Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
As the name implies, pulmonary function testing provides quantification of pulmonary physiologic function. By definition this information is disease independent and static, representing a point-in-time evaluation.
Nonetheless, this information can be very helpful for building a differential diagnosis. In fact, many pulmonary diseases are clinical syndromes and without either a definitive molecular marker for disease or without unique defining functional features. These diseases therefore often require integration of histopathology with radiologic patterns, clinical context, and functional status. Pulmonary function tests (PFTs) often provide the first diagnostic tool that helps guide a clinical pulmonologist in creating a filing system for a possible differential. This chapter will focus on the basic elements that comprise a full set of PFTs. In general, these consist of lung volumes (TLC, FRC, RV; see Table 2.1 for a list of abbreviations used in this chapter), lung flows by spirometry (FVC, FEV1, FEF 25-75 ), airway resistance (R aw ), and capillary bed assessment (DLCO). Correct interpretation of PFTs requires that the patient-obtained values be read in comparison with appropriate reference values, resulting in a reporting method of “percent of predicted.” Numerous regression equations have been proposed, and used, all commonly adjust for age, sex, height, and race. The European Respiratory Society and the American Thoracic Society have published guidelines regarding the conduct of measuring and interpreting PFTs. ,
| TLC | total lung capacity | The volume in the lungs at maximal inflation | TLC = RV + VC = FRC + IC |
| FRC | functional residual capacity | The volume in the lungs at end expiration | |
| RV | residual volume | The volume that remains after full exhalation | |
| ERV | expiratory reserve volume | The volume that remains after normal tidal respiratory exhalation above the RV | |
| IRV | inspiratory reserve volume | The maximal additional inhalable volume starting after a normal tidal volume | IRV = IC − TV |
| IC | inspiratory capacity | The maximal volume for inhalation starting at FRC | IC = TV + IRV |
| IVC | inspiratory vital capacity | ||
| VC | vital capacity | The total available volume from RV to TLC | TLC − RV = VC |
| TV | tidal volume | The normal respiratory cycle volume | |
| FVC | forced vital capacity | Maximal volume attained on dynamic forced expiration beginning at TLC | |
| FEV1 | forced expiratory volume in first second | Maximal volume attained on forced exhalation in first second | |
| FEV1/FVC | the ratio of the % predicted | Reveals if increased or decreased flows | |
| NIF | negative inspiratory force | Reveals force generated on inspiration | |
| PEF | positive expiratory force | Reveals force generated on expiration | |
| DLCO | diffusion capacity of carbon monoxide | Measures the uptake of CO as surrogate for capillary beds |
Furthermore, PFTs provide quantification of the severity of the lung impairment and can be used to evaluate for change in lung function over time. This change over time in function may be age related or represent deterioration related to a disease state or, potentially, improvement related to institution of therapy.
The approach of this chapter is therefore to outline how the functional data from PFTs can help guide that differential. Fundamentally, lung physiologic function will be normal, restrictive, or obstructive. Restriction implies reduction in lung volumes—size of the lungs. Obstructive implies reduced air flows, mostly secondary to narrowing of the airways, such as in asthma, or reduced elastic recoil, such as from emphysema, leading to greater exhalation times. We will start with simple categorization of normal compared with restrictive and obstructive patterns.
Although patterns may be mixed, for purposes of organization, one must be predominant. In truth, many techniques and a plethora of available equipment make this arena very diverse. Therefore each part has pros and cons and must be considered in the interpretation of PFTs. After all the parts are established, pattern recognition is a key element, as with many composite tests in medicine.
This chapter seeks to provide a clear understanding of the fundamentals of PFTs. Basic interpretation should allow the pathologist to independently provide additional functional context to their differentials on evaluation of histopathology of lung tissue to better inform the clinician for a diagnosis.
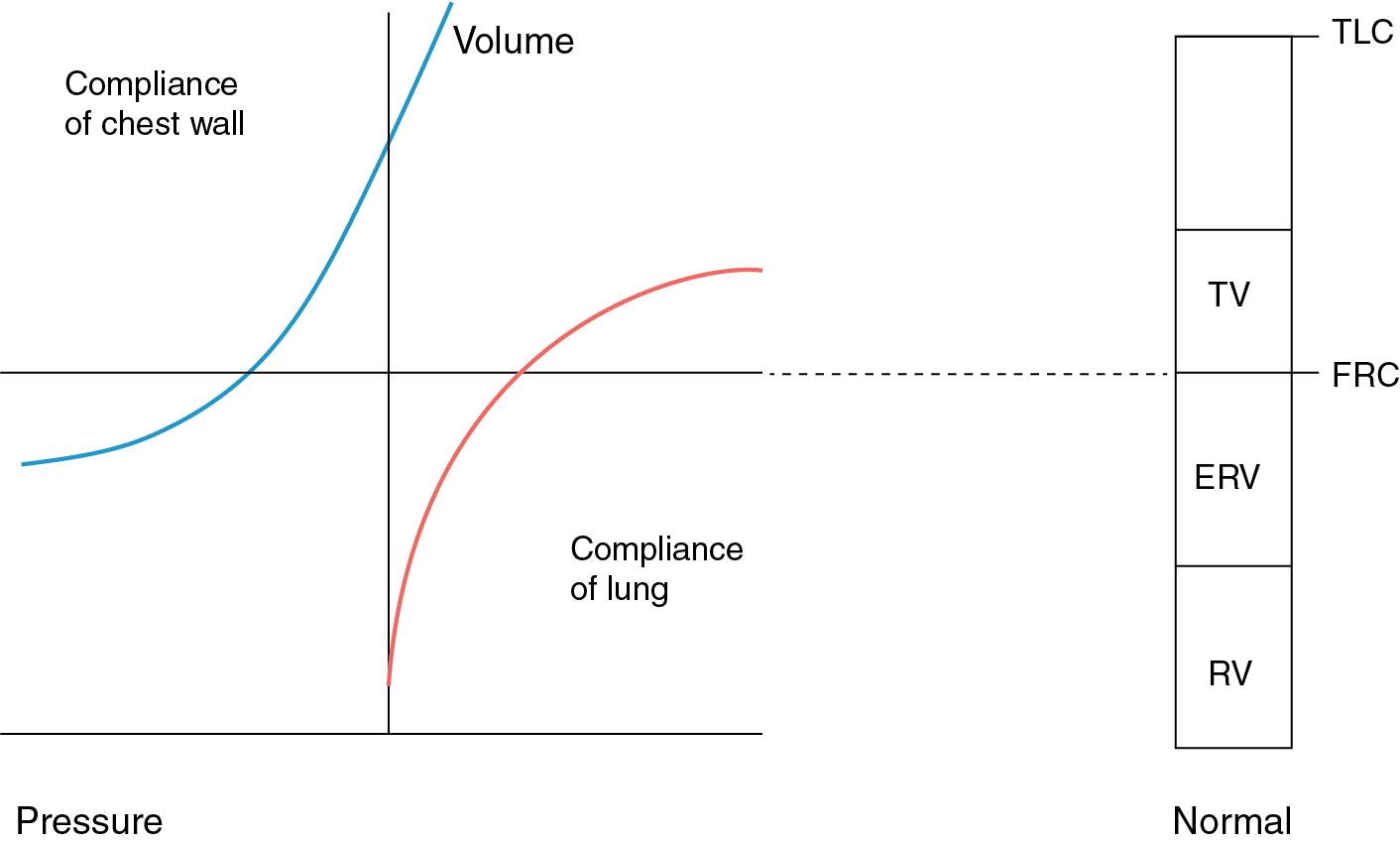
The first objective of a full set of PFTs involves determination of the size of the lungs or the lung volumes. Almost all pulmonary diseases that affect function can be divided into three simple categories. Obstructive lung diseases will all eventually lead to increased lung volumes. This is because ultimately air gets in but cannot get back out. This effect can result in static air trapping, such as in emphysema, or dynamic air trapping, as in reversible airway disease like asthma. Restrictive lung diseases will all lead to some measure of reduction in lung volumes because the lung themselves are stiffer or the chest wall either will not allow for expansion (i.e., chest wall restriction) or cannot expand fully (i.e., neuromuscular weakness ). Normal lung size implies no clinical deficit from obstruction or restriction. This leaves the pulmonary vasculature or, alternatively, causes external to the lung as potentially causal for any presenting symptomatology.
The lung volumes and lung capacities refer to volumes associated with different phases of the respiratory cycle. Although the volumes can be directly measured, the available capacities are inferred from the lung volumes.
There are a number of volumes that can be measured ( Table 2.1 and Fig. 2.1 ); however, three measures (TLC, FRC, RV) are key in determining restriction versus obstruction. The remaining volumes and capacities represent measures for compartmentalization of the respiratory cycle functions (IRV, TV, ERV, RV, IC, and VC).
There are several methodologies to attaining lung volumes. The gold standard involves body box plethysmography. This method uses Boyle’s law (PV = nRT) to measure changes in pressure to determine lung volumes, assuming the temperature is constant. Note that this measure is ideally conducted with the patient breathing normally and therefore measures the functional residual capacity (FRC). Determination of the total lung capacity and residual volume are therefore determined by simple algebraic addition of inspiratory capacity (FRC + IC = TLC) and subtraction of the vital capacity (TLC − VC = RV). Therefore these last two volumes should be interpreted in light of the quality of the IC and VC. Although this approach is the most accurate, it also involves the largest and most expensive piece of equipment. As a consequence many labs will use a closed-circuit technique with a helium dilution or nitrogen washout technique. These techniques make assumptions regarding the equilibration of gas concentrations in the portions of the lung that communicate with the breathing circuit. The key limitation of these last two approaches is that areas of the lung that involve trapped air (bullous disease in example) do not necessarily communicate with the breathing circuit and therefore result in an underestimation of the total volume.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here