Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Psoriasis is a common chronic inflammatory disorder caused in large part by abnormal T-lymphocyte function.
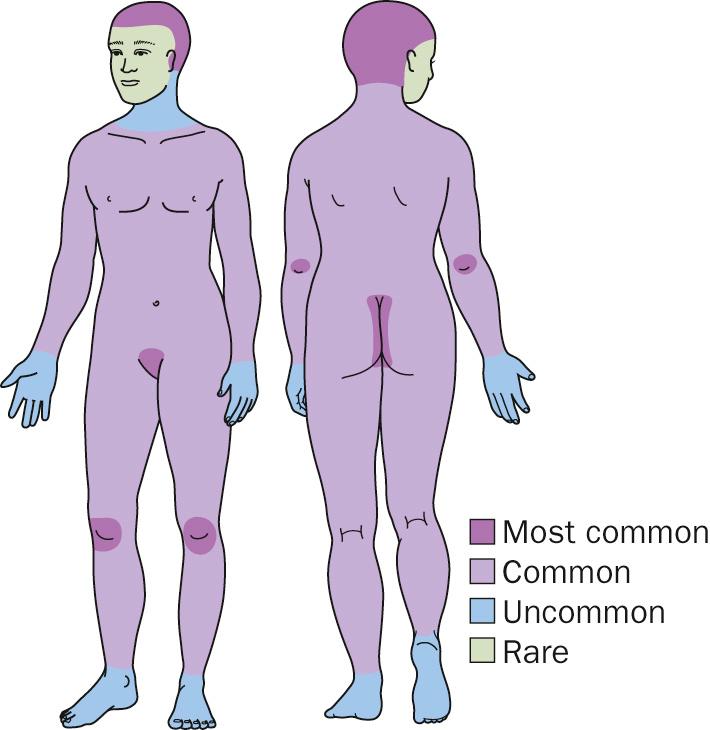
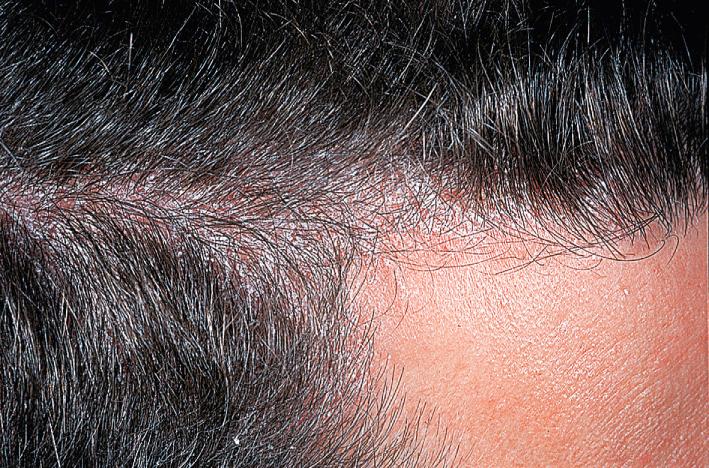
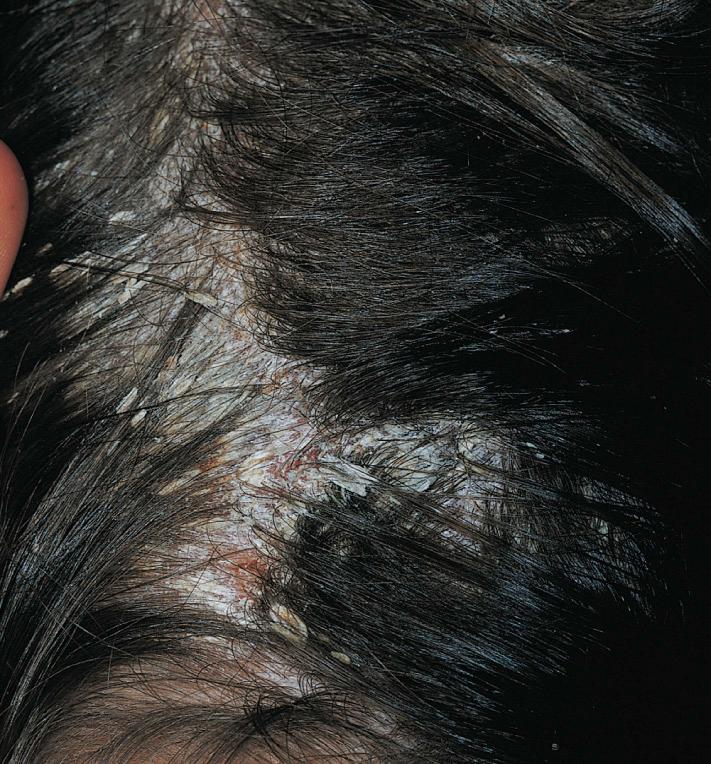
Pink to red papules and plaques with thick white scale may be localized or widespread, involving the scalp, elbows, and knees.
Psoriasis may be isolated to the scalp, nails, and skinfolds.
Although psoriasis persists throughout life, patients may experience extended periods of remission.
Prevalence worldwide is estimated to be 1% to 3% of the population.
Psoriasis affects all age groups; onset is more common from 20 to 30 years and 50 to 60 years of age.
Up to 90% of patients have a family history of psoriasis.
Histocompatibility studies have shown HLA-Cw6 to be associated with up to a 25% risk for developing psoriasis and a 90% risk for early onset psoriasis.
Many genetic loci have been linked to psoriasis, and PSORS1 is thought to account for a 50% risk for psoriasis.
Psoriasis is associated with an increased risk for anxiety, depression, obesity, diabetes, hypertension, lymphoma, myocardial infarction, and stroke.
Flares of psoriasis may be triggered by local factors (skin injury, scratching), systemic factors (infections, especially Streptococcus and HIV), psychologic stress, medications (lithium, beta-blockers, interferon, and antimalarials).
Psoriasis may be grouped into distinct clinical patterns that are not mutually exclusive; patients may present with one pattern that evolves into another.







Chronic plaque psoriasis is the most common presentation.
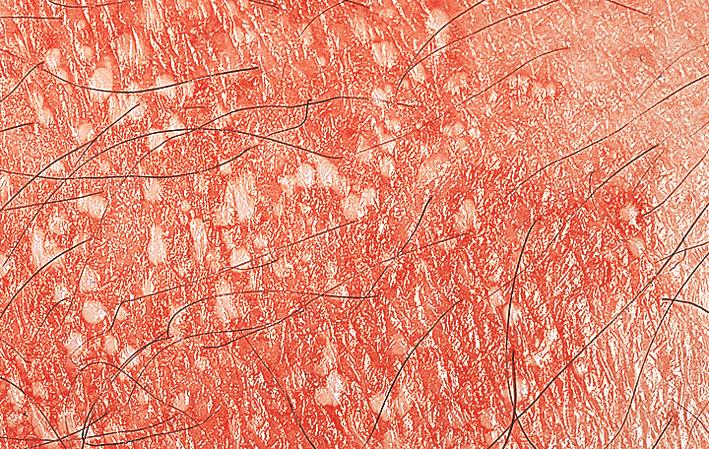
Red, sharply defined papules and plaques with thick white scale are seen and may be generalized with accentuation on the scalp, elbows, knees, and gluteal cleft.
Firmly adherent scale bleeds when it is removed (Auspitz's sign).
Aggressive mechanical removal of scale on the scalp may result in alopecia.
Guttate psoriasis is seen more commonly in children and young adults, who have been exposed to an upper respiratory virus or Streptococcus pyogenes.
Small round to oval red papules and plaques appear suddenly on the torso and extremities and have a tendency to resolve over a 6- to 12-month period.
Red, moist, and fissured plaques occur in the retroauricular folds, inframammary regions, axillae, inguinal creases, and intergluteal cleft.
Inverse psoriasis is often confused with primary dermatophyte, candidal and streptococcal infection. These organisms may initiate a psoriatic flare.





This severe form of psoriasis must be distinguished from other forms of cutaneous erythroderma, such as cutaneous T-cell lymphoma.
Onset may be acute (drug-induced, systemic steroid withdrawal) or chronic from poorly controlled psoriasis.
Patients may have skin tenderness, fever, weight loss, protein loss, and lymphadenopathy.
Pustular psoriasis is caused by intense inflammation resulting in sterile pustules.
Several clinical variants have been described, including generalized (seen in pregnancy, after infection, and systemic steroid withdrawal), localized (seen at the edge of an existing plaque), palmar/plantar (seen with smoking and possibly associated with bone lesions), and acral (seen on the distal portions of the toes and fingers with nail involvement).
Nail disease may occur in isolation, but most patients typically exhibit cutaneous signs of psoriasis. Signs of psoriatic nail disease include pits, nail whitening, friable nails, yellow spots (“oil spots”), splinter hemorrhages, thickened nail beds, and separation of the distal end of the nail plate from the nail bed (onycholysis).
Up to 30% of patients with psoriasis will develop psoriatic arthritis.
Arthritis is more common in patients with widespread cutaneous involvement.
A small number of patients develop psoriatic arthritis before the appearance of cutaneous psoriasis.
Five clinical patterns have been described: monoarthritis and asymmetric oligoarthritis (most common form), distal interphalangeal, symmetric polyarthritis (similar to rheumatoid arthritis), mutilating arthritis, and spinal arthritis.
Usually skin biopsy is not necessary to diagnosis psoriasis but should be considered before systemic therapy is administered.
Primary providers should monitor cholesterol, blood sugars, and blood pressure because psoriatic patients are at risk for cardiovascular disease and metabolic syndrome.
Throat cultures and antistreptolysin O titers should be performed in patients with guttate flares.
Wet mounts and bacterial cultures should be performed in patients with inverse psoriasis or in patients who flare despite adequate topical or systemic therapy.
In severe recalcitrant cases, evaluate for infection with HIV.






Seborrheic dermatitis
Dyshidrotic eczema (hand, foot)
Tinea capitis (scalp)
Onychomycosis (nails)
Intertrigo (candidal or streptococcal)
Pityriasis rosea
Drug eruption
Psoriasis is treated in a graded manner starting with topical therapy and progressing to phototherapy and finally to systemic therapy.
Given the chronic relapsing nature of psoriasis, treatments are combined and rotated to minimize the toxicity of any one given treatment.
Topical glucocorticoids are the mainstay of localized psoriasis.
In general, psoriatic lesions on the scalp, torso, and extremities require more potent glucocorticoids (classes I−II), whereas lesions on the delicate areas of the face and intertriginous areas receive lower potency glucocorticoids (classes V−VI).
Steroid-sparing medications (tar, retinoids, vitamin D analogs) are frequently combined with glucocorticoid to enhance their effectiveness and minimize side effects, such as skin thinning.
An example of a regimen for plaque psoriasis on the elbows may include a vitamin D analog twice daily (e.g., calcipotriene cream, calcitriol ointment) during the week and a class I glucocorticoid twice daily during the weekends.
Glucocorticoids may be compounded with tar in specialized compounding pharmacies.
Calcipitriol-betamethasone diproprionate (Taclonex) is an example of a combination medication that is effective for psoriasis on the scalp, torso, and extremities.
Triamcinolone acetonide injections (5–10 mg) effectively induce remission in many difficult-to-control psoriatic plaques.
Some locations, such as the scalp and nails, may be more challenging to treat.
Thick scale on the scalp may be gently removed with olive oil occluded with a warm, moist towel for 30 minutes. Scale must be gently removed to prevent alopecia.
Derma-Smoothe oil is effective for more mild scalp psoriasis.
Foams and solutions are easier to apply to the scalp than creams and ointments.
Mildly affected nails may be treated with a class I topical glucocorticoid solution.
More severely affected nails may be treated with triamcinolone acetonide injections (5–10 mg) into the nail bed.
Generally, nail disease requires systemic therapy for improvement.





Phototherapy may be used as a solo therapy or in combination with topical or systemic agents.
The most common treatment is narrowband ultraviolet B (311–313 nm), which has been shown to be highly effective.
Patients require three treatments per week for 1 to 3 months. Many patients go on and off phototherapy for years.
Tar, vitamin D analogs, retinoids (tazarotene cream or gel), and topical steroids enhance the effectiveness of phototherapy.
The excimer laser (ultraviolet B, 308 nm) is effective for limited plaque psoriasis and is administered two to three times per week.
Other modalities include broadband ultraviolet B and A wavelengths (usually administered with psoralen).




Current systemic therapy may be divided into traditional and biologic therapy.
Methotrexate, cyclosporine, and acitretin are the most widely used traditional systemic treatments for psoriasis.
Methotrexate acts by inhibiting folic acid and is effective for all forms of psoriasis.
Methotrexate is administered weekly through oral, subcutaneous, and intramuscular routes.
Cyclosporine is a calcineurin inhibitor and effectively improves psoriasis quickly.
Cyclosporine may be used to quickly improve more severe forms of psoriasis, such as pustular psoriasis and erythrodermic psoriasis.
Acitretin is a systemic retinoid that is very effective for all forms of psoriasis, but is used mostly for erythrodermic, pustular, and palmar/plantar psoriasis.
Biologic treatments are immune modulators that target the T cell and cytokines involved in psoriasis.
These agents are highly effective but are very expensive and thus are not accessible to many patients.
Etanercept, infliximab, and adalimumab target tumor necrosis factor-alpha; ustekinumab targets p40 subunit of interleuin-12/23; secukinumab and ixekizumab target interleukin-17A. Brodalumab binds to the IL-17 receptor. Guselkumab targets interleukin-23.
There are many targeted immunologic modulators in the pipeline for psoriasis.




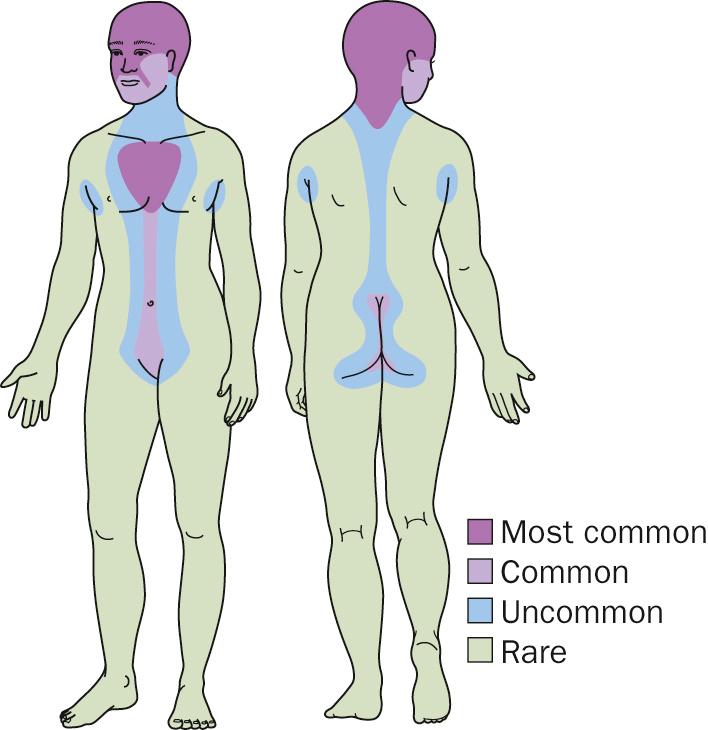
Seborrheic dermatitis is a common, chronic, inflammatory condition characterized by pink to yellow plaques with waxy scale involving areas of the body with increased sebaceous glands including the scalp, central face, ears, and chest.
Malassezia furfur (Pityrosporum ovale) is thought to cause seborrheic dermatitis.
Seborrheic dermatitis occurs in all age groups.
Infantile seborrheic dermatitis tends to resolve by 1 year of age.
Approximately 5% of adults have seborrheic dermatitis.
Men are affected more than women.
Seborrheic dermatitis is more severe in patients with neurologic disorders (Parkinson's disease, stroke, and head trauma) and patients infected with HIV.
Pink to yellow papules and plaques with greasy scale involve scalp, central face, ears, and presternal areas. Characteristic locations are the eyebrows, the base of eyelashes (seborrheic blepharitis), nasolabial folds and paranasal skin, and external ear canals.
May affect flexural skin, including the postauricular, inguinal, and inframammary folds as well as the anogenital area.
Skin biopsy should be performed for atypical presentations.
Fungal wet mount preparations should be considered for resistant cases.
Yellow, greasy adherent scale on the vertex of the scalp (cradle cap) with minimal underlying redness.
Scale may accumulate, becoming thick and adherent over much of the scalp.
Diaper area and axillary skin may become involved, often with redness that is more obvious than scaling.
Secondary bacterial and candidal infection can occur.
Infantile seborrheic dermatitis is easy to diagnose. Infants who do not respond to standard treatment measures can rarely have an underlying systemic illness such as Langerhans' cell histiocytosis or zinc deficiency.
Infantile seborrheic dermatitis is usually a self-limited condition often not requiring treatment. Usually gentle removal of scale and a low-strength corticosteroid are sufficient to control infantile seborrheic dermatitis.
Referral to a dermatologist is indicated for infants with severe recalcitrant seborrheic dermatitis or with widespread disease.













Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here