Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Q35.1 What are the four main categories of psychodermatologic disorders? (Pg. 383, Fig. 35.1 )
Q35.2 What are the four major underlying psychopathologic conditions upon which the medication choice is decided (what is the ‘fifth’ nonpsychiatric category of interest)? (Pg. 384, Fig. 35.2 )
Q35.3 What is the basis of the tremendous dosing variation between patients receiving doxepin for depression or for pruritus (and how does this relate to doxepin-induced sedation)? (Pg. 386)
Q35.4 What are some of the most important measures to minimize the risk from sedation in patients receiving doxepin therapy? (Pg. 386)
Q35.5 What are several measures clinicians may use to reduce the cardiac risk of doxepin? (Pg. 386)
Q35.6 What is meant by the term ‘discontinuation symptoms’ and what are some of the therapeutic options in dealing with these symptoms? (Pgs. 387, 388, 390)
Q35.7 What are the most common adverse effects of the selective serotonin reuptake inhibitors (SSRI), and what are some measures for reducing these adverse effects? (Pg. 388)
Q35.8 Which drugs in this chapter have the risk of inducing sexual dysfunction? (Pgs. 388, 390x2, 391)
Q35.9 What are some of the risk factors for and signs of serotonin syndrome? ( Pg. 388)
Q35.10 What is the most important relatively unique adverse effect of bupropion? (Pg. 391)
Q35.11 What are some risk factors of and management options for tardive dyskinesia induced by pimozide? (Pg. 393)
Q35.12 Concerning cardiac complications because of QTc-interval prolongation, what are measures to diagnose and manage this risk with (1) pimozide, and (2) risperidone? (Pg. 393x2) (also Pg. 388)
5-Hydroxytryptamine
Adverse effect(s)
Cytochrome P-450
Electrocardiogram
Monosymptomatic hypochondriasis
Obsessive–compulsive disorder
Serotonin–norepinephrine reuptake inhibitor
Selective serotonin reuptake inhibitor
Tricyclic antidepressant
A significant proportion of patients seen in an average dermatology practice have psychosocial issues associated with their skin diseases. The most blatant cases are those such as delusions of parasitosis, in which the patients have no real skin disorder and all the skin manifestations are self-induced as a result of the underlying serious psychopathology. In addition, many patients with various common skin disorders, such as acne vulgaris, atopic dermatitis, or psoriasis, will report that their skin disorder gets worse with psychological stress. Furthermore, many patients develop emotional problems as a result of having a disfiguring skin disease.
To address these psychological issues affecting our dermatology patients, the easiest course of action would be to refer them to a psychiatrist or another mental health professional. However, these patients will frequently resist such a referral. Some of these patients may refuse to see a psychiatrist because of the perceived stigma associated with psychiatric illnesses, whereas others may refuse the referral because they lack the insight to recognize the psychological component of their skin disorder. Faced with these patients, a dermatologist has two choices. The first is to try to ‘look the other way’ and pacify the patient by providing relatively benign, but minimally effective treatments. The other option is to try to directly address the psychological/psychiatric problems.
The idea of using psychotropic medications may seem foreign to many dermatologists, given that dermatology residencies and postgraduate courses typically have limited emphasis on the practice of psychopharmacotherapy. Patients with psychodermatologic problems who refuse referral to a psychiatrist can still be greatly helped by a dermatologist who has an adequate knowledge base and the experience to prescribe selected psychotropic medications. This knowledge and experience are especially important when the alternative is for these problems to be left unattended by any physician. Although a nonpharmacologic approach to psychiatric illness may be beneficial, most dermatologists have neither the time nor the training to conduct such psychotherapy.
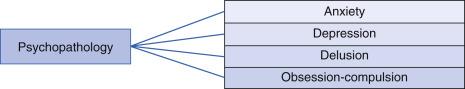
In this chapter a clinically useful way of classifying psychodermatologic cases is presented, followed by a discussion of the treatments for the major categories of psychopathology encountered in a dermatology practice. These categories include: (1) anxiety, (2) depression, (3) psychosis, and (4) obsessive–compulsive disorder (OCD).
There are at least two ways of classifying psychodermatologic cases: (1) by the category of psychodermatologic disorder, and (2) by the nature of the underlying psychopathologic conditions.
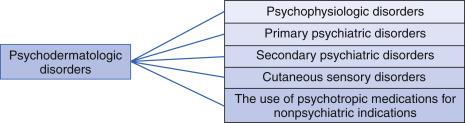
Q35.1 Other than personality disorders, in which pharmacotherapy has limited usefulness, most psychodermatologic disorders can be classified into four categories: (1) psychophysiologic disorders, (2) primary psychiatric disorders, (3) secondary psychiatric disorders, and (4) cutaneous sensory disorders. A fifth ‘category’ of use for psychotropic agents in dermatology is for purely dermatologic (i.e., nonpsychiatric or nonpsychodermatologic) cases ( Fig. 35.1 ).
Psychophysiologic disorders refer to psychodermatologic cases where a real skin disorder is exacerbated by psychological factors such as stress. Some examples of psychophysiologic conditions in dermatology include atopic dermatitis, psoriasis, acne vulgaris, lichen simplex chronicus, and hyperhidrosis. For each of these common dermatoses there are patients who experience a close chronologic association between psychologic and emotional stress and exacerbation of their skin condition, and other patients for whom their emotional state has negligible influence on the natural course of their skin disorder ( Table 35.1 ).
| Diagnosis | Proportion with Emotional Trigger (%) | Biologic Incubation Between Stress and Clinical Change |
|---|---|---|
| Hyperhidrosis | 100 | Seconds |
| Lichen simplex chronicus | 98 | Days |
| Rosacea | 94 | 2 days |
| Dyshidrosis | 76 | 2 days for vesicles |
| Atopic dermatitis | 70 | Seconds for itching |
| Urticaria | 68 | Minutes |
| Psoriasis | 62 | Days |
| Papular acne vulgaris | 55 | 2 days |
| Seborrheic dermatitis | 41 | Days |
| Fungus infection | 9 | Days |
| Nevi | 0 | |
| Basal cell carcinoma | 0 | |
| Keratoses | 0 |
Primary psychiatric disorders are conditions in which the patient has no real skin disease but presents instead with serious psychopathology; all the skin manifestations are self-induced. Some examples of primary psychiatric disorders include skin-picking disorders, delusional infestations, factitious dermatitis, and trichotillomania.
Secondary psychiatric disorders describe patients who develop emotional problems as a result of having a disfiguring skin disease, such as vitiligo, alopecia areata, or cystic acne.
Cutaneous sensory disorders refer to conditions in which the patients have only cutaneous sensory disturbances, such as itching, burning, stinging, crawling, biting, or any other disagreeable sensations on the skin. These symptoms occur in the absence of a primary skin disorder or an identifiable underlying medical or neurologic condition. A psychiatric diagnosis may or may not coexist. Some examples are cutaneous dysesthesia and formication.
It is helpful to classify a psychodermatologic condition into one of these four categories because they help guide physicians to select the optimal interpersonal approach for a given patient. For example, patients with psychophysiologic disorders or secondary psychiatric disorders usually welcome the opportunity to discuss their psychologic status. In contrast, some patients with primary psychiatric disorders are often extremely resistant to talking about their situation in psychological terms. In addition, because the clinician is dealing with the skin and the mind simultaneously in psychophysiologic cases, the simultaneous use of both somatic (i.e., dermatologic) and psychotropic therapeutic modalities may be more effective than either approach alone. In dealing with primary psychiatric cases somatic modalities are at best supportive, and are more likely therapeutically useless. For secondary psychiatric cases the approach may be somatic, such as resorting to a more powerful therapeutic option, because of the great emotional distress suffered by the patient. An example would be the use of isotretinoin for borderline acne where severe psychosocial or occupational impact warrants its use. A psychological approach for secondary psychiatric cases may also be helpful, such as a referral to a support group such as the National Psoriasis Foundation or the National Alopecia Areata Foundation. Lastly, with cutaneous sensory disorders, successful treatment often involves a highly empiric approach to therapy, with therapeutic trials of various psychotropic medications having analgesic or antipruritic effect, or both.
The last category of psychodermatologic conditions involves clinical situations where psychotropic medications are more efficacious in treating certain dermatologic conditions than ‘traditional’ therapeutic agents used in dermatology. For example, the antidepressant doxepin (Sinequan) is a more powerful antipruritic agent than most traditional antihistamines such as diphenhydramine (Benadryl) and hydroxyzine (Atarax).
In the four categories of psychodermatologic disorders discussed previously, the choice of psychotropic medication is based on the nature of the underlying psychopathology involved. Q35.2 Most psychodermatologic patients fall primarily into one of the four underlying psychiatric diagnoses: (1) anxiety, (2) depression, (3) psychosis, and (4) obsessive–compulsive disorder ( Fig. 35.2 ). For example, if the underlying psychopathology involves depression, an antidepressant would be a logical choice. It does not matter whether the patient presents with a primary psychiatric disorder (e.g., skin-picking disorder or body dysmorphic disorder resulting from depression), a psychophysiologic disorder (e.g., psoriasis exacerbated by depression), or secondary depression resulting from disfigurement. As long as the underlying psychopathology is depression, an antidepressant would be the most appropriate choice. The same holds for anxiety, psychosis, and OCD, where the use of antianxiety agents, antipsychotic agents, and anti-OCD agents, respectively, may be indicated.
Any one of the psychopathologies, such as anxiety, depression, psychosis, or OCD, can be found in any one of the four previously discussed categories of psychodermatologic disorders. The determination of the category of psychodermatologic disorders and the decision about the underlying psychiatric diagnosis are made independently. Also, it is important to recognize that dermatologic labels used to diagnose psychodermatologic patients may not give any information as to the true nature of the underlying psychopathology involved. For example, when a patient presents with self-induced skin lesions, the diagnosis of ‘neurotic excoriations’ may be given. Even though this term contains the word ‘neurotic,’ the nature of the underlying psychopathology may not involve neurosis. Patients may excoriate their skin in response to a variety of other psychopathologies, such as anxiety, depression, or OCD. Therefore, for each individual case it is important to move beyond the dermatologic label to assess the exact nature of the underlying psychopathology to guide the psychopharmacologic therapy.
Patients with anxiety disorders report excessive anxiety and worry, which may revolve around valid concerns about money, jobs, marriage, and health. Patients may also report stress, restlessness, difficulty concentrating or their mind going blank, and irritability. Associated physical symptoms may include muscle tension, palpitations, sweaty palms, and sleep disturbances ( Box 35.1 ). The subjective anxiety and associated physical symptoms are difficult to control and cause significant distress or impairment in functioning. Anxiety may also exacerbate obsessive–compulsive tendencies such as skin picking, or cause flares of pruritus or flushing.
Excessive anxiety and worry
Restlessness or feeling ‘keyed up’ or ‘on edge’
Difficulty concentrating or mind going blank
Irritability
Muscle tension
‘Stress’
Sleep disturbance (difficulty falling or staying asleep; or restless, unsatisfying sleep)
Dizziness
Sweating
Palpitations
Abdominal complaints
Frequent urination
In general, psychodermatologic cases involving anxiety can often be divided into two groups: acute versus chronic anxiety. The acute and time-limited episode of anxiety usually involves a specific situational stress such as increasing demand at work, interpersonal difficulty, or a financial crisis. Unlike patients with chronic anxiety, many of these patients with acute situational anxiety have adequate coping skills and usually recover from the ‘crisis’ after a few weeks. However, this short period of stress can be long enough to exacerbate their skin disorder. The use of a quick-acting anxiolytic medication may be indicated for a few weeks to avert a flare of the skin condition and improve mental stability until the patient recovers from the crisis. The decision as to the treatment of choice for psychodermatologic cases involving anxiety should take into account whether the anxiety is acute (short-term) or chronic.
For the treatment of acute and self-limited stress , an antianxiety agent with a quick onset of action is indicated. Benzodiazepines are especially useful in the management of acute situational anxiety as the drug takes effect immediately and can almost always relieve anxiety if given in adequate doses. Alprazolam (Xanax) is a prototypical quick-acting benzodiazepine. Usually half of a 0.25 mg tablet (0.125 mg), up to four times daily on an as-needed basis, is adequate to control acute anxiety. The dosage can be titrated upward; however, for dermatologic patients the authors rarely prescribe more than 0.25 mg three times daily. Because of the potential risk of addiction with long-term use, the physician should try to limit the duration of the treatment to no more than 3 to 4 weeks. In many cases the situational stress resolves within this period.
With short-term use, sedation is usually the only adverse effect (AE) encountered, and this usually subsides (tolerance) after several days of treatment, or can be controlled by dosage adjustment. It may be helpful for patients to take their initial dose at home in the early evening to see how it affects them while awake. Alprazolam differs from the older benzodiazepines, such as diazepam (Valium) or chlordiazepoxide (Librium), because the half-life is short and predictable, and most/all of the previous dose is eliminated before the next dose. Even though this feature of short-acting benzodiazepines makes them much safer, with less drug accumulating in the body over time, it also requires the medication to be slowly tapered when the therapeutic course is complete. Even though the risk of physical dependency is extremely small with short-term usage, patients who stop alprazolam ‘cold turkey’ may experience a ‘rebound’ anxiety beyond the baseline level of anxiety. Alprazolam may have a unique antidepressant effect, whereas most other benzodiazepines generally have a depressant effect.
Buspirone (BuSpar) is a nonsedating anxiolytic medication that does not cause dependency. Buspirone is a partial agonist of the 5-HT (5-hydroxytryptamine) 1A receptor. The major drawback of this drug is that its onset of action is delayed for 2 to 4 weeks, so that buspirone cannot be used on an as-needed basis and is not appropriate for the treatment of acute situational stress.
The starting dose is 7.5 mg twice daily, subsequently increasing to 15 mg twice daily after 1 week, up to a maximum of 60 mg daily if needed. Most patients respond at a dosage between 15 and 30 mg daily. The 15- and 30-mg tablets are scored to allow more precise dosing. Buspirone is generally well tolerated. The most common AE are nausea, headache, dizziness, and fatigue, although most patients experience no AE.
Antidepressants such as paroxetine (Paxil 25–50 mg daily) and venlafaxine extended release (Effexor XR; 75 and 150 mg daily) have also been shown to be useful for the treatment of chronic anxiety. These antidepressants are discussed in more detail later in this chapter.
Depression is frequently encountered in a dermatology practice. It can have subjective and physiologic manifestations. Subjective manifestations include depressed mood, crying spells, anhedonia (i.e., markedly diminished interest or pleasure in activities), and excessive guilt, along with feelings of helplessness, hopelessness, and worthlessness. The physiologic manifestations of depression include insomnia or hypersomnia, loss of appetite or hyperphagia, difficulty with concentration, memory loss, fatigue, and lack of energy ( Box 35.2 ). The easiest way to make a diagnosis of depression is to ask the patient questions such as ‘Are you depressed?’ or ‘Have you been feeling very discouraged?’ It is not unusual, however, for many patients to deny the fact that they are experiencing depression, because they use denial as the primary method for coping with their depression. Frequently, this denial takes the form of somatization, where they consciously or unconsciously focus on vague, nonspecific, or exaggerated physical concerns to diminish their awareness of feeling depressed.
Depressed mood
Anhedonia (i.e., markedly diminished interest or pleasure in activities)
Significant weight loss when not dieting, weight gain, or decrease or increase in appetite
Insomnia or hypersomnia
Psychomotor agitation or retardation
Fatigue, lack of energy
Helplessness, hopelessness, worthlessness
Excessive guilt
Difficulty with concentration, memory loss
Suicidal ideation/plan
Crying spells (i.e., finding oneself tearful for no reason or with minimal provocation)
Somatization (i.e., preoccupation with vague, nonspecific or exaggerated physical concerns but not of delusional intensity)
When one encounters patients who deny their depression, it is frequently helpful to change the line of questioning to general medical inquiries. Patients are usually not defensive in responding to questions about physiologic manifestations of depression, such as insomnia and loss of appetite. Once the clinician is quite certain that the patient is suffering from depression, one should ask open-ended questions regarding his or her personal, occupational, or financial situation in a sympathetic, nonjudgmental way. It is not unusual for depressed patients to come to realize the presence of depression as they talk about the difficulties in their lives. Once such an understanding is reached, it is much easier to obtain the patient’s cooperation in treating underlying depression.
There are several classes of antidepressant agents to choose from. Currently available antidepressants are generally equally effective, with 60% to 80% of patients responding adequately. Full clinical response is typically gradual, with the initial response beginning about 2 to 3 weeks after the therapeutic dosage is reached. Typically, a minimum of 6 weeks of full-dose treatment is required before full therapeutic effectiveness is reached. AE profiles and toxicity vary substantially, so the choice of an antidepressant medication depends primarily on tolerability and safety. The antidepressants can be broadly separated into tricyclic and nontricyclic ( Table 35.2 ).
| Generic Name | Trade Name | Generic Available | Manufacturer | Drug Category | Tablet/Capsule Sizes | Standard Dosage Range |
|---|---|---|---|---|---|---|
| Doxepin | Sinequan | Yes | Pfizer | Tricyclic antidepressant | 10, 25, 50, 75, 100, 150 mg a | 100–300 mg QHS (depression) 10–100 mg QHS (pruritus) |
| Amitriptyline | Elavil | Yes | Astra-Zeneca | Tricyclic antidepressant | 10, 25, 50, 75, 100, 150 mg | 100–300 mg QHS (depression) 25-75 mg QHS (PHN) |
| Bupropion | Wellbutrin Wellbutrin SR Wellbutrin XL |
Yes | GlaxoSmithKline | Atypical antidepressant | 75, 100 mg SR 100, 150, 200 mg XR 150, 300 mg |
150–300 mg daily |
| Venlafaxine | Effexor Effexor XR |
Yes | Wyeth-Ayerst | Serotonin–norepinephrine reuptake inhibitor | 25, 37.5, 50, 75, 100 mg XR 37.5, 75, 150 mg |
75–225 mg daily |
| Mirtazapine | Remeron | Yes | Organon | Atypical antidepressant | 7.5, 15, 30, 45 mg b | 15–45 mg nightly |
a Doxepin also has liquid formulation—10 mg/mL.
b Mirtazapine also has a disintegrating oral tablet formulation.
Table 35.2 lists general features and key pharmacologic concepts of antidepressant medications.
The tricyclic antidepressant (TCA) doxepin is probably the ideal agent for the treatment of depressed patients with neurotic excoriations. In addition to its antidepressant effects, doxepin has strong antipruritic effects because it is a very powerful H 1 antihistamine. To stop the excoriating behavior, it is important to treat the patient’s depression and to put an end to the ‘itch–scratch cycle.’ Moreover, the majority of depressed patients who present with excoriations appear to be suffering from an agitated depression, in which they paradoxically become more restless, angry, and argumentative when depressed. For these patients, the most common AE of doxepin—sedation—can actually be beneficial, through taking doxepin about 1 hour before bedtime.
Probably the only TCA still worth considering as a possible first-line antidepressant in dermatology is doxepin, because of its combined antipruritic and antidepressant effects. The usual starting dosage of doxepin for depression is 25 mg at bedtime. The dosage can be titrated by 10 to 25 mg increments every 5 to 7 days, as tolerated, up to the maximum range of 75 to 100 mg. The therapeutic range for depression—anywhere from 100 to 300 mg daily—is usually not well tolerated by most dermatologic patients. Although it may take 6 to 8 weeks or more to reach the antidepressive therapeutic dosage for doxepin, other effects, such as antipruritic effects, calming of the patient, and improvement in insomnia, generally improve right away. Q35.3 There can be at least a 20-fold difference in serum trough blood levels among individuals who are taking the same dose of doxepin. The underlying explanation for this wide dosing range relates to the metabolism of doxepin by cytochrome P-450 (CYP)2D6, which has a significant polymorphism (‘poor,’ ‘intermediate,’ ‘rapid,’ and ‘ultrarapid’ metabolizers). Given this wide interindividual variation, patients who fail to show a therapeutic response despite taking a relatively large dose of doxepin for several weeks should have a serum trough doxepin level tested (i.e., at least 12 hours after the last dose) to see whether the drug level is within (or at least near) the therapeutic range for depression. Table 35.3 lists drug interactions for TCA. Box 35.3 lists the risk profile for TCA.
| Drug Category | Drug Examples | Comments |
|---|---|---|
| Relatively High-Risk Drug Interactions a | ||
| SSRI antidepressants | Paroxetine, fluoxetine | Primary CYP2D6 inhibitors of drug group; doxepin/amitriptyline CYP2D6 substrates ↑ TCA levels |
| NSRI antidepressants | Venlafaxine > bupropion | Same |
| Allylamine antifungals | Terbinafine | Same |
| H 1 antihistamines | Diphenhydramine | Same |
| MAOI | All TCA at risk | May induce hyperpyretic crisis with CNS and cardiovascular complications |
| Drugs prolong QTc interval | (See Chapter 66 ) | Greatest concern pimozide , certain SSRI antidepressants; macrolides (erythromycin, clarithromycin), fluoroquinolones (gatifloxacin, moxifloxacin), antidysrhythmics , sotalol , others |
| Sedating drugs | Multiple drug classes | Excessive sedation potential in combination (ethosuximide, narcotics, alcohol, cannabinoids, sedating H 1 antihistamines, anticholinergics, antidepressants, antipsychotics, benzodiazepines, etc.) |
| H 2 antihistamines | Cimetidine (no others in drug class) | Cimetidine weak CYP2D6 inhibitor—may ↑ TCA drug levels somewhat |
| Anticholinergic drugs | Wide variety drug classes | May ↑ dry mouth, constipation, dry eyes, narrow angle glaucoma risks of TCA; most common dermatologic anticholinergic treatment glycopyrollate, oxybutynin |
| Lower-Risk Drug Interactions | ||
| Anticonvulsants | Phenytoin, carbamazepine, phenobarbital, primidone | None are CYP2D6 inducers (some TCA CYP2D6 substrates); doxepin is CYP2C9 and CYP2C19 minor substrate (amitriptyline CYP2C19 minor substrate) → these anticonvulsants may ↓ TCA efficacy |
| Rifamycins | Rifampin > rifabutin, rifapentine | As above CYP2C9/19 substrates; amitriptyline weak CYP3A4 substrate → may ↓ TCA efficacy |
| Supplements | St. John’s wort | Is not a CYP2D6 inducer (TCA major substrate), minor effect ↓ TCA levels via CYP2C9/19 |
a Overall highest-risk drug interactions indicated in bold italics.
| Contraindications | |
| Hypersensitivity to drug or components of formulations Acute recovery phase following MI |
Concomitant MAOI Glaucoma, urinary retention (for doxepin) |
| Boxed Warnings | |
| Suicidal thinking and behavior (label for all antidepressants) | |
| Warnings & Precautions a | |
| Psychiatric a Suicidal thinking and behavior a Discontinuation syndrome Hypomania and mania Sleep-related activities—driving, having sex, cooking, eating Anticholinergic Effects a Dry mouth/eyes, constipation, urine retention a Excessive sedation a Eyes—pupillary dilation and narrow angle glaucoma Hypersensitivity reactions Allergic ‘rashes’ with/without fever |
Cardiovascular a Orthostatic hypotension—caution in elderly falls at nighttime a Caution in patients with cardiovascular disorders Metabolic a Altered appetite and weight Caution in patients with diabetes mellitus Neurologic Neuroleptic malignant syndrome Caution in patients with prior seizures Extrapyramidal symptoms |
| Pregnancy Prescribing Status | |
| Traditional US Food and Drug Administration rating —category C | Newer rating b —low Risk |
a Under “Warnings & Precautions” these adverse effects can be considered relatively high risk or important clinical scenarios to avoid.
b See Chapter 65 Dermatologic Drugs During Pregnancy and Lactation, for detailed explanations of terms for “Newer rating” based on 2015 US Food and Drug Administration rulings.
The most common AE of doxepin is sedation. Q35.4 The sedative effect of doxepin can usually be minimized by taking it at bedtime. More persistent sedation may require lowering the dose or changing the time of administration of doxepin. For example, if the patient complains of difficulty waking up in the morning, this morning sedation can usually be overcome by taking doxepin earlier than bedtime (at least 1–2 hours in advance). Alternatively, the dose may be divided such that the patient may take some of the dose when he or she gets home, taking the rest at least 1 to 2 hours before bedtime. This way the patient is less likely to experience an excessively high peak serum level, and the resultant sedation, the next morning. Patients sensitive to the sedative effects and the elderly may start with an initial doxepin dose of 10 mg or lower. The other AE of doxepin are similar to those of other TCA including cardiac conduction disturbances, weight gain, orthostatic hypotension, and anticholinergic AE such as dry mouth, blurry vision, constipation, and urinary retention.
Q35.5 In terms of the cardiac conduction disturbance, the most prominent effect of a TCA, such as doxepin, is to prolong the QTc interval. Thus, older patients or any patient with a history of cardiac conduction disturbance should have a pretreatment electrocardiogram (ECG) to rule out the presence of prolonged QTc interval. In addition, an ECG should be repeated to rule out dysrhythmia if doxepin is used in dosages of 100 mg daily or higher.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here