Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In total, there are 31 spinal nerve root pairs: 8 in relation to the 7 cervical vertebrae, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal. In general, one nerve root is adjacent to each vertebra, but the cervical spine has an extra set of nerve roots accompanying the seven cervical vertebrae. At the cervical level, the first seven roots exit the spinal column above their respective vertebrae. The C8 root exits below the seventh cervical vertebra, and all nerve roots caudal to this level leave the spinal canal below their respective vertebrae.
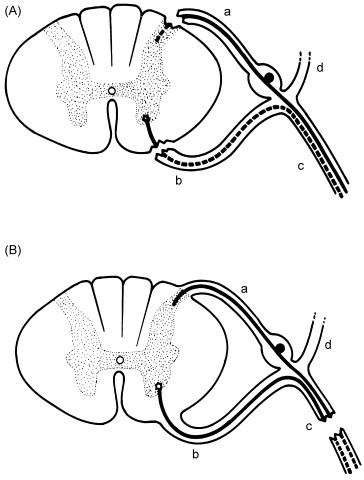
At each spinal level there is a ventral (anterior) and dorsal (posterior) root exit or entry zone, from or to the respective portions of the spinal cord. As shown in Figure 12.1 , the anterior horn of the homologous spinal cord level contains the cells of origin for the anterior motor root, while the primary sensory neuron cell bodies are within the dorsal root ganglion. The anterior or ventral (somatic motor) and posterior or dorsal (somatic sensory) roots join in the intervertebral foramen to form a combined motor and sensory spinal nerve, which then bifurcates into anterior and posterior primary rami. The larger anterior primary rami are the most important, particularly those in the cervical and lumbosacral regions, which innervate the muscles of the extremities (myotomes) and are the source for the sensory innervation of the skin (dermatomes). The posterior primary rami innervate the paraspinal musculature and the skin of the neck and posterior trunk.
Magnetic resonance imaging (MRI) is the procedure of choice to evaluate and characterize lesions affecting spinal nerve roots. With disc protrusions, MRI enables visualization of effacement of the nerve root by the herniated nucleus pulposus. In children, MRI imaging is useful to identify and characterize intra- and extramedullary lesions causing nerve root compression and radiculitis.
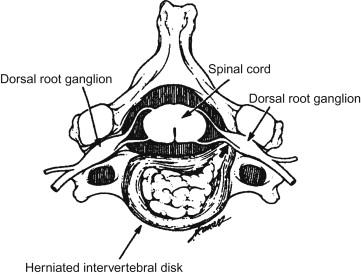
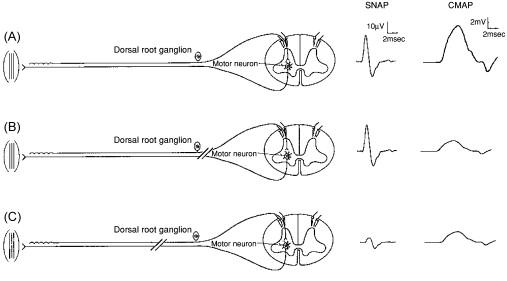
Nerve conduction studies are generally normal in radiculopathies. Intraspinal lesions, such as those seen with a herniated nucleus pulposus, occur prior to the bifurcation of the spinal nerve, affecting both its anterior and posterior primary rami. With compression of a single nerve root, motor nerve conduction studies tend to be normal because typically only a fraction of nerve fibers in the root undergo axon loss, and because of the overlapping segmental innervation of many muscles. At the same level the sensory nerve action potentials (SNAPs) are also normal, because the dorsal root ganglion is distal to the site of the damage, residing within the intervertebral foramen ( Figures 12.2 and 12.3 ). This is true for all cervical and lumbosacral root levels except L5, where up to 30% of dorsal root ganglia are intraspinal and therefore vulnerable to compression from disc extrusion, resulting in an abnormal superficial peroneal SNAP amplitude. Electromyography (EMG) in radiculopathies is more sensitive to changes affecting a single nerve root, showing signs of denervation (spontaneous discharges such as fibrillation potentials), in the paraspinal muscles as well as other muscles of the myotome corresponding to that spinal level.
In contrast, when the lesion is distal to the intervertebral foramen, the posterior ramus is spared and EMG of the paraspinal muscles is normal, while EMG of limb muscles shows the characteristic changes of denervation. One important caveat to the EMG assessment of radiculopathies in children is that, when they are anxious or upset, it can be difficult to obtain enough paraspinal muscle relaxation to adequately evaluate for abnormalities.
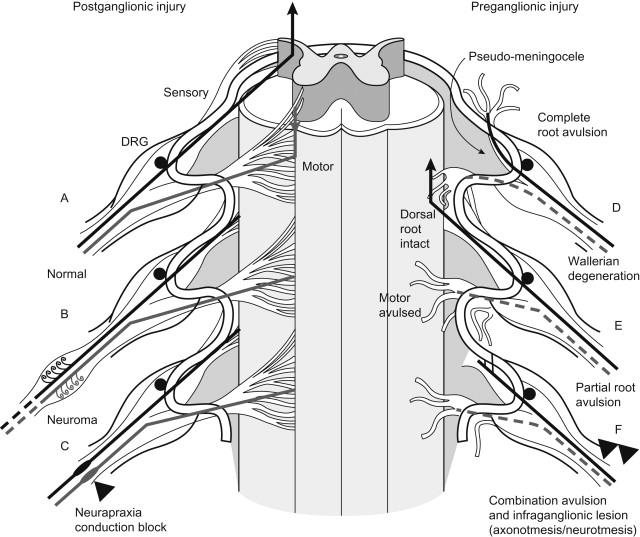
Children with peripheral nerve trauma may have both nerve root avulsion and plexus injuries. In the pediatric age group, therefore, EMG findings compatible with a primary plexus lesion (i.e. absent SNAPs) do not exclude additional damage at the nerve root level ( Figure 12.4 ). A combined process should always be considered in patients with possible proximal nerve lesions.
Cervical nerve root lesions in children are rare, but tend to mimic the signs and symptoms of cervical radiculopathy in adults: local or radiating pain and focal weakness, with or without focal loss of the deep tendon reflexes. In adults C7 root lesions are most common, followed by C6 root lesions, but in children there are too few such lesions to judge their relative frequency.
Most cervical radiculopathies in childhood follow trauma or traction injuries (see Case Example 12.1 ), but tumors, inflammatory lesions and other extramedullary lesions can also cause nerve root compression or injury ( Box 12.1 ).
A 15-year-old boy, who participated on his high school wrestling team, developed intermittent numbness and tingling in his right shoulder, radiating down his upper lateral arm, and lasting 15 minutes at a time. Three months earlier he had had an episode of “whole arm” numbness, and he had a history of multiple right shoulder dislocations requiring surgery some years earlier. No specific neurologic abnormalities were identified on examination.
He was referred to the EMG laboratory. The right median, ulnar, radial, medial, and lateral antebrachial cutaneous sensory amplitudes and distal latencies were normal. Similarly his right median and ulnar motor conduction studies and associated F-latencies were normal. Concentric needle EMG demonstrated mildly reduced recruitment in several C6–7 innervated muscles including biceps, deltoid, triceps, and brachioradialis. There was no abnormal spontaneous activity in these muscles or in the right C5–6 paraspinals. These findings were suggestive of a mild patchy chronic right C6–7 radiculopathy with no significant signs of active or chronic denervation. He was restricted from wrestling, as this was thought to be the pathophysiologic mechanism for his injury, and his symptoms resolved.
Cervical radiculopathies are very rare in the pediatric population but may be triggered by athletic activities. These injuries have to be differentiated from traumatic lesions at the level of the brachial plexus, including the so-called stinger injury. The two major proposed etiologies for these athletic injuries are either cervical nerve root compression and traction or a mild stretch injury to the upper trunk of the brachial plexus. If weakness persists, and either MRI or EMG evidence of a nerve root lesion is identified, one may need to consider cervical laminectomy.
Trauma: athletics injuries.
Inflammatory lesions: pseudoneoplasm.
Extramedullary lesions: hematoma.
It is important to be familiar with the clinical characteristics of radiculopathies at each spinal level, because these lesions may mimic much more common clinical entities, such as mononeuropathies or plexopathies. Most individuals with cervical radiculopathy have cervical or periscapular pain, which often radiates into the arm. With traumatic radiculopathies, this pain may precede the onset of numbness by 4 to 8 weeks, can spontaneously improve, and can then be followed by paresthesia and weakness a few weeks later. C7 or C6 nerve root lesions typically present with numbness affecting digits two or three, in a similar distribution to a median neuropathy. In contrast, C8 radiculopathies cause sensory symptoms involving the fifth digit, mimicking the distribution of the ipsilateral ulnar nerve or medial cord of the brachial plexus. When there is weakness, the triceps muscle is particularly affected in C7 lesions and the pronator teres and flexor carpi radialis in C6 radiculopathies; and the intrinsic hand muscles, flexor pollicis longus, extensor pollicis longus, and extensor indicis proprius are typically weakened by C8 nerve root lesions.
Refer to Box 12.2 for a list of differential diagnoses, discussed in the following subsections.
Congenital cervical stenosis
Hirayama disease
Motor neuron disease
Neck–tongue syndrome
Grisel syndrome
Neurogenic thoracic outlet syndrome.
Although the authors’ experience has not included any typical cervical radiculopathies secondary to either spinal disk or osteophyte-induced foraminal stenosis, we have seen occasional cases of pain in neck, shoulders or arms, or of painless progressive upper extremity weakness, with changes of chronic denervation on EMG and imaging evidence of congenital spinal stenosis, often in association with segmentation anomalies affecting the cervical spine.
This cervical myelopathy causes progressive painless wasting and weakness of the distal upper extremities in adolescence. Most affected children are teenage males, often of western Pacific Rim heritage. Weakness progresses for a few years then arrests spontaneously, for reasons which are poorly understood. Neuropathologic and radiologic findings in this condition suggest forward displacement of the posterior cervical dural sac during neck flexion, causing compression of the cervical cord and ischemic changes in the anterior horn. Because Hirayama disease usually initially affects hand function, it can be confused with ulnar neuropathy, a medial cord brachial plexus lesion, or C8 radiculopathy.
The authors have seen only one case of juvenile motor neuron disease, in a teenager with a one-year history of progressive painless weakness of one arm. In this adolescent the median and ulnar compound muscle action potentials were absent, the SNAPs normal, and needle EMG demonstrated diffuse fibrillation potentials with almost no definable motor unit potentials (MUPs). Eighteen months later, when she died, an autopsy demonstrated classic ALS. In a major review of 123 ALS patients there was only one similar case of symptoms of MND commencing before age 20 years.
Grisel syndrome is an atraumatic atlanto-axial subluxation which may follow inflammatory or infection conditions in the head and neck. Affected children typically present with unrelenting neck or throat pain, followed by torticollis, usually with a preceding history of a flu-like illness, tonsillitis, or pharyngitis. Other neurologic manifestations may include greater occipital nerve paresthesias and development of long-tract signs due to cervical myelopathy. Occasional patients develop cervical radiculopathy. The physical findings include tenderness to spinal percussion and restriction of neck movement leading to a torticollis. Plain X-rays and MRI imaging demonstrate atlanto-axial subluxation. Treatment with antibiotics, anti-inflammatories, immobilization and/or traction is important in order to prevent cord injury.
A similar condition, neck-tongue syndrome, presents with paroxysmal attacks of sharp unilateral neck pain associated with ipsilateral tongue numbness, which may be precipitated by rotation of the neck. Some cases are associated with torticollis, tongue deviation, and dysarthria. Symptoms are presumed related to intermittent compression of the C2 nerve root, and respond in most cases to conservative treatment.
This disorder is caused by a congenital aberrant fibrous band extending from an elongated C7 transverse process to the first thoracic rib, and can come to clinical attention in late adolescence or early adulthood. Patients describe atrophy and weakness of hand muscles, aching in the medial forearm, and occasionally loss of sensation along the ulnar aspect of the hand. The initial consideration is of ulnar neuropathy or C8 radiculopathy. However, close inspection shows predominant weakness and atrophy of the thenar eminence. The pathology stems from progressive extraspinal stretching of the T1 anterior primary ramus over the fibrous band. Nerve conduction studies (NCS) show the classic pattern of severe reduction of the median CMAP to the thenar eminence (abductor pollicis brevis muscle), less reduction of the ulnar compound muscle action potential (CMAP) to the hypothenar eminence (abductor digiti minimi muscle), severe reduction of medial antebrachial cutaneous SNAP and less reduction of the ulnar SNAP to digit 5. Based on this electrical pattern, imaging should be performed to identify the elongated transverse process and band, and surgery is indicated to section the band and release the T1 nerve trunk.
On the rare occasions that intervertebral disk herniation occurs in children, it usually occurs in the lumbosacral area. See Box 12.3 for reported causes of pediatric lumbar radiculopathies.
Trauma: sport-related, falls, heavy lifting.
Postoperative: direct trauma, or traction.
Developmental anomalies: vertebral anomalies, synovial cysts, diskal cysts, arachnoid cysts.
Tumors: schwannoma, osteblastoma, osteosarcoma, leukemia, synovial sarcoma, giant cell tumor, aneurysmal bone cyst.
Immunosuppression: chemotherapy, bone marrow transplantation, radiotherapy.
Most cases are in adolescent boys. Trauma, related to sporting activities, lifting, falls, or occupational injuries, accounts for at least one-third to one-half of pediatric lumbosacral radiculopathies. The youngest such case was of a 27-month-old boy who fell from his crib. A significant proportion (13–57%) of adolescents with lumbosacral disc disease has a first-degree relative with a similar history, suggesting a genetic component to this condition.
Scoliosis surgery also predisposes to development of pediatric lumbosacral radiculopathies. One series attributed a 29% incidence of these lesions postoperatively to either surgical trauma or traction in the lumbosacral area. Intraoperative spinal monitoring may aid prevention of this surgical complication.
Developmental anomalies involving intramedullary and extramedullary structures can impinge on the spinal roots, causing pain, weakness and sensory changes.
Nerve root tumors occasionally present with radicular pain radiating into the lower extremities, with or without sensory changes and focal weakness. Reported causes of this syndrome include schwannoma, leukemia, synovial sarcoma, osteoblastoma, osteosarcoma, and aneurysmal bone cysts. Treatment of childhood malignancies with chemotherapy, radiotherapy, and bone marrow transplantation may also be followed by radiculitis.
Most children present with back pain and sciatica. Pain is not invariable; occasional children develop a painless scoliosis. Children aged less than 10 years present with irritability, paravertebral muscle spasm, and leg weakness.
Neurologic deficits are usually relatively subtle and apparent at only one spinal level. A mild degree of focal weakness is seen in 32–60% of adolescents, most often involving the L5 musculature (tibialis anterior, extensor hallucis, and/or extensor digitorum). This is not generally severe enough to cause a foot drop. Well-defined sensory loss may or may not be present. In addition, paravertebral muscle spasm with concomitant limitation of spinal motion, cough-sneeze exacerbation (76%), and/or a positive Lasègue sign are often apparent. Most adolescents have pain on straight-leg raise or back motion. Disturbances of bladder and bowel function, however, are very rare and should prompt consideration of intrinsic cord dysfunction.
Routine spinal radiographs may demonstrate congenital bony and spinal segmentation anomalies, but the significance of these is often uncertain. A combined diagnostic approach including lumbosacral X-rays, lumbosacral spine MRI, CT imaging in certain cases, and—when these studies are nondiagnostic—EMG, has been recommended for diagnosis of lumbar nerve root disease in teenage children.
Infections, malignancies, and spinal injuries or developmental disorders such as spondylolisthesis should be considered in all children with spinal pain, lumbar nerve root symptoms, and an abnormal gait. As in adults, acute back pain is usually a self-limited musculoskeletal disorder that does not require investigation, and which responds to mobilization exercises and nonsteroidal anti-inflammatory medications. However, there are red flags that should trigger more aggressive evaluation. These include fever; pain that does not improve at night, at rest, or when supine; weight loss; known malignancy; or when symptoms extend beyond several weeks. See Box 12.4 for a list of differential diagnoses.
Infections: diskitis.
Inflammatory conditions: ankylosing spondylitis, sacro-iliac misalignment.
Developmental anomalies: Chiari malformation, tethered cord, cord lipoma.
Mass lesions: angiolipoma, arteriovenous hemangioma, cavernous hemangioma.
Sacral lesions: Ewing’s sarcoma, osteoblastoma, hemangiopericytoma, chordoma.
Pelvic lesions: hematocolpos.
Diskitis, or intervertebral disk inflammation, is an uncommon and poorly understood disorder that generally presents in childhood with back pain, limp, and refusal to walk. It can be associated with decreased muscle strength and/or hyporeflexia. Although diskitis is believed to be infectious, positive bacterial cultures are rarely obtained. Imaging studies show narrowing of the intervertebral disk space and/or increased uptake in the area on bone scan, and most authors advocate antibiotic therapy. Disk protrusion into the spinal canal in diskitis may underpin radicular pain and focal weakness in a small proportion of children with this condition.
In older children, especially adolescent boys, ankylosing spondylitis is an important consideration in the differential diagnosis of sciatica. There may be a history of early morning stiffness and “jelling,” associated with diminished chest excursion on examination. Sacroiliac joint misalignment can also cause back pain.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here