patients with submental fat and lax skin.
Add platysmaplasty for patients with good skin quality but with a non-decussated, lax platysma.
Patients with poor skin quality may require superficial musculoaponeurotic system plication, platysmaplasty, as well as skin excision.
Botulinum toxin treatment is an option for patients with good skin tone and platysma bands visible during teeth clenching.
Radiofrequency and ultrasound for tissue tightening of the submentum is beneficial for patients with mild submental and jowl laxity.
The effects of age, sun, and adipose redistribution take their toll on the neck as well as the face. It is important to keep this in mind when evaluating a patient with photoaging. The appearance of an aged neck in contrast to a newly resurfaced or lifted face is undesirable and a “white flag” that one has had surgery. In order to balance the face and neck, there are a variety of procedures available. Non-surgical or surgical rejuvenation of the neck can be performed using botulinum toxin, fractional laser resurfacing, standard ablative laser resurfacing, radiofrequency tissue tightening, ultrasound tissue tightening, laser-assisted liposuction, and liposuction with or without platysma repair or superficial muscular aponeurotic system (SMAS) plication. These therapies can be used alone or in combination, depending on the condition of the neck tissues. This chapter will focus on surgical recontouring of the neck using fractional CO 2 laser resurfacing, liposuction, laser-assisted liposuction, platysma repair, SMAS plication, and tissue tightening, using radiofrequency and ultrasound energy.
With the advent of tumescent liposuction in 1987, liposuction of excess adipose tissue from the submental area, jowls, and neck has become an attractive alternative to the face lift for cervicomental aesthetic surgery. With time, sun damage, and gravity, increased deposition of fatty tissue in the submental area, descent of the malar pads and sagging jowls, and neck skin redundancy, with or without banding of the platysma muscle, occur. This may give the appearance of excessive weight gain or aging to an otherwise healthy person. The traditional approach to these patients has been face-lift surgery, but with tumescent anesthesia, neck liposuction has evolved as a safe procedure to enhance the appearance of the neck and jawline in such individuals. Many variations and additions to neck liposuction have been employed. These include concomitant simple platysma plication, the corset platysma repair, laser-assisted liposuction, and a combination of neck liposuction, platysma plication, and SMAS plication.
Platysma repair can improve refinement of the cervicomental angle in addition to eliminating visible bands. The etiology of platysma bands is speculated to be due to stretching and loss of contractility of skin and fat overlying the anterior platysma, plus stretching of the overlying SMAS, which normally retracts the muscle. Both of these contractility failures are exacerbated with overuse of the muscles and advancing age. An alternative treatment for early and mild platysma muscle banding is botulinum toxin A (BTX-A) (Allergan Inc, Irvine, CA) injections into the vertical platysma bands. Although quite useful for patients with platysmal show during muscle contraction, BTX-A injections provide temporary (3–6 months) improvement and do not help patients with persistent sagging bands.
Those patients with excessive jowling or poor skin elasticity can benefit from concomitant SMAS plication and skin excision with repositioning. For patients with severe elastosis of the face with sagging skin at the temporal and malar areas, a full face lift may be appropriate. However, many patients have aging changes limited to the lower cheek and jowl, which can be greatly improved via SMAS plication and skin excision alone. The advantage of this safe, less invasive, and less time-consuming procedure, performed under local anesthesia, is that it eliminates the risks of intravenous or general anesthesia and gives excellent results with reduced morbidity. Some surgeons noted a disadvantage of limited SMAS plication is a potential reduction in the durability and longevity of the correction.
In addition, newer filler substances, such as hyaluronic acid, can be used to volumize the face, allowing for central lifting and decreased sagging. For patients with poor skin elasticity, fractionated laser resurfacing has been shown to improve the texture and tautness of the skin, and can also be used on the neck and chest area.
For those patients with mild jowling and submental neck skin laxity who do not wish to undergo surgery, radiofrequency and ultrasound-based devices have demonstrated minor amounts of tissue tightening. These will be discussed in greater detail later in the chapter.
1968 Millard, Pigott, and Hedo describe the submandibular lipectomy for neck enhancement
1971 Cronin and Biggs describe the T–Z plasty for the male “turkey-gobbler” neck
1978 Illouiz develops liposuction
1987 Klein develops tumescent liposuction
1992 Feldman describes the corset platysmaplasty
2001 Carruthers and Carruthers describe the use of botulinum in the mid and lower face and neck
2003 Radiofrequency tissue tightening is used to enhance cervicomental angles
2005 Laser-assisted liposuction revisited
2007 Ablative fractionated lasers are developed for skin rejuvenation
Choosing appropriate candidates for neck rejuvenation is essential and perhaps one of the most important determinants of the postoperative result. Examination for submental adipose, skin quality, and platysma laxity or prominence during teeth clenching can guide the physician to the appropriate procedure or combination of procedures. In addition, several analyses of cervicomental aesthetics have been performed, and show that patients with ideal neck proportions have cervicomental angles between 90 and 135°. The ideal position of the hyoid bone was found to be at the C3–C4 level, and at a location equal to or higher than the menton (the most inferior point on the mandibular symphysis in the midsagittal plane) (see Fig. 1.14 ). These details should be considered when selecting patients for neck liposuction, as additional procedures may need to be employed for maximum results. For example, those patients with relatively low-set hyoid bones are less likely to achieve a sharp cervicomental angle because their underlying anatomy will not support it. Hyoid position is an important landmark for muscular attachments and thus is an important determinant of neck angles and contour. Optimal candidates for neck liposuction include those patients with full jowls but otherwise good skin elasticity, patients with high-set hyoid bones, and those with submental fat pads palpable by pinch techniques ( Fig. 41.1 ).

Several maneuvers can be performed to assess submental fat; the patient is asked to clench their teeth, which will tighten the platysma muscle and define the fat as pre- or retroplatysmal fat. Preplatysmal fat can be suctioned through a small submental incision, but retroplatysmal fat must be excised directly. Asking the patient to place their tongue up against the hard palate will also help the surgeon to identify fat location as more retroplatysmal fat will protrude. The surgeon should also release the skin as part of a snap test to determine skin elasticity. If the skin feels loose and does not recoil quickly, or if the skin reveals vertical banding at rest, then liposuction alone is unlikely to provide maximal benefit ( Fig. 41.2 ). This type of patient may be a good candidate for a partial SMAS plication, platysma repair, radiofrequency tissue tightening after liposuction, or laser-assisted liposuction. The clenched teeth test is also useful to evaluate the platysma location and banding as non-decussating platysma muscle fibers become evident. Patients with prominent platysmal banding should be given the option for platysma repair at the time of liposuction as this will maximize final results ( Fig. 41.3 ).


The surgeon should also evaluate the submandibular gland position. Many patients have ptotic submandibular glands which appear as a subcutaneous fullness bilaterally along the inferior mid-portion of the mandibular ramus. This ptotic gland can resemble jowls, and is important to identify preoperatively. Platysma repair over these glands can improve this ptosis in some patients.
Gender may also play a role in patient selection. We have found that male neck skin takes longer to retract and redrape after neck liposuction as compared with female neck skin. Whether this is due to differences in hormones, skin thickness, or volume of fat removed, remains unclear. As with all patients, postoperative skin retraction with liposuction alone may be suboptimal if preoperative skin elasticity is poor. However, radiofrequency tissue tightening can be performed to improve laxity either prior to, or after liposuction. In addition, laser-assisted liposuction may heat and retract the underside of the dermis, allowing for smoother redraping and retraction of the skin.
Patients with mild jowling, good skin quality, submental neck skin laxity, and minimal submental adipose tissue are good candidates for the radiofrequency- or ultrasound-based energy treatment. Optimal patient selection parameters include patients aged 35–55, and those with thinner faces and thin skin.
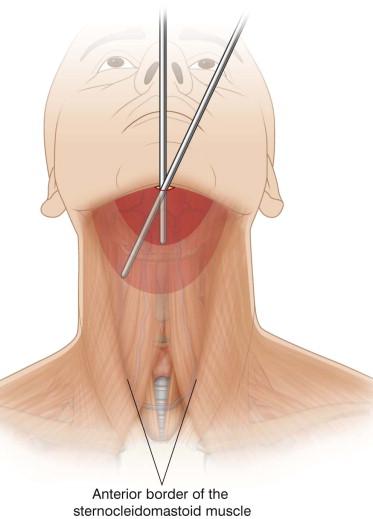
The process of neck liposuction involves first marking the mandibular border, jowls, submental fat pad, anterior borders of the sternocleidomastoid (SCM) muscle, left and right platysma bands (if present), and the thyroid cartilage. This is done with the patient in a seated position ( Fig. 41.4 ). Care must be taken to identify the jowl bilaterally, as it will extend slightly below the mandibular ramus. The superior extents of the jowl should also be marked. These guides help to delineate the areas for liposuction, and the top of the “T” placed at the level of the thyroid cartilage marks the distal extent for plication of the platysma, if necessary. Preoperative marking is essential to define landmarks that will be otherwise distorted after tumescence.

The procedure is performed in a well-equipped ambulatory surgery setting, with appropriate sterile technique and nursing staff assistance. The patient's face, neck, and upper shoulders are cleansed thoroughly with povidone-iodine and sterile towels are wrapped around the head. After the patient is prepped and draped in sterile fashion, a small amount of local full-strength (0.1% lidocaine) tumescent anesthesia is administered in the submental crease. With a no.11 blade, a small 2–3 mm incision site is made in the anesthetized area. The patient's head is gently extended back with the chin raised. A small-diameter, 6-inch, sprinkler-tipped infusion cannula is used to carefully deliver full-strength (0.1% lidocaine) tumescent solution through the submental incision into the immediate subdermal adipose compartment. Before and after tumescence, the patient is asked to purse the lips and clench the lower teeth to check the functioning of the marginal mandibular nerves. Occasionally, the anesthesia will inhibit functioning of the nerve, which is important to note before proceeding with the liposuction. For the lateral cheeks, a 20-gauge, 3.5-inch spinal needle (Becton Dickinson and Co, Franklin Lakes, NJ) is used to create infusion points 2 cm below the tragus. Tumescent solution is infused into the subcutaneous cheek and jowl areas bilaterally. Caution must be exercised during this buccal infiltration as overzealous filling can potentially lead to intraoral airway occlusion. A total of 300–500 mL of tumescent anesthesia is required to anesthetize the average patient's neck, cheeks, and jowls.
After tumescent anesthesia is complete and allowed to take effect over a 45-min time period, a 3-mm spatula-tipped liposuction cannula is used to gently debulk the submental, anterior, and lateral neck adipose tissue via machine suctioning through the submental incision (Aspirator III, Wells Johnson, Tucson, AZ) ( Table 41.1 ). This is fine tuned by aspiration using a 2-mm, 3–4-inch spatula-tipped cannula attached to either machine suction or a 5-mL syringe ( Fig. 41.5 ). The syringe method of suction has been evaluated by several surgeons and found to be a precise and controlled method for adipose removal. Caution must be used to keep the cannula in the mid to superficial fat and to stay medial to the anterior border of the SCM muscle. This helps to avoid injury to large veins in the area ( Fig. 41.6 ). Suctioning is then continued with the 2-mm spatula-tipped cannula through no.11 blade stab incision sites placed along the lateral portion of the jawline. Head extension and lateral rotation provides appropriate positioning for suctioning the cheek, jowl, lateral neck, and jawline. The mid-plane of jowl suctioning is first identified with syringe-assisted hand suctioning, followed by gentle contouring of the jowl and jawline via machine-assisted liposuction. During suctioning, the operator's free hand is used to identify the mandibular rim and the skin is lifted upwards by the cannula motion to prevent injury to the marginal mandibular nerve. It is important to note that while the patient's head is extended and laterally rotated, the marginal mandibular nerve (see Figs 1.16 and 38.2 ) may drop as much as two fingerbreadths below the mandible, become more superficial, and pose a greater risk for nerve injury. Care is taken to stay in a mid to superficial adipose plane.
| Instrument | Manufacturer |
|---|---|
| 3-mm, 6-inch spatula-tipped cannula | Bernsco Surgical Supply Inc, Seattle, WA |
| 2-mm, 3-inch spatula-tipped cannula | Wells Johnson, Tucson, AZ |
| 4-mm closed-neck dissector | Byron Medical, Tucson, AZ |

At times, it can be helpful to briefly turn the cannula opening upwards towards the dermis, particularly in the submental region. While contouring the cheeks and jowls, one must avoid aggressive suctioning of the medial and superior cheeks, as this can result in unwanted dimpling or hollowing. This is most likely to occur at the junction of the buccinator and masseter muscles, where the parotid duct travels through the buccinator to the oral mucosa. Labiomandibular tethering near the depressor anguli oris may require gentle blunt dissection with the cannula to allow adequate adipose removal and contouring of the jowls. Removal of neck adipose tissue extending to the medial border of the SCM muscles bilaterally and to the thyroid cartilage inferiorly is necessary if the surgeon will be performing platysma repair. After contouring is achieved, a 4-mm closed-neck dissector (Byron Medical, Tucson, AZ) may be used to release the superficial submental and anterior neck septae via the submental incision ( Fig. 41.7 ). In some patients, it can be of value to release these tethering fibrous bands to allow smooth redraping of the neck skin. The sharp “V”-shaped notch of the dissector allows a more thorough and gentle approach than aggressively swiping the area with a blunt cannula. Gentle rasping of the underside of the dermis may also facilitate tightening and adherence of the skin to the underlying muscle, but this concept is anecdotal and unproven. A cannula may then be used in a side-to-side motion to check for full release of the fibrous bands. Figure 41.8 shows the results of a neck liposuction-only procedure.


Laser lipolysis, either alone or in combination with liposuction, has been used to treat submental adiposity in the USA since the 1990s. A number of different lasers have been used, including the 1064-nm neodymium : yttrium aluminum garnet (Nd : YAG) and the diode laser (multiple wavelengths, including 810, 900, 924, 970, and 980 nm). Most recently, the 1320-nm wavelength has been introduced as part of a dual 1064/1320-nm system, with the goal of further enhancing skin tightening compared with single wavelength systems.
Despite the different wavelengths and platforms available, all laser lipolysis systems work by the same principal – selective photohyperthermia. When activated within adipose tissue, the laser light energy is converted to heat and absorbed by surrounding adipocytes. Histologic studies have demonstrated that the heat melts adipocytes via creation of a pore in the cell membranes. The laser is passed in a fan-like motion throughout the targeted adipose tissue in the same pattern as traditional liposuction, leading to the creation of tunnels lined by thermally damaged adipocytes. Some investigators believe that laser lipolysis can enhance traditional liposuction, giving the neck a more even contour, with enhanced formation of collagen in the treated area improving pre-existing wrinkling.
Although some reports have demonstrated good results using laser lipolysis alone, without traditional liposuction, current studies indicate that laser lipolysis alone can only effectively treat volumes of 100 cm 3 or less. Consequently, this technology is used most frequently in an attempt to enhance conventional liposuction. Laser lipolysis is thought to improve ease of suctioning if performed immediately before liposuction.
Most laser lipolysis systems use a 300-µm optical fiber ensheathed in a 1-mm cannula. The laser is equipped with a helium : neon aiming beam that facilitates visibility of the tip through the skin. This allows the operator to visualize the tip at all times, decreasing the risk of inadvertently damaging deeper structures or burning the skin itself.
Whereas lower energies cause tumefaction (reversible swelling) of adipocytes, higher energies have demonstrated lysis of adipocytes and significantly improved results. Although higher laser energies have been shown to enhance lysis of adipocytes and as much as a 20-cm 3 reduction in fat, these energies carry an increased risk of thermal injury to the skin. Additionally, given the small diameter and significant heat generated by these lasers, it is possible to penetrate the platysma, which could potentially lead to injury to the marginal mandibular nerve. It is recommended that surgeons undergo extensive training with these lasers before using them for treatment of neck adiposity. Katz and McBean reported local complications such as skin burns in 0.93% of patients in a retrospective study of 537 cases treated with the original 1064-nm laser. Albeit a low statistic, it is clear that the surgeon had performed more than 500 procedures, and was therefore experienced in the technique. Further prospective safety studies need to be performed from several investigative sites to determine the true rate of complications with these devices.
Alexiades-Armenakas reported utilization of a combination of laser-assisted lipolysis (LAL) and fractional radiofrequency-mediated minimally invasive skin tightening (MIST) to improve focal submental and neck adiposity and laxity using a single 2-mm incision in the submental crease. MIST refers to delivery of the laser or radiofrequency energy directly into the dermis or subcutaneous plane through needle electrodes or fiber cannula with the intent of increasing efficacy in treating lower face and neck laxity after addressing fat excess.
In a randomized, blinded comparison with the surgical face lift, MIST with fractional radiofrequency achieved 37% of the laxity reduction of the surgical face lift. In this 12-subject study, combination LAL-MIST with real-time temperature control for the Nd : YAG laser delivering 1064 nm, 1319 nm, or a combination of the two wavelengths (Sciton ProLipo PLUS system with TempASSURE, Sciton, Palo Alto, CA) was found to be safe and effective in the treatment of excess fat and skin laxity of the submentum and neck. A temperature of 45–48°C was maintained in the targeted plane for the LAL and MIST steps, with a total energy delivery of 5000–7000 J. Fat removal efficacy was consistent among the three wavelength combinations, with a mean aspirate of 7.0 ± 3.8 mL (range 3.0–15.0 mL) per subject ( Figs 41.9 , 41.10 ). Consistent and clinically meaningful skin reduction was achieved across the entire study population, regardless of laser type used, with a mean percentage grade improvement of 39.4 ± 12.1% over baseline ( p < 0.0005).


Common post-treatment included focal ecchymoses (resolved within 7 days), and edema, which persisted for approximately 2 weeks in all subjects. Some residual induration was evident for up to 3 months. Advantages of this included a single device, laser cannula, and entrance point. Additionally, LAL and MIST were effectively performed using a single wavelength.
In patients who lack decussation of the platysma (crossing of the medial fibers of the platysma), or who have visible platysma bands or laxity of the muscle fibers, plication can be performed. Current methods of platysma repair include bilateral platysma plication, midline platysma plication with transection of distal fibers, and neck lift with skin excision. The corset platysmaplasty, originally described by Feldman, is an extremely effective and comprehensive anterior approach to platysma tightening and correction of submandibular ptosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here