Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Psychiatric disorders, also known as mental illnesses, are extraordinarily common and have a profound impact on well-being and functional status. Collectively, psychiatric disorders account for more aggregate disability than do disorders involving any other organ system, with depression alone being second only to cardiovascular disorders.
Psychiatric disorders are defined as disorders of the psyche—that is, conditions that affect thoughts, feelings, or behaviors. By definition, such mental disturbances must be sufficient to produce significant distress in the patient or impairment in role or other functioning. Because the pathogeneses of most psychiatric disorders are incompletely understood, classification is based on clinical syndromes that are defined by diagnostic criteria with high interrater reliability. To achieve that reliability, the criteria emphasize discrete reportable or observable symptoms and signs. Interestingly, however, many underlying pathophysiologic mechanisms probably cut across these descriptive diagnostic categories, although current knowledge of such mechanisms rarely directly informs predictions of course or clinical decision-making.
Because many psychiatric disorders result from the direct influence of neurologic conditions, systemic diseases, or drugs on brain functioning, assessment of any new or worsened psychiatric condition must include evaluation for their potential contributions ( Table 362-1 ). Delirium ( Chapter 361 ) and dementia ( Chapter 371 ), which are neurocognitive disorders defined by impairment in intellectual functions such as attention, memory, or language, are always the result of neurologic abnormalities, systemic illnesses, or drugs. Although intellectual impairment is the hallmark of neurocognitive disorders, these conditions also may manifest as alterations in other aspects of mental status, including mood, thought content, thought process, and behavior.
| CENTRAL NERVOUS SYSTEM DISEASES |
| Trauma Tumor Toxins Seizures Vascular Infections Genetic/congenital malformations Demyelinating diseases Neurodegenerative diseases Hydrocephalus |
| SYSTEMIC DISEASES |
| Cardiovascular Pulmonary Endocrine Metabolic Nutritional Infections Cancer |
| DRUGS (e.g., recreational, prescription, or over-the-counter drugs) |
| Drug intoxication Drug withdrawal |
If a noncognitive psychiatric syndrome is caused by an identifiable underlying condition, it is known as a secondary psychiatric disorder (e.g., “major depression due to hypothyroidism”).
The major non-secondary, non-cognitive psychiatric syndromes ( Table 362-2 ) can coexist with multiple syndromes. Mood disorders are categorized as either depressive (also termed unipolar , and characterized by depressive episodes only) or bipolar (characterized by manic or hypomanic episodes, typically with depressive episodes as well). For example, a patient suffering major depression with psychotic features by definition will have depressive and psychotic syndromes simultaneously, and the same patient may also manifest anxiety or other syndromes. Addictive disorders are considered in Chapters 364 and 365 .
| SYNDROME | MAIN SYMPTOMS AND SIGNS | MAY OCCUR AS PART OF THESE DISORDER CATEGORIES |
|---|---|---|
| Neurocognitive/
cognitive |
Deficits in intellectual functions (e.g., level of consciousness, orientation, attention, memory, language, praxis, visuospatial, executive functions) | Neurocognitive disorders (delirium, dementia, amnesia, aphasia) Intellectual disability (if onset in childhood) |
| Depressive | Lowered mood, anhedonia, negativistic thoughts, neurovegetative symptoms and signs | Neurocognitive disorders Depressive disorders (primary or secondary) Bipolar disorders (primary or secondary) Psychotic disorders (schizoaffective disorder) |
| Manic | Elevated or irritable mood, grandiosity, goal-directed hyperactivity with increased energy, pressured speech, decreased sleep need | Neurocognitive disorders Bipolar disorder (primary or secondary) Psychotic disorders (schizoaffective disorder) |
| Anxiety | All include anxious mood and associated physiologic symptoms (e.g., palpitations, tremors, diaphoresis); may include various types of dysfunctional thoughts (e.g., catastrophic fears, obsessions, flashbacks) and behavior (e.g., compulsions, avoidance behavior) | Neurocognitive disorders Mood disorders (bipolar or depressive) (primary or secondary) Psychotic disorders (primary or secondary) Trauma- and stressor-related disorders Anxiety disorders (primary or secondary) Obsessive-compulsive and related disorders |
| Psychotic | Impairments in reality testing: delusions, hallucinations, thought process derailments | Neurocognitive disorders Depressive disorders (primary or secondary) Bipolar disorders (primary or secondary) Psychotic (schizophrenia and related) disorders |
| Somatic symptom syndromes | Somatic symptoms with associated distressing thoughts, feelings, or behaviors | Depressive disorders (primary or secondary) Bipolar disorders (primary or secondary) Anxiety disorders (primary or secondary) Obsessive-compulsive and related disorders Trauma- and stressor-related disorders Somatic symptom disorders |
| Personality pathology | Enduring patterns of dysfunctional emotional regulation, thought patterns, interpersonal behavior, impulse regulation | Neurocognitive disorders (dementia) Personality change due to another medical condition Personality disorders |
It is common for persons who suffer from mental disorders to meet the diagnostic criteria for more than one condition. Such comorbidity may reflect the limitations of current diagnostic approaches based on signs and symptoms rather than pathogenesis. At the individual level, the behavioral manifestations of psychiatric disorders are variable and could meet multiple diagnostic criteria with overlapping symptoms. Furthermore, comorbidity of psychiatric disorders overlaying other medical conditions also is common, probably reflecting complex bidirectional causal relationships between physical and mental illnesses. Such comorbidity often worsens the prognosis for both conditions.
The most common psychiatric comorbidities encountered in general medical settings are substance abuse ( Chapters 364 and 365 ) and depressive disorders. More than 50% of patients who seek treatment for substance use disorders have past or current diagnoses of depression or an anxiety disorder. Substance abuse is also common among bipolar disorder patients. These overlapping neurobiologic conditions may be caused by a link between addictive behavior and mood disorders, or patients with mood disorders may use drugs and alcohol in an attempt to self-medicate their emotional distress. Substance abuse generally will exacerbate a mood disorder, and the overlapping clinical manifestations and mutually reinforcing clinical course often make the assessment and treatment of patients with comorbid substance use and mood disorder challenging. Generally the treatment plan should address both the mood disorder and the addictive behaviors.
Substance use is also common in patients with psychotic disorders (e.g., schizophrenia, schizoaffective disorder). Psychoactive substances such as hallucinogens and stimulants often mimic or exacerbate psychotic symptoms that are difficult to separate from underlying psychotic disorders. Regardless of cause, acute treatment of psychosis and accompanying agitation requires judicious use of antipsychotic medication. It is also crucial to ensure the cessation of active substance use while treating acute psychosis and to maintain abstinence, in part by encouraging adherence to medications and psychosocial treatments for the psychotic disorder.
Acute treatments in psychiatry are intended to reduce or eliminate symptoms, thereby reducing the patient’s distress and dysfunction, and, for many patients, averting suicidal behavior. Maintenance therapies reduce the frequency or severity of recurrent episodes. Pharmacotherapy is an evidence-based mainstay of the treatment of many psychiatric conditions. The evidence for a number of forms of psychotherapy administered in individual, group, or family modalities also strongly support their use as primary treatment or co-treatment of many conditions. Other psychosocial interventions, ranging from self-help groups to the use of structured treatment or residential programs, are often important components of treatment. Nonpharmacologic evidence-based somatic therapies include electroconvulsive therapy, light therapy, and vagal nerve stimulation for particular forms of major depression. Other neuromodulatory treatment methods being studied for selected patients with severe depressive or obsessive-compulsive disorders include repetitive transcranial magnetic stimulation, transcranial direct-current stimulation, and deep brain stimulation.
Major depressive disorder is characterized by one or more episodes of idiopathic major depressive syndrome ( Table 362-3 ). This disorder should be distinguished from the generally milder dysthymic, cyclothymic, and grief disorders (see later).
| DIAGNOSTIC CRITERIA (a minimum of five symptoms must be present for a minimum of 2 consecutive weeks) |
| Depressed mood (may be irritable mood in children and adolescents) most of the day, nearly every day, OR Markedly diminished interest or pleasure most of the day, nearly every day AND Weight loss or gain, or change in appetite (decrease or increase) nearly every day Change in sleep (insomnia or hypersomnia) nearly every day Psychomotor agitation or retardation nearly every day Fatigue or loss of energy nearly every day Feeling of worthlessness or guilt nearly every day Diminished concentration or indecisiveness nearly every day Recurrent thoughts of death or suicidal ideation, or a suicide attempt, or a specific suicide plan |
| MNEMONIC TO AID RECALL OF DIAGNOSTIC CRITERIA: “SIG: E CAPS” (i.e., prescribe energy capsules) along with depressed mood |
| S leep change I nterests decreased G uilt E nergy decreased C oncentration decreased A ppetite/weight disturbance P sychomotor changes S uicide thoughts |
| DEPRESSIVE SYMPTOMS/SIGNS GROUPED CONCEPTUALLY, WITH ADDITIONAL COMMON PHENOMENA |
| Emotional |
| Depressed mood, sadness, tearfulness Irritability (seen in all ages, perhaps most commonly in children/adolescents and the elderly) Anxiety Loss of interests or pleasure (anhedonia) |
| Ideational |
| Worthlessness/lowered self-esteem Guilt Hopelessness/nihilism Helplessness Thoughts of death, dying, suicide |
| Somatic/Neurovegetative |
| Change in appetite/weight Change in sleep Anergia Decreased libido Trouble concentrating Diurnal variation in symptoms (mornings—worst pattern is most characteristic) |
| Other |
| Ruminative thinking (tendency to dwell on one [negativistic] theme) Somatic symptoms or somatic worry Psychotic symptoms (negativistic delusions most characteristic)—defines the subtype “Major Depression with Psychotic Features” |
In the United States, major depression has a 12-month prevalence of approximately 7%, and it is at least 1.5 times more common in females than males, partly but not fully explained by the 6 to 13% prevalence of postpartum depression. Lifetime prevalence of depression is up to 10% in males and 20 to 25% in females. New depressive episodes have an annual incidence of approximately 3%. Depression is associated with more than twice as much disability in midlife as any other medical condition, and its overall cumulative burden is greater than that from all but cardiovascular disorders. The economic impact is also enormous, with U.S. estimates of annual costs for depression exceeding $12 billion for treatment, $8 billion for associated morbidity, and $33 billion for lost earnings and work productivity.
Major depression is not a single disease entity but rather a heterogeneous group of conditions with multiple pathogenic mechanisms. It is both multifactorial and polygenic: genetic factors account for approximately 40% of the risk for depression, but multiple gene loci, most of which are currently unknown, are probably involved in a complex interplay with developmental and environmental influences. Alterations in the brain’s noradrenergic and serotonergic systems are likely related to the efficacy of current antidepressant medications. The hypothalamic–pituitary–adrenal axis is hyperactive in depression, as evidenced by a nonsuppressed response to the dexamethasone suppression test, although this test is too insensitive and nonspecific for clinical use as a diagnostic tool. Neuroimaging studies in subjects with depression show an array of findings, including smaller hippocampal volumes that may be the result of exposure to chronically elevated cortisol levels, and altered cerebral metabolic activity in regions including frontal-striatal circuitry and the anterior cingulate cortex. Cognitive psychology studies have demonstrated dysfunctional patterns of negative thinking, with distorted thoughts about self, the future, and the environment. These cognitive distortions are both risk markers for the onset of depression and manifest in worsened form during depressive episodes. Impairments in the quality or number of social relationships, and stressful life events, particularly exit events such as deaths, separations, or functional impairment, are powerfully associated with depression as well.
The symptoms of depression (see Table 362-3 ) may be conceptually grouped as alterations in emotions, ideation (i.e., thought content), and somatic/neurovegetative functioning. Importantly, patients with depressive illness may be seen without a depressed mood, albeit by definition they then must have loss of interest or pleasure in their usually desired activities. In addition to the core symptoms that define the depressive syndrome, depressed patients also may exhibit prominent anxiety, irritability, or somatization. Although the mildest forms of major depression in the community may remit spontaneously within a few months without medical care, patients may have persistent symptoms for months or years, too often without seeking treatment.
The diagnosis is made clinically by elicitation of findings from the history and mental status examination to determine the presence of major depressive syndrome. The differential diagnosis includes other idiopathic disorders with episodes of major depression, such as bipolar disorder (distinguished by a history of manic episodes) and schizoaffective disorder (distinguished by a history of psychotic episodes in the absence of depression). Major depression may manifest as part of delirium or dementia, and secondary depression also commonly accompanies serious medical illnesses; these comorbid conditions require careful, well-coordinated care. Screening instruments (see Table 361-3 in Chapter 361 ) can help identify cases of depression, and screening of adults is recommended by the U.S. Preventive Services Task Force. For example, using the two-item version of the Patient Health Questionnaire, the screener asks the patient the following questions: Over the past 2 weeks, how often have you (1) had little interest or pleasure in doing things, or (2) been feeling down, depressed, or hopeless? Responses for each question are scored as follows: 0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day. A score of 3 points or higher on the two-item screen is associated with 75% probability of having a depressive disorder.
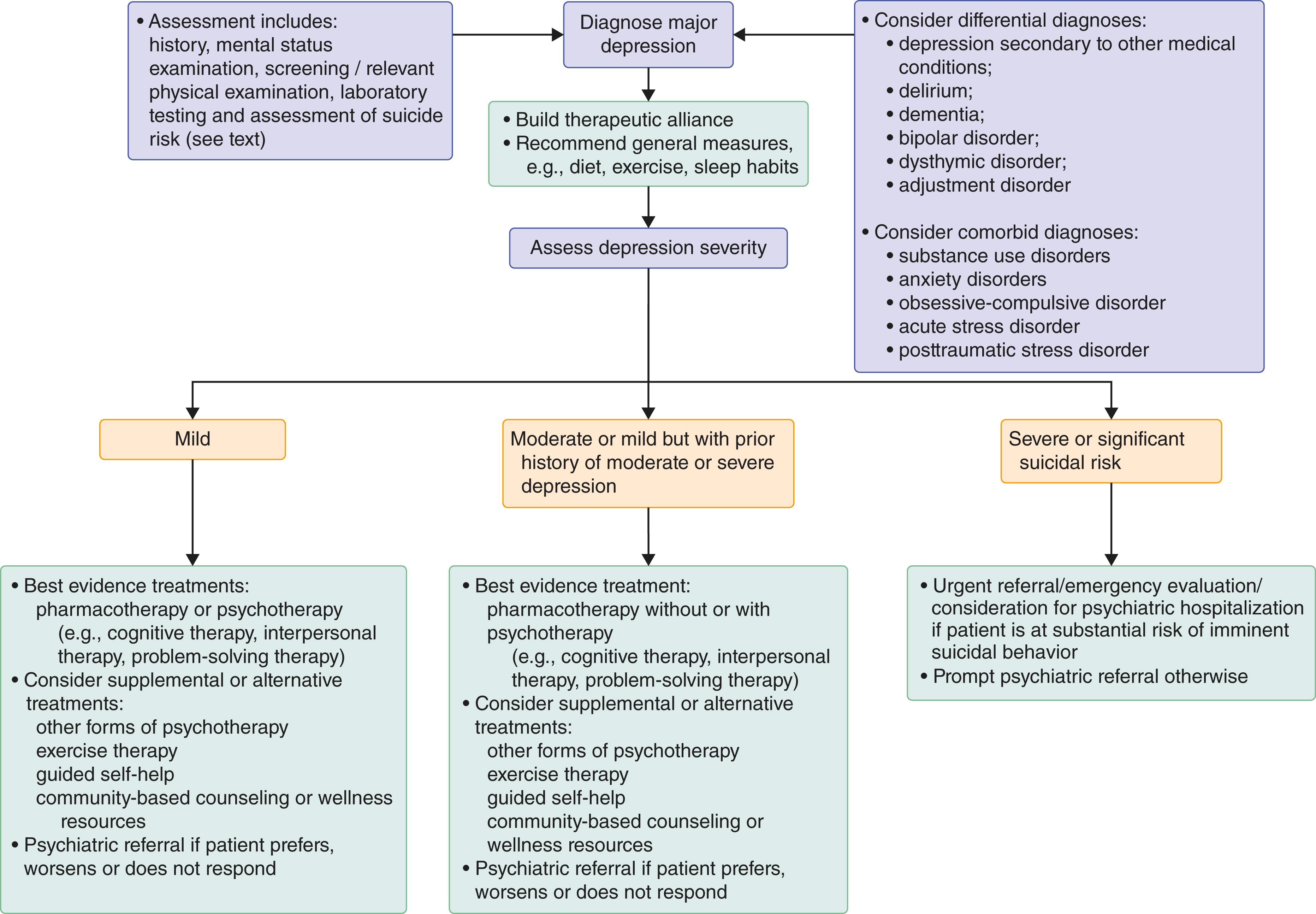
The approach to treatment begins with an assessment of the severity of the depression, based on the number and intensity of symptoms as well as the degree of functional impairment. Although approaches to distinguishing severe from mild to moderate major depression vary, severe depression generally produces substantial dysfunction in all aspects of the patient’s life and often includes so-called melancholic features, for example, nonreactive mood and profound somatic/neurovegetative symptoms ( Fig. 362-1 ).
The three phases of treatment are (1) acute, in which treatment is provided to resolve the major depressive episode; (2) continuation, in which the acute treatment is continued for 6 to 12 months to prevent relapse; and (3) maintenance, for those with two to three or more episodes of recurrent depression, for whom treatment is maintained indefinitely to reduce the frequency and severity of future recurrences.
Antidepressant medications are effective for acute, continuation, and maintenance therapy. Some patients have episodes of hypomania (e.g., low-level manic symptoms without substantial functional impairment and without psychosis) accompanied by episodes of major depression. However, these patients typically seek care during depressive episodes rather than during hypomania.
Based on the patient’s preference, psychotherapy rather than medication may be the initial treatment of mild to moderate depression, perhaps especially for individuals with prominent psychosocial stressors. Focused psychotherapies ( Table 362-4 ), which are more efficacious than usual care and equivalent to medications when used for patients in primary care settings. Involvement of family members for education, support, and sometimes formal family therapy may be an important adjunctive or primary therapeutic approach.
| NAME OF PSYCHOTHERAPY | APPROACH |
|---|---|
| Cognitive psychotherapy | Identify and correct negativistic patterns of thinking |
| Interpersonal psychotherapy | Identify and work through role transitions or interpersonal losses, conflicts, or deficits |
| Problem-solving therapy | Identify and prioritize situational problems; plan and implement strategies to deal with problems with the best combination of high priority and high addressability |
| Psychodynamic psychotherapy | Use therapeutic relationship to maximize use of the healthiest defense mechanisms and coping strategies |
Meta-analyses demonstrate that antidepressant medications ( Table 362-5 ) are safe and effective for treating depression, including when used appropriately in patients who have comorbid medical conditions. Furthermore, the combination of medications plus psychotherapy may be more effective than medication alone for treatment-resistant major depression. Because antidepressant medications typically do not begin to improve symptoms for at least 1 to 2 weeks, with maximal benefit accruing up to at least 6 to 8 weeks, it is crucial to see patients regularly (every 1 to 2 weeks initially) to monitor their clinical status, provide support and education, and foster adherence.
| NAME OF CLASS/SPECIFIC MEDICATION | IMMEDIATE MECHANISM OF ACTION | INITIAL ADULT DOSE | TARGET ADULT DOSE RANGE † | SIDE EFFECTS | COMMENTS |
|---|---|---|---|---|---|
| Selective serotonin reuptake inhibitors (SSRIs) | Inhibit presynaptic reuptake of serotonin | Nausea, diarrhea, sexual dysfunction, serotonin syndrome | As a class, common and reasonable first-line agents | ||
| Citalopram | 20 mg daily | 20-40 mg daily (maximum 20 mg daily in patients age >60 yr) | Risk of QTc prolongation/torsades de pointes in at-risk patients | Few drug-drug interactions. May be activating | |
| Escitalopram | 10 mg daily | 10-20 mg daily | Enantiomer of citalopram. May be activating | ||
| Fluoxetine | 20 mg daily | 20-40 mg daily (depression), up to 80 mg daily (OCD) | Long half-life; tends to be activating | ||
| Paroxetine | 20 mg daily | 20-50 mg daily | Anticholinergic effects | Tends to be sedating | |
| Sertraline | 25-50 mg daily | 50-200 mg daily | Few drug-drug interactions. May be activating | ||
| Serotonin and norepinephrine reuptake inhibitors (SNRIs) | Inhibit presynaptic reuptake of serotonin and norepinephrine | Nausea, diarrhea, serotonin syndrome, sinus tachycardia, mild elevation in blood pressure, tremor | |||
| Duloxetine | 30-60 mg daily | 30-60 mg daily on a twice-daily schedule, maximum of 120 mg/day | |||
| Venlafaxine | 37.5 mg bid | 150-375 mg/day on bid schedule | XR form allows once-daily dosing | ||
| Desvenlafaxine | 50 mg daily | 50 mg daily, maximum of 100 mg ER daily | Metabolite of venlafaxine | ||
| Tricyclic antidepressants (TCAs) | Inhibit presynaptic reuptake of serotonin and norepinephrine (in varying proportions depending on the specific TCA) | Anticholinergic effects, sedation, orthostatic hypotension, tremor, cardiac conduction delays, ventricular arrhythmias | |||
| Amitriptyline | 25-75 mg qhs | 150-300 mg qhs | Strongly anticholinergic and sedating; aim for combined amitriptyline/nortriptyline blood level of 120-250 ng/mL | ||
| Desipramine | 25-75 mg daily | 150-300 mg daily | Aim for blood level of 115-250 ng/mL | ||
| Doxepin | 25-75 mg qhs | 150-300 mg qhs | Strongly sedating | ||
| Imipramine | 25-75 mg daily | 150-300 mg daily | Strongly anticholinergic; aim for combined imipramine/desipramine blood level of 180-350 ng/mL | ||
| Nortriptyline | 25-50 mg qhs | 50-150 mg qhs | Aim for blood level of 50-150 ng/mL; least anticholinergic of the TCAs | ||
| Monoamine oxidase inhibitors (MAOIs) | Inhibit monoamine oxidase, the enzyme that catalyzes oxidative metabolism of monoamine neurotransmitters | Need for tyramine-free diet to avoid sympathomimetic (hypertensive) crisis; sedation, anticholinergic effects, tremor, orthostatic hypotension | Initiation of any MAOI for a psychiatric indication generally should be on advice and under supervision of a psychiatrist | ||
| Isocarboxazid | 10 mg bid | 20-60 mg/day in bid-qid dosing | |||
| Phenelzine | 15 mg tid | 45-90 mg/day in tid or qid dosing | |||
| Selegiline | (selective MAO-B inhibitor) | 5 mg bid | 5 mg bid | Tyramine-free diet not required | Take with meals |
| Tranylcypromine | 10 mg tid | 30-60 mg/day in tid dosing | |||
| Other | |||||
| Bupropion | Unknown, although it is a weak inhibitor of presynaptic reuptake of norepinephrine and dopamine | 75-150 mg/day | 300-450 mg/day | Activating; risk for seizures reduced by divided dosing and careful dosage titration | Divided dosing required unless using SR or XL forms. A reasonable alternative to SSRIs as a first-line agent |
| Mirtazapine | Antagonist at α 2 and 5-HT 2 receptors | 15 mg qhs | 30-45 mg qhs; maximum of 45 mg qhs | Sedation, hyperphagia | Becomes less sedating at higher doses. Often used for more severe or treatment-refractory depression |
| Trazodone | Inhibits presynaptic reuptake of serotonin; antagonist at 5-HT 2 and 5-HT 3 receptors | 25-50 mg qhs | 300-600 mg qhs for depression, 25-100 mg qhs for insomnia | Sedation, priapism | Few sexual side effects |
| Vilazodone | Inhibits presynaptic reuptake of serotonin; agonist at 5-HT 1A receptors | 10 mg daily | 40 mg daily | Nausea, diarrhea, sexual side effects | Dosage must be increased slowly. Reasonable second-line agent |
| Vortioxetine | Inhibits presynaptic reuptake of serotonin; agonist at 5-HT 1A receptors, antagonist at 5-HT 3 receptors | 10 mg daily | 20 mg daily | Nausea, diarrhea, sexual side effects | Reasonable second-line agent |
∗ Patients on any of these medications must be monitored for suicidal thoughts.
In most general medical settings, it is common and reasonable practice to begin medication therapy with a selective serotonin reuptake inhibitor (SSRI) because of tolerability and straightforward dosing. The choice of initial SSRI may be guided by relative side effect profiles, in particular whether to prefer or avoid sedation, although these effects may vary in individual patients. Serotonin-norepinephrine reuptake inhibitors (SNRIs) are reasonable choices for patients who do not achieve remission after an adequate trial of a SSRI and as first-line options for patients with more severe episodes. Initiation of treatment with tricyclic antidepressants or monoamine oxidase inhibitors is generally limited to patients with more severe, complex, or treatment-refractory disorders that generally require psychiatric consultation.
Antidepressant medications appear to increase the relative risk for suicidal behavior in adolescents and young adults, so such patients require careful benefit/risk assessments and close monitoring. By comparison, the relative risk for suicidal behavior is not increased by drug treatment in individuals older than age 25 years and is substantially reduced in older adults.
For severe major depression, including significant suicidality, melancholic symptoms, and substantial functional disability, psychiatric consultation is required and hospitalization may be indicated. Psychotherapies alone are insufficient for more severe forms of depression, including major depression with psychotic features, so medications should be used as initial treatment for most patients with more severe forms of major depression. Overall data suggest that no second-generation agent is predictably better than others, although agents targeting noradrenergic as well as serotonergic systems may be more efficacious in more severe depression. For patients with psychotic depression, the addition of an antipsychotic medication (see Table 362-12 ) to an antidepressant is more efficacious than either alone. For postpartum depression ( Chapter 221 ), zuranolone (a neuroactive steroid that modulates gamma butyric acid receptors at 50 mg daily for 14 days) may be the preferred option.
For medication-resistant major depression, expert consultation is required. Electroconvulsive therapy is the most effective treatment available and is the preferred approach for the most severe forms of major depression, especially major depression with psychotic features. , A single intravenous dose of ketamine may rapidly reduce severe depressive symptoms within 24 hours, and esketamine nasal spray is effective for treatment-resistant depression. Ketamine appears to be as effective as electroconvulsive therapy for treatment-resistant major depression without psychotic features. However, ketamine can lead to a significant increase in symptoms of psychosis in normal volunteers and people with schizophrenia. Optimal management strategies after initial improvement with ketamine or esketamine remain to be determined.
Deep brain stimulation is an investigational therapy for otherwise refractory depression. Overall evidence to date offers modest support for the efficacy of repetitive transcranial magnetic stimulation for depression, whereas transcranial direct current stimulation does not appear to be beneficial. Hallucinogenic drugs such as lysergic acid diethylamide (LSD), psilocybin, , and 3,4-methylenedioxymethamphetamine (MDMA) are experimental approaches that should be considered only under supervised conditions.
After a patient achieves remission with an initial treatment, the same treatment should be continued for at least 6 months to reduce the risk of relapse. Patients who have had three or more lifetime episodes, or who develop rapidly recurrent or severe functionally disabling episodes should receive maintenance therapy. Mindfulness-based cognitive therapy, behavioral activation, and maintenance antidepressant treatment can reduce the rate of relapsing or recurrent depressive symptoms, and may have approximately equal efficacy in broad outpatient populations. For highly recurrent depression, however, maintenance pharmacotherapy may have the best outcomes. Optimal care for depression in primary care and other treatment settings may be enhanced by the use of collaborative care models that include on-site mental health specialists, although the lack of reimbursement mechanisms often limits their implementation.
Optimal guideline-based treatment of major depression results in full remission in up to 80% of patients, and the expectation is that patients with major depression will return to baseline functioning after resolution of the depressive episodes. However, at least 50 to 70% of patients will suffer recurrent episodes, up to 20% may experience chronic major depression, and many more will achieve only partial remission with persistent lower-level symptoms because of a variety of factors, including limited access to care, reluctance to seek or adhere to treatment, or insufficiently assertive treatment strategies by the treating clinician. Worldwide, less than 25% of individuals with depression receive adequate treatment and are at higher risk of recurrent depressive episodes and of suicide. The life time risk of suicide among patients with untreated depression is nearly 20%.
Bipolar disorder, also known as bipolar I disorder, is characterized by recurrent episodes of idiopathic mania. Most persons with bipolar disorder also have recurrent episodes of major depression.
The 12-month prevalence of bipolar disorder is approximately 0.6%, with a slightly higher prevalence in males compared with females. The average age at first onset is late adolescence or early adulthood. Childhood onset is possible, but diagnosis may be difficult because of symptomatic overlap with other conditions of childhood, such as attention deficit hyperactivity disorder. First onset in midlife to late life is also possible, although late-onset mania is often secondary to other medical conditions or drugs rather than idiopathic bipolar disorder.
Even though the pathogenesis of bipolar disorder remains unclear, genetic factors play a greater role than in unipolar depressive conditions. Heritability has been traced to several specific loci in rare families, but genetic screening is not yet clinically useful, and the gene associations have to date revealed no unifying pathophysiologic themes. Most cases of bipolar disorder are polygenic and multifactorial, with genetic factors accounting for approximately 50% of the risk for the disorder. Dysregulation of frontostriatal systems is probably involved in the manifestations of the illness. Though not specific enough to be diagnostic, structural neuroimaging studies show increased ventricular-brain ratios suggestive of parenchymal atrophy. Phase advance of central circadian rhythms can precipitate episodes of mania in persons with bipolar disorder, so the decreased sleep need of persons with incipient mania may produce a vicious cycle in which phase-advanced circadian cycles lead to a further decreased need for sleep, thereby resulting in further phase advancement. Psychosocial stressors also often play a role in precipitating episodes of both mania and depression.
The symptoms of mania include a distinct period of abnormally and persistently elevated (euphoric) or irritable mood; goal-directed hyperactivity, often for pleasurable activities, with poor judgment that leads to long-lasting adverse financial, psychosocial, or medical consequences (e.g., sprees of spending, sexual activity, or gambling); increased energy; decreased need for sleep; pressured speech; and distractibility.
As with major depression, the diagnosis is based on findings from the history and examination revealing a pattern of recurrent manic episodes ( Table 362-6 ) that are usually interspersed with major depressive episodes and cannot be explained by other medical conditions, medications, or other substances. Persons with bipolar disorder may become psychotic while in manic or depressed states, but a history of psychotic symptoms in the absence of mania or depression indicates a diagnosis other than bipolar disorder. Manic and depressive episodes also may be seen in the course of delirium ( Chapter 361 ) and dementia ( Chapter 371 ), in which case the psychiatric symptoms are accompanied by the cognitive deficits that are the hallmark of these neurocognitive conditions.
| DIAGNOSTIC CRITERIA |
| A distinct period of abnormally, persistently elevated, expansive, or irritable mood; and abnormally and persistently increased goal-directed activity or energy lasting ≥1 week and present most of the day, nearly every day, AND 3 or more of the following symptoms/signs (4 or more if the mood abnormality is only irritability):
|
| MANIC SYMPTOMS/SIGNS GROUPED CONCEPTUALLY, WITH ADDITIONAL COMMON PHENOMENA |
| Emotional |
| Euphoria Irritability Labile affect |
| Ideational |
| Grandiosity |
| Somatic/Neurovegetative |
| Increased energy Psychomotor agitation Decreased need for sleep Distractibility |
| Other |
| Goal-directed hyperactivity Pressured speech Impaired judgment Flight of ideas Psychotic symptoms (may include delusions, hallucinations, or derailment of thought processes such as loose associations)—defines the subtype “mania with psychotic features” |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here