Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Children differ physiologically from adults and are susceptible to abnormalities in development and maturation not seen in adults. They differ in anatomy (e.g., the thymus) and are more susceptible to the harmful effects of ionizing radiation. This chapter will highlight some of the more common pediatric diseases associated with imaging findings.
Newborn respiratory distress
Transient tachypnea of the newborn
Neonatal respiratory distress syndrome
Meconium aspiration syndrome
Chronic lung disease of infancy
Childhood lung disease
Reactive airways disease/bronchiolitis
Asthma
Pneumonia
Soft tissues of the neck
Enlarged tonsils and adenoids
Epiglottitis
Croup (laryngotracheobronchitis)
Ingested foreign bodies
Other diseases
Cardiomegaly in infants
Salter-Harris growth plate fractures
Child abuse
Necrotizing enterocolitis (see also Chapter 19 )
Esophageal atresia with/without trachea-esophageal fistula
Hypertrophic pyloric stenosis ( Chapter 19 )
Intussusception ( Chapter 19 )
Developmental dysplasia of the hips ( Chapter 19 )
Respiratory distress is one of the most common presenting problems of newborns. Clues to its etiology include the infant’s gestational age , the severity and the progression of symptoms, and the appearance of the chest radiograph. There are many etiologies of respiratory distress including those produced by cardiac, metabolic, hematologic, and anatomic causes. Four pulmonary causes will be discussed but first, a word about names.
Pediatric diseases, like many other diseases, adjust their names over time. Table 27.1 contains the term we will use in this chapter and other names by which the disease has been or may be known.
| Used in the Chapter | Other Terms by which the Disease May Be Known |
|---|---|
| Transient tachypnea of the newborn (TTN) | Retained fetal fluid |
| Neonatal respiratory distress syndrome (NRDS) | Surfactant deficiency disorder Infantile respiratory distress syndrome Respiratory distress syndrome of newborn Hyaline membrane disease |
| Meconium aspiration syndrome | Neonatal aspiration of meconium |
| Chronic lung disease of infancy (CLD) | Chronic lung disease of prematurity Bronchopulmonary dysplasia |
| Growth plate fractures | Salter-Harris fractures Epiphyseal plate fractures Physeal plate fractures |
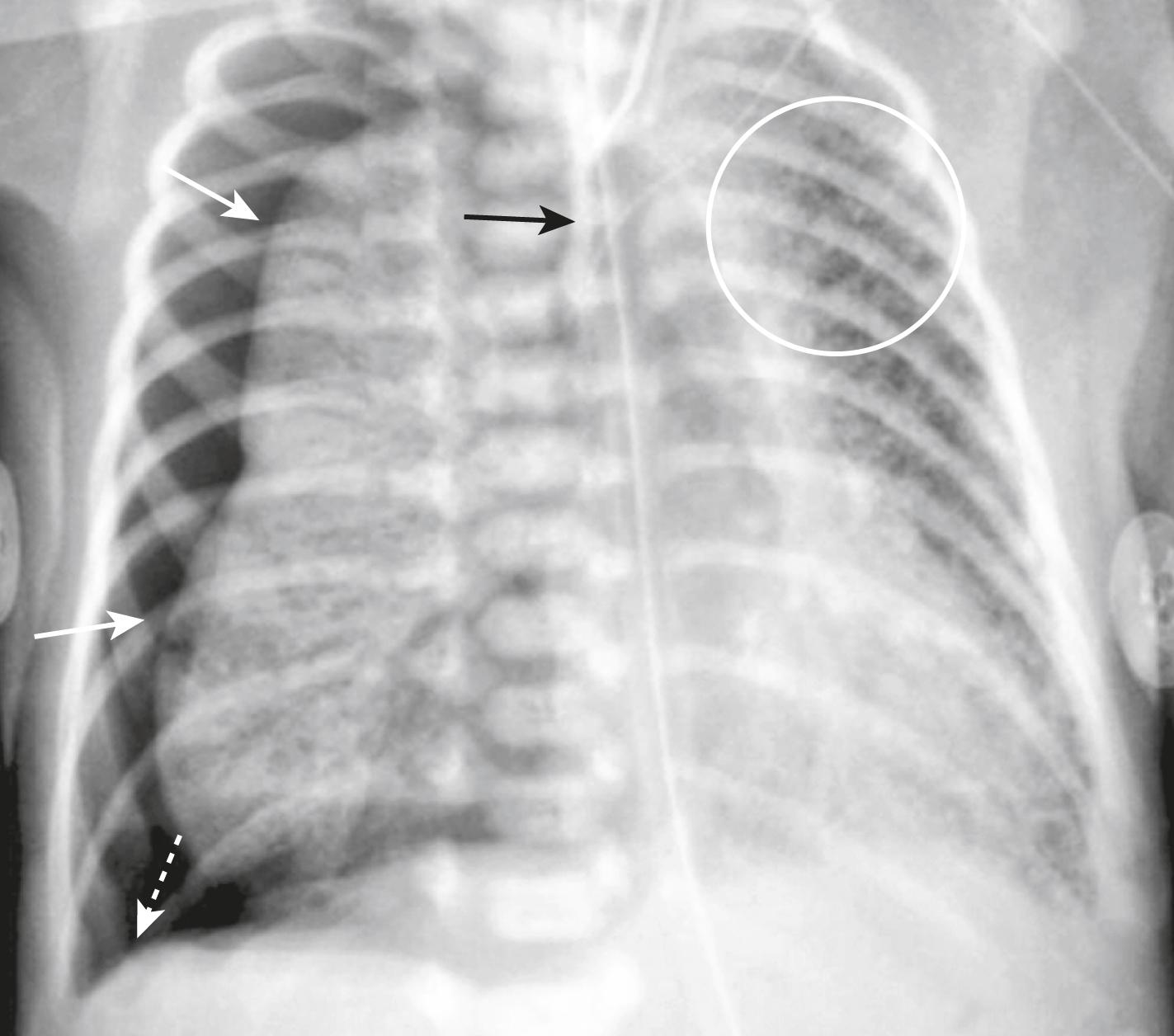
| Assisted ventilation with high peak inspiratory pressures and positive end-expiratory pressures may cause overdistension and rupture of alveoli | |
| Complication | Remarks |
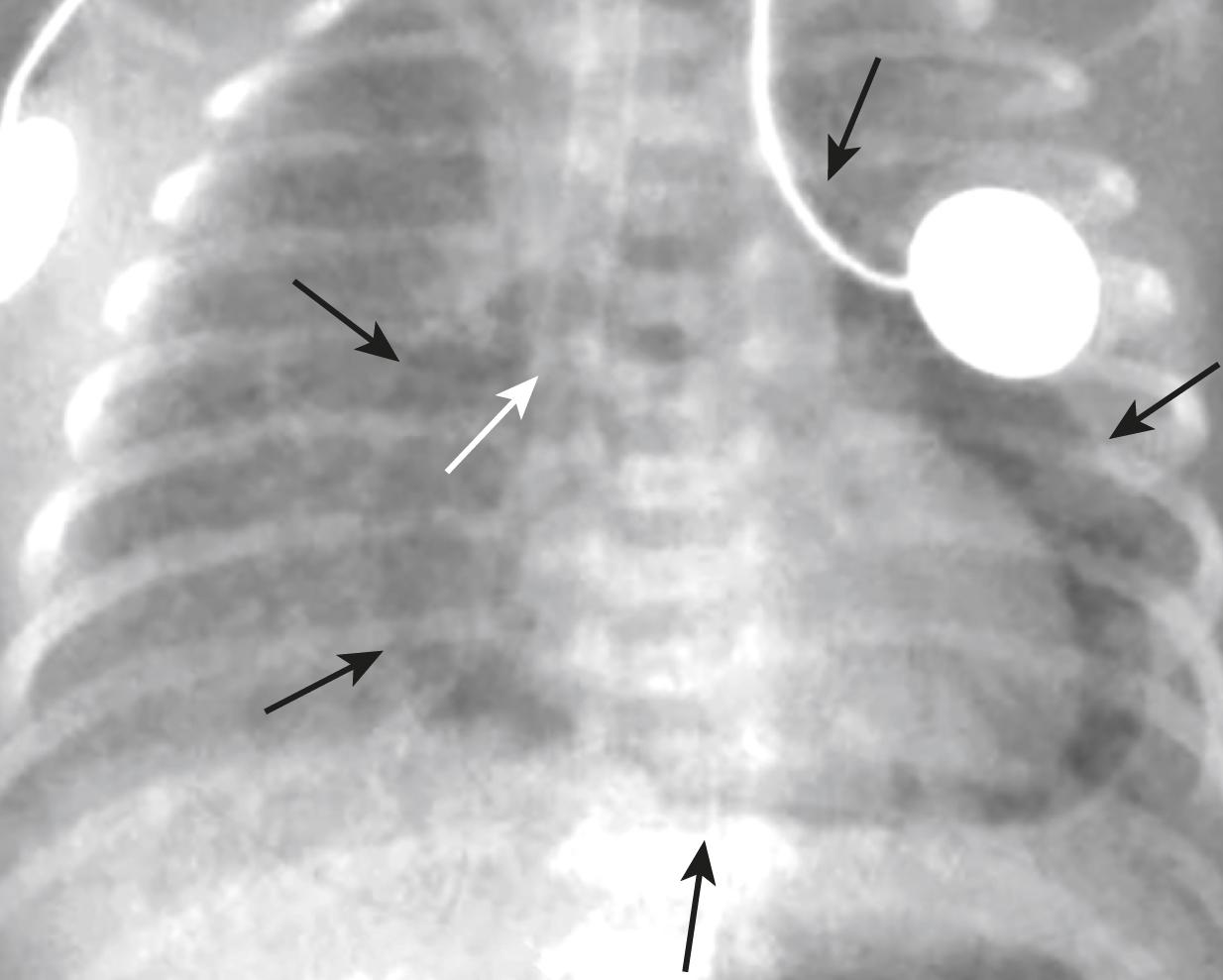
| Pulmonary interstitial emphysema | Rupture of an alveolus with dissection of the air back along the bronchovascular and perilymphatic interstitium may produce multiple small pockets of air in the lung called pulmonary interstitial emphysema . ( Fig. 27.6 ) |
| Pneumothorax | Rupture of an alveolus adjacent to the visceral pleural surface of the lung may dissect outward into the pleural space producing a pneumothorax. ( Fig. 27.7 ) |
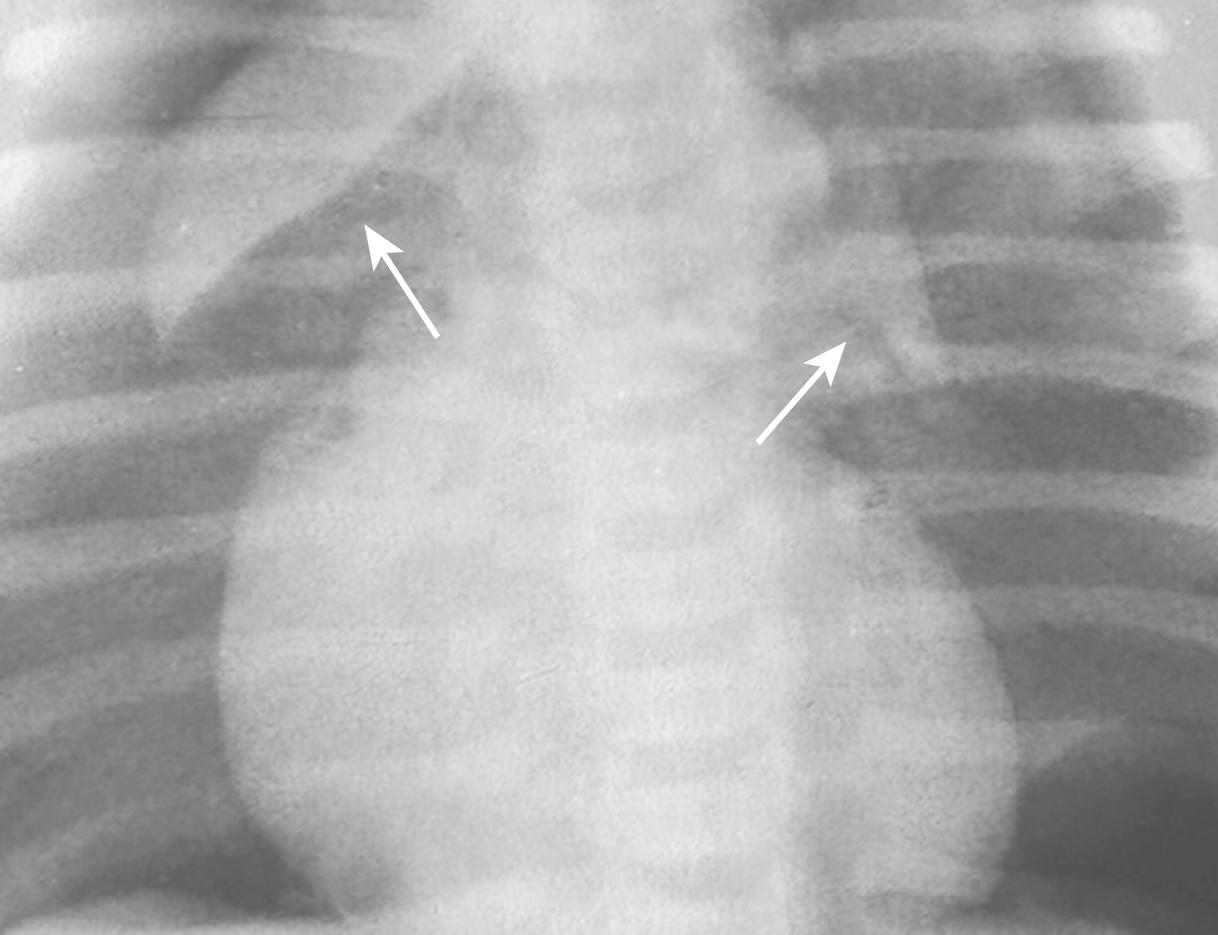
| Pneumomediastinum | Air leaks along the bronchovascular bundles of the lung will eventually reach the mediastinum and may produce a pneumomediastinum. ( Fig. 27.8 ) |
| Pneumopericardium | In infants, there may be connections between the mediastinum and the pericardial sac. Air that surrounds the heart but does not extend above the level of the great vessels may be a sign of pneumopericardium. ( Fig. 27.9 ) |
Occurring in infants born by Caesarian or precipitous vaginal delivery, transient tachypnea of the newborn is the most common cause of respiratory distress in the newborn. It is thought to be due to delay in the resorption of fetal lung fluid.
Clinically, TTN is marked by the immediate onset of tachypnea and mild respiratory distress. Intubation is usually not required. Infants typically improve over several hours with noninvasive oxygen supplementation and supportive therapy and completely recover by 48 hours.
Imaging findings of TTN:
The lungs are often hyperinflated, though less so in premature infants .
There can be streaky, perihilar linear densities.
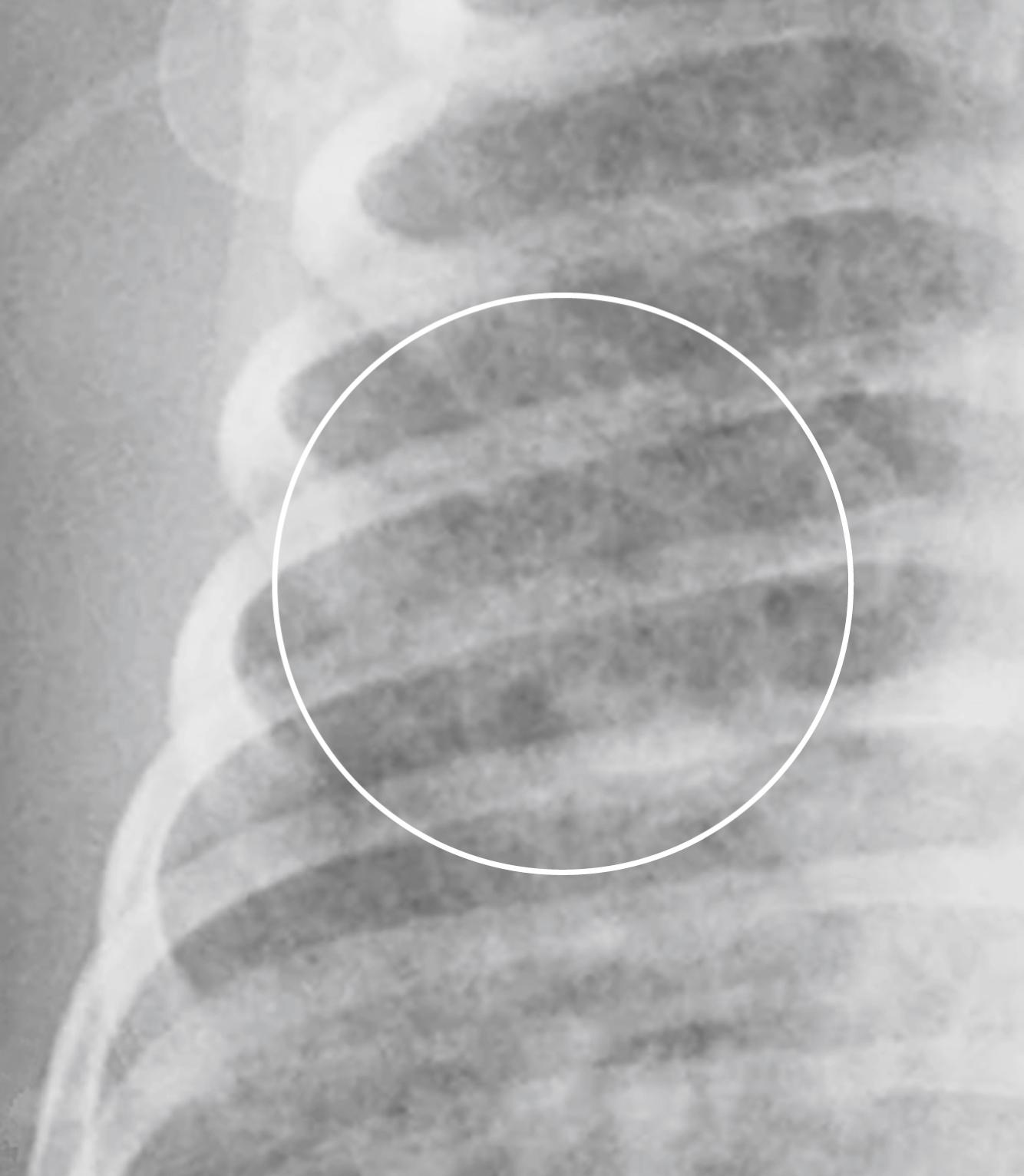
There also may be fluid in the fissures and/or laminar pleural effusions ( Fig. 27.1 ).
Neonatal respiratory distress syndrome (NRDS) is a disease of premature infants , usually less than 34 weeks of gestation. The incidence and severity of the disease often worsens with increasing prematurity. There are numerous risk factors, including perinatal asphyxia, hypoxia, and maternal diabetes.
The major cause of this disorder is surfactant deficiency. Without surfactant, the alveolar sacs have an increased tendency to collapse, leading to widespread atelectasis.
Typically, these premature infants have severe respiratory distress after birth that progressively worsens. Clinical findings include cyanosis, grunting, nasal flaring, intercostal and subcostal retractions, and tachypnea.
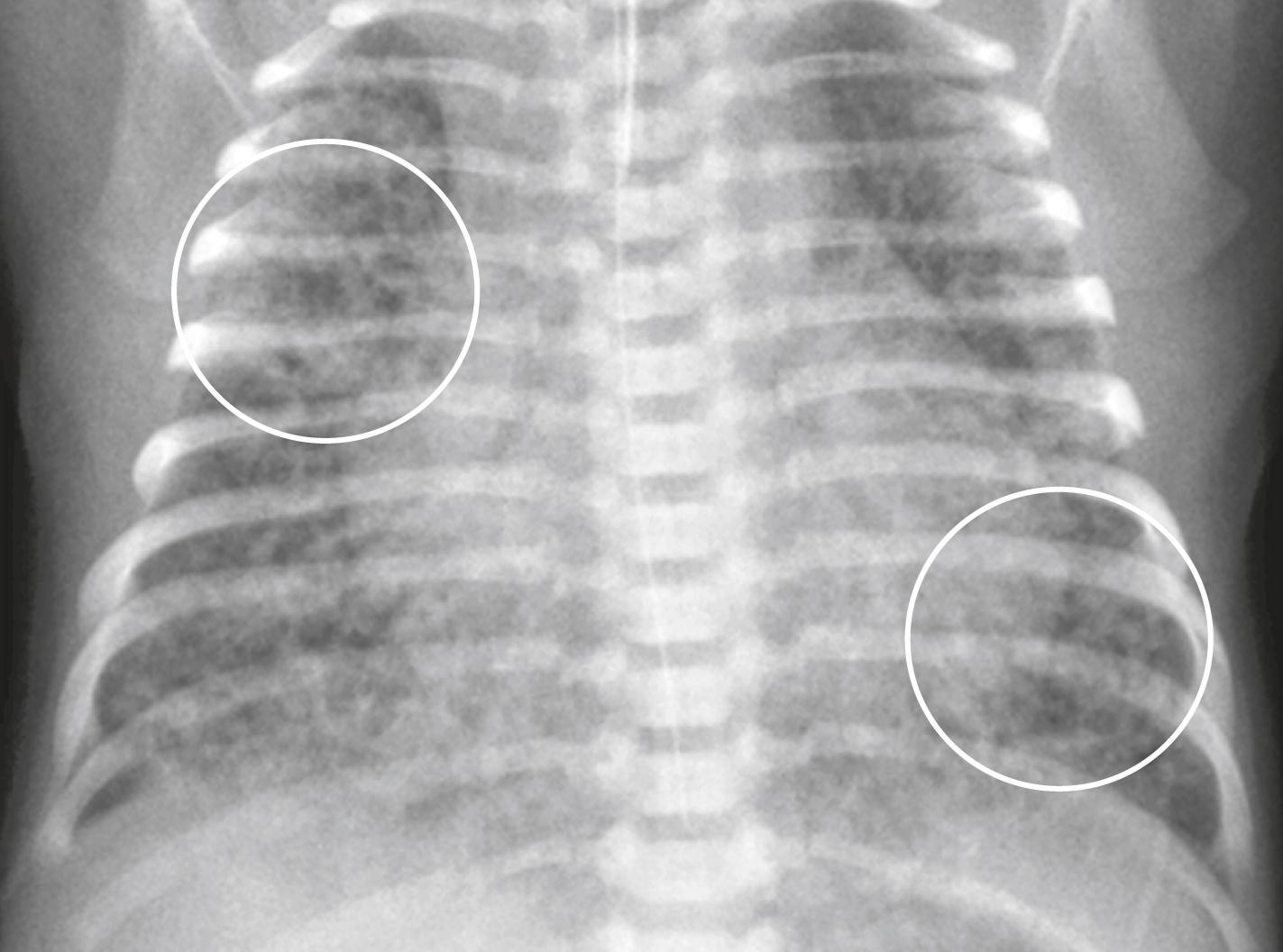
Imaging findings of NRDS ( Fig. 27.2 ):
There is typically a diffuse ground-glass or finely granular appearance to the lungs in a bilateral and symmetric distribution. The granularity seen in the lungs is the interplay of air-distended bronchioles and ducts against a background of atelectatic alveoli.
Air bronchograms are common and extensive, especially extending peripherally.
Hypoaeration is seen in nonmechanically ventilated lungs. Hyperinflation in nonintubated patients excludes NRDS.
Oxygen requirements progressively increase over the first few hours after birth. The treatment of NRDS generally includes positive-pressure ventilation and may include intratracheal surfactant replacement.
Infants who are very premature (23 to 27 weeks gestation) may require positive-pressure respiratory support for several weeks. The ductus arteriosus may fail to close, leading to patent ductus arteriosus , and pulmonary edema or hemorrhage can occur. They are at increased risk for the development of chronic lung disease of infancy.
The mortality rate from NRDS in the newborn varies by country and is dependent, in part, on the rate of premature births and the availability of appropriate treatment interventions in those who develop the disease. In the United States, the mortality rate has declined dramatically in the last several decades.
Meconium aspiration syndrome is most common in postmature infants.
Meconium is found in the amniotic fluid in approximately 15% to 20% of all pregnancies. As a consequence, meconium aspiration as such is considered to be a relatively common event. Meconium products produce bronchial obstruction, air trapping, and a chemical pneumonitis.
There is severe respiratory distress almost immediately , differentiating it from neonatal respiratory distress syndrome, whose onset is usually delayed by hours to a few days. However, whereas many infants with meconium aspiration have the onset of symptoms at birth, some infants have an asymptomatic period of several hours and then worsen over time.
Clinically, there may be tachypnea, hypoxia, and hypercapnia. Small airway obstruction may produce a ball-valve effect, leading to air trapping, overdistension, and air leaks.
Treatment is supportive, consisting of antibiotics and oxygen , inhaled nitric oxide, or extracorporeal membrane oxygenation (ECMO), if needed.
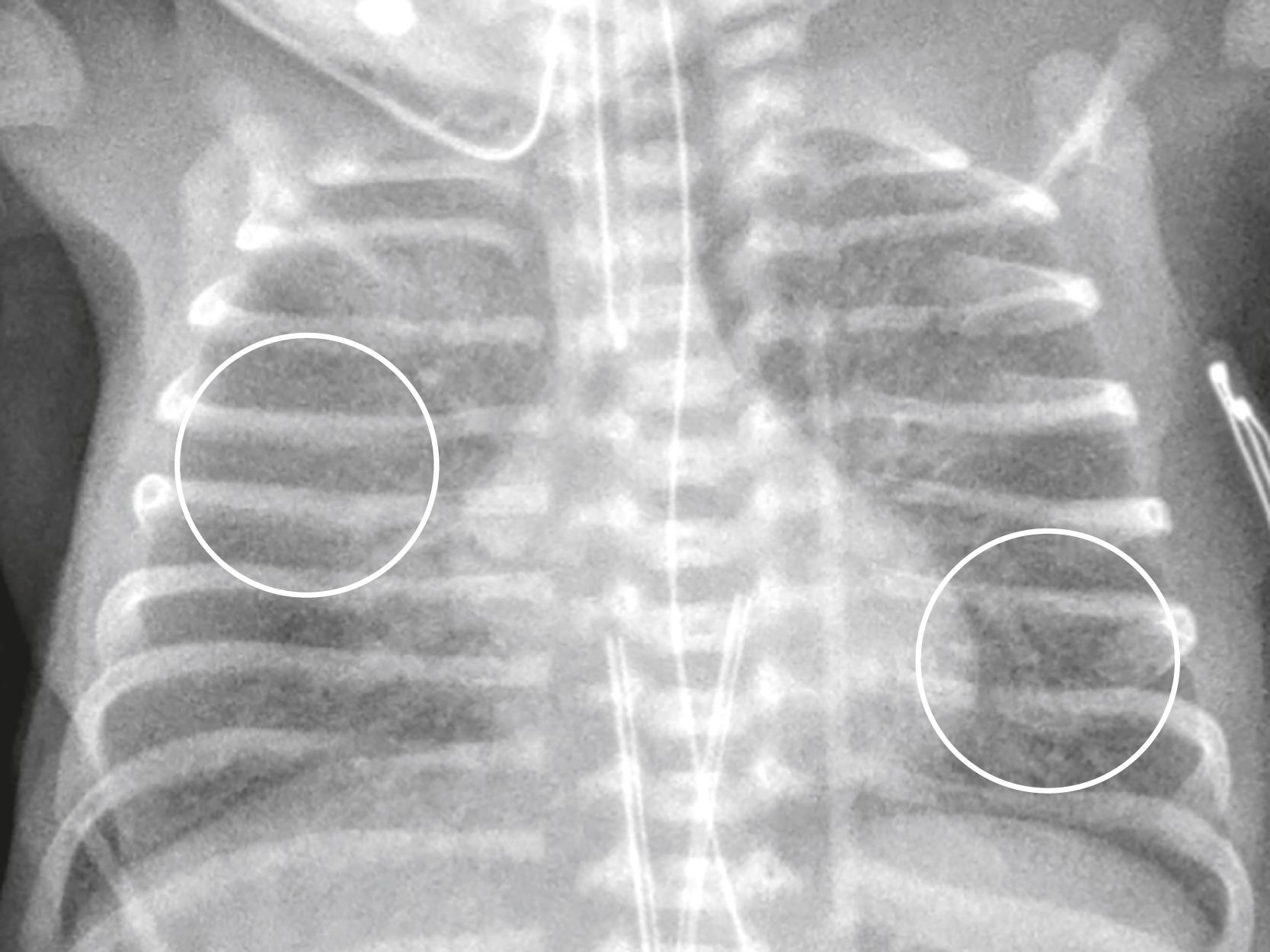
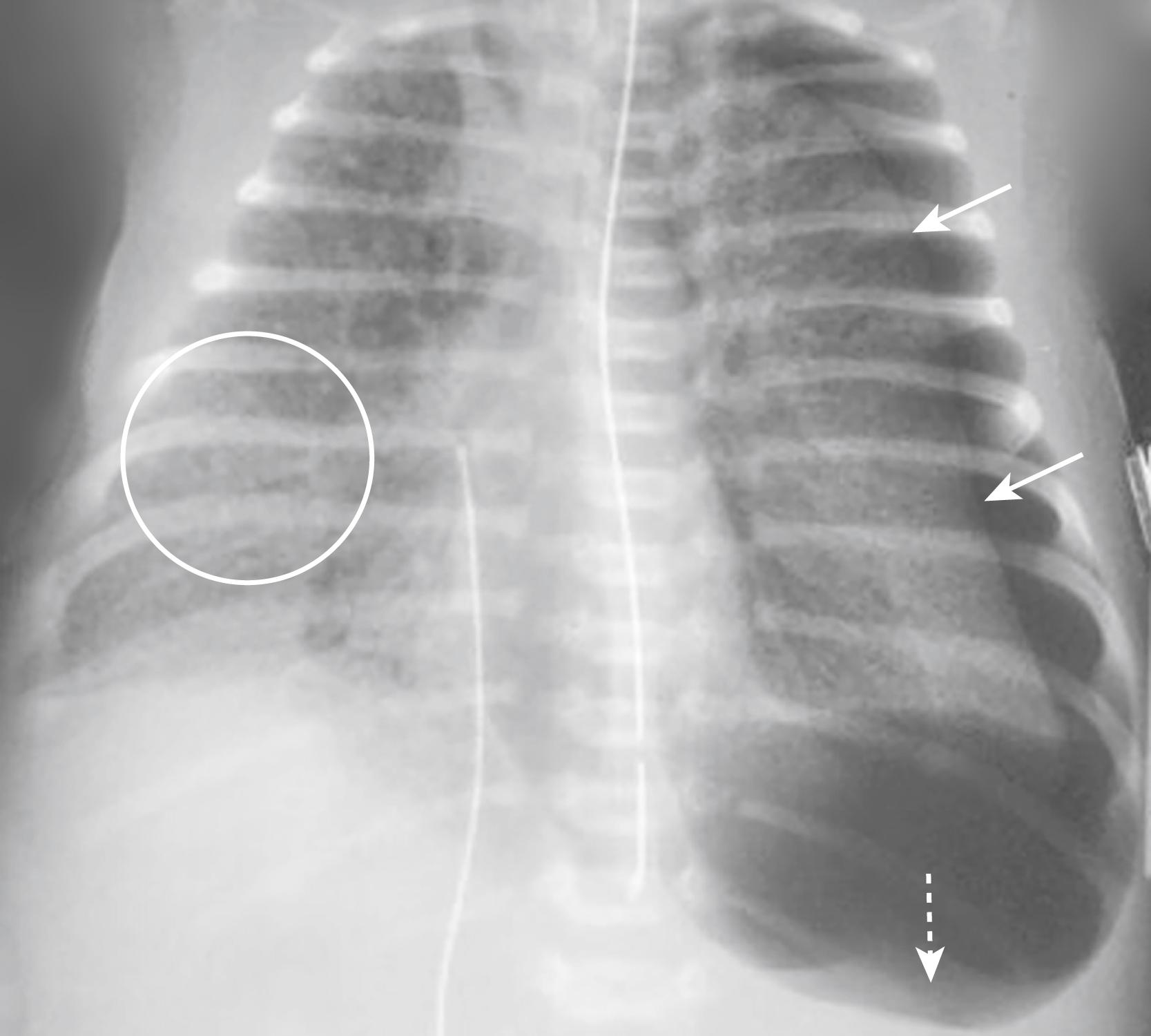
Imaging findings of meconium aspiration ( Fig. 27.3 ):
The lungs are hyperinflated with diffuse ropey densities (similar in appearance, but not in timing, to chronic lung disease of infancy).
There may be patchy areas of atelectasis and emphysema from air trapping.
Spontaneous pneumothorax and pneumomediastinum occur in 25% ( Fig. 27.4 ).
There may be an associated pneumonia , usually without air bronchograms.
Small pleural effusions may be present in 20%.
Chronic lung disease of infancy is a consequence of early, acute lung disease , frequently neonatal respiratory distress syndrome. CLD may also complicate meconium aspiration syndrome and neonatal pneumonia.
It is a clinical diagnosis with recently updated definitions including a degree of oxygen dependence at certain corrected gestational ages as well as abnormal lung parenchyma on chest radiograph.
Associated with most cases of CLD is the prior use of oxygen, which was administered under positive pressure.
Clinically, infants with CLD have oxygen dependence, hypercapnia, and a compensatory metabolic alkalosis. They may develop pulmonary arterial hypertension and right-sided heart failure.
CLD more often manifests in a milder form now than the severe manifestations of the disease when it was first described in 1967.
Imaging findings of CLD ( Fig. 27.5 ):
It may be impossible to distinguish early stages of chronic lung disease of infancy from later stages of NRDS.
The lungs are usually hyperaerated overall.
They may contain coarse, irregular, rope-like, linear densities representing atelectasis or, later, fibrosis.
These areas of atelectasis may be intermixed with lucent, cyst-like foci representing hyperexpanded areas of air trapping. Together, these processes give the lung a sponge-like appearance.
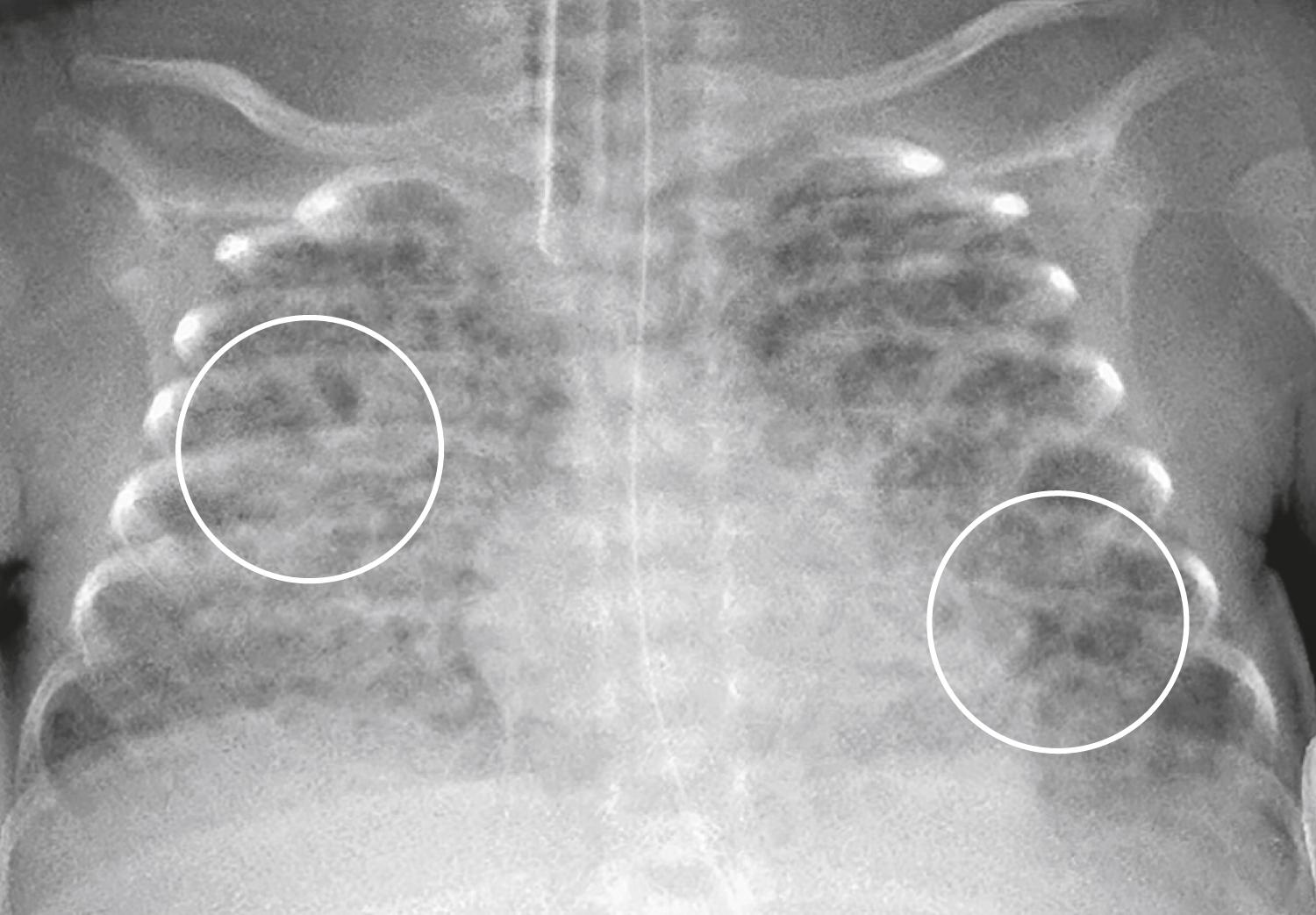
Infants with CLD may require mechanical ventilation for months. Changes of CLD will revert to normal on the chest radiograph in most patients after the age of 2 years although abnormalities may still remain visible on CT of the chest.
In any of these conditions (TTN, NRDS, meconium aspiration, and CLD), sudden worsening in the patient’s symptoms suggests the possibility of an air leak —a complication of positive-pressure ventilation in relatively noncompliant lungs. There are four manifestations of an air leak discussed in Table 27.2 , Figs. 27.6, 27.7, 27.8, and 27.9 .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here