Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Additional content is available online at Elsevier eBooks for Practicing Clinicians
Additional content is available online at Elsevier eBooks for Practicing Clinicians
Each year, almost 800,000 Americans have a stroke, and between 200,000 and 500,000 have a transient ischemic attack (TIA). Data from 2020 show that about 610,000 of these strokes are new and 185,000 are recurrent. Overall the incidence of stroke has declined in adults from the 1980s to 2010, although this was somewhat uneven in various patient subgroups. Approximately 146,000 people in the United States die of a stroke each year, making stroke the fifth leading cause of death. (Globally, stroke is the second leading cause of death.) Stroke kills more women than men, mainly because there are more elderly women than men in the United States. About 1 out of every 19 deaths in the United States is due to a stroke, of which the majority (63%) occur outside of an acute care hospital. Although ischemic strokes are most common, the mortality associated with an acute ischemic stroke is much lower (about 15%) than with a hemorrhagic stroke (mortality of 40% to 45%). The overall number of deaths from stroke has declined 30-40% from the 1980s to 2010. This likely reflects improved stroke prevention as well as improvements in acute care. The decline is similar in men and women but is more pronounced in an older population (65 and above) compared with younger groups.
Overall, the incidence of stroke is lower in women than in men in most age groups. However, the impact of cardiovascular disease (CVD) risk factors (high blood pressure [BP], diabetes, heart disease) on stroke risk is higher in women than in men in most age groups. Although stroke incidence may be declining in some groups, aging of the population combined with more CVD risk factors may be contributing to an increased lifetime risk of having a stroke. Approximately 6.8 million Americans age 20 years or older have had a stroke, which is a leading cause of severe, long-term disability. Stroke disproportionately affects some minority populations (see Chapter 93 ). Black and Hispanic populations (compared with whites) have a higher incidence and mortality from stroke. This disparity likely results in part from more stroke risk factors, more severe risk factors, and undertreatment of these risk factors in certain groups and populations. Environmental factors as well as socioeconomic disparities also play a role in the differential impact of some risk factors on various populations, leading to higher mortality.
Strokes are generally classified as ischemic or hemorrhagic ( Fig. 45.1 ). This chapter will focus primarily on ischemic stroke and TIAs and will begin by discussing the various types of ischemic strokes and TIAs and the pathophysiology leading to a stroke ( Table 45.1 ). The next section will review approaches for primary and secondary stroke prevention. The third section will focus on acute therapy for patients with ischemic stroke and TIA. The important topic of rehabilitation will not be discussed in this chapter because of space limitations but is discussed in Chapter 33 .
| Stroke Mechanism | Vessel Type | Stroke Type/Syndrome | Acute Therapy | Secondary Prevention | Comment |
|---|---|---|---|---|---|
| Atherothrombotic | Variable small, medium, large | Highly variable; large hemispheric to tiny lacunar; brainstem also | IV lytics, EVT if large/medium vessel | CVD risk factors control; antiplatelet agents consider surgery or stent | Most common etiology; highly variable presentation |
| Cardioembolic | Variable; MCA or MCA branch is typical | Cortical or hemispheric syndrome | IV lytics, could be EVT if large/medium vessel | Consider anticoagulation if AF | Other etiologies besides AF; endocarditis, valve disease, PFO |
| Artery-to-artery embolization | Typically small or medium vessel | Cortical branch syndrome | IV lytics | Medical therapy; consider CEA or stent | Identify proximal atherostenotic lesion |
| Hypercoagulable state | Typically small or medium vessel | Cortical branch syndrome | IV alteplase | Anticoagulation | Rule out underlying cancer |
| Inflammatory vasculopathy | Small or medium vessel | Any vessel; could impact retina, spinal cord | Consider steroids | Immunosuppressive therapy | May be due to systemic autoimmune disease or isolate to CNS |
| Structural vasculopathy/dissection | Vertebral or internal carotid artery | Vessel occlusion or artery-to-artery emboli | Anticoagulation, stent, antiplatelets | ||
| Venous thrombosis | Sagittal or transverse sinus, jugular vein; not in a typical arterial territory | Hemorrhagic infarction; increased intracranial pressure | Anticoagulation | Address underlying process | Typically due to underlying hypercoagulable state; common in pregnancy |
Ischemic stroke is a heterogeneous condition with a common pathway of injury, namely reduced or obstructed arterial blood flow to one or more parts of the brain (which includes the retina and spinal cord). Even among ischemic strokes, there are a variety of underlying mechanisms that can lead to reduced blood flow (see Table 45.1 ). (There are a few rare processes that do not follow this common pathway, e.g., mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes [MELAS] and cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy [CADASIL] .)
Atherothrombosis is the most common underlying mechanism for an ischemic stroke. It can affect large vessels (aorta, carotid artery, vertebral and basilar arteries), medium-sized vessels (middle, anterior, posterior cerebral arteries), and small vessels deep in the brain (and the retina). It is important to understand that atherothrombosis is a systemic disorder affecting blood vessels in many different locations throughout the body (heart, kidneys, major vessels such as the aorta and femoral artery, etc.) (see Chapter 24 ). , It is typically mediated by a host of cardiovascular disease risk factors, as discussed later. Therefore, the prevention and treatment of atherothrombosis should be viewed from a systemic perspective.
Atherothrombosis of the carotid artery can cause a hemispheric stroke as well as areas of watershed ischemia involving parts of the hemisphere. If the process involves the basilar artery, it can produce a devastating brainstem stroke. Atherothrombotic lesions can also act as a source of artery-to-artery emboli whereby parts of a proximal lesion embolize downstream to produce a smaller stroke (see Chapter 25 ).
Embolization from a central source such as the heart (or aorta) is another very common stroke mechanism. Cardiac emboli can affect almost any part of the body, although the brain is the most sensitive to this type of insult. Such emboli typically lodge in medium to small-sized vessels. Common underlying etiologies include atrial fibrillation (AF), valvular disease, recent myocardial infarction (MI), mural thrombus, infective endocarditis, paradoxical emboli, and others (see Chapter 37, Chapter 41, Chapter 66, Chapter 74, Chapter 75, Chapter 79 ).
Lacunar strokes account for about 20% to 24% of all ischemic strokes. They involve a tiny artery (200 μm) deep in the brain and produce one of five common lacunar stroke syndrome ( Table 45.2 ). The underlying pathology is either a hypertrophic proliferation of the vessel wall (lipohyalinosis) or microatheroma in the penetrating vessels. It is noteworthy that rupture of the same vessels in the same location can also produce a hypertensive cerebral hemorrhage.
| Lacunar Syndrome | Anatomy | Typical Symptoms |
|---|---|---|
| Pure motor hemiparesis | Internal capsule | Hemiparesis affecting face/arm/leg about equally |
| Hemisensory loss | Thalamus | Loss of sensation affecting face, arm, trunk, and leg |
| Ataxic-hemiparesis | Basis pontis or posterior limp of internal capsule | Ataxia > weakness involving leg > arm; no dysarthria |
| Mixed motor-sensory syndrome | Internal capsule or centrum semiovale | Mixed motor and sensory symptoms |
| Dysarthria-clumsy hand | Internal capsule, basis-pontis | Dysarthria, ataxia/dysdiadochokinesia |
In the hyperacute setting it may not be possible to precisely determine the underlying etiology of a stroke or TIA because of time constraints. However, for effective secondary prevention, understanding the underlying mechanism and etiology is often very important.
In any type of stroke, the symptoms will be dependent on the vessel involved and the territory of infarcted tissue ( Table 45.3 ). The rapidity of onset may also be a clue to the stroke mechanism. Atherothrombotic and lacunar strokes typically display a gradual or stepwise onset of symptoms, with evolution spanning minutes to an hour or more. An embolic mechanism typically will have maximum symptoms at once, which may lessen a bit over ensuing minutes to hours in some cases.
| Involved Vessel | Brain Region | Common Mechanism | Typical Symptoms | Comment |
|---|---|---|---|---|
| Carotid artery | Hemisphere | Atherothrombotic or dissection | Complete hemiplegia + aphasia or neglect syndrome | May develop ipsilateral Horner syndrome |
| Middle cerebral artery | Portions of hemisphere | Embolic | Partial hemiparesis (face, arm > leg); aphasia if dominant hemisphere; neglect syndrome and apraxia if nondominant | Symptoms dependent on artery involved |
| Anterior cerebral artery | Frontal lobe | Atherothrombotic or embolic | Weakness leg > arm > face; apraxia | May display abulic behavior |
| Basilar artery | Brainstem | Atherothrombotic | Possible loss of consciousness, bilateral weakness; abnormal ocular movements; ataxia | May develop crossed sensory deficits, Horner syndrome |
| Posterior cerebral artery | Occipital lobe | Embolic | Visual field cut; unable to read | May develop visual neglect if tracts involved; unable to read |
| Lacunar syndrome | Deep in hemisphere or brainstem | Lipohyalinosis or small vessel atheroma |
|
|
Cryptogenic strokes account for 15% to 20% of all ischemic strokes ( Table 45.4 ). Recent studies of these patients have identified some common mechanisms that may help to better define the underlying etiology in some of these patients (see Tables 45.3 and 45.4 ). Paroxysmal AF has been identified in at least 12% of such patients after 1 year of cardiac monitoring (see Chapter 66 ). A patent foramen ovale (PFO) is also found in 5% to 10% of such patients, particularly those <50 years of age (see Chapter 82 ). Less common mechanisms for ischemic stroke include vasculopathies (inflammatory, structural) and a hypercoagulable state. Atherosclerotic plaques without a high-grade stenosis may be an underappreciated etiology for cryptogenic strokes. Patients may have entities such as antiphospholipid antibodies/anticardiolipin antibodies or a lupus anticoagulant (see Chapter 95 ). Some patients may have a hypercoagulable state due to an underlying malignancy, which is often occult. Rare genetic disorders (e.g., CADASIL, cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy [CARASIL] CARASIL ) are other uncommon etiologies. The diagnosis and treatment of such patients may be problematic. , ,
| Presumed Etiology/Mechanism | Diagnostic Test | Comment |
|---|---|---|
| Inflammatory vasculitis | Cerebral angiogram | May not be associated with a systemic inflammatory condition; often associated with prominent or new headaches |
| New or occult hypercoagulable condition | Full coagulation panel + genetic tests | Look for systemic clotting features (deep vein thrombosis, pulmonary embolism); may be seen with an occult malignancy |
| Cardioembolic | Implantable cardiac monitor to evaluate for paroxysmal atrial fibrillation; consider cardiac CT or MRI | Consider blood cultures to rule out endocarditis; cardiac imaging rule out fibroelastoma |
| Pulmonary arteriovenous malformation | Chest CT scan | May be associated with hereditary hemorrhagic telangiectasia |
| Genetic disorder | Family history; specific gene testing | Gene testing is commercially available; look for systemic signs of disease |
| Occult drug abuse | Complete toxicology screen | Patients often not forthcoming about drug abuse |
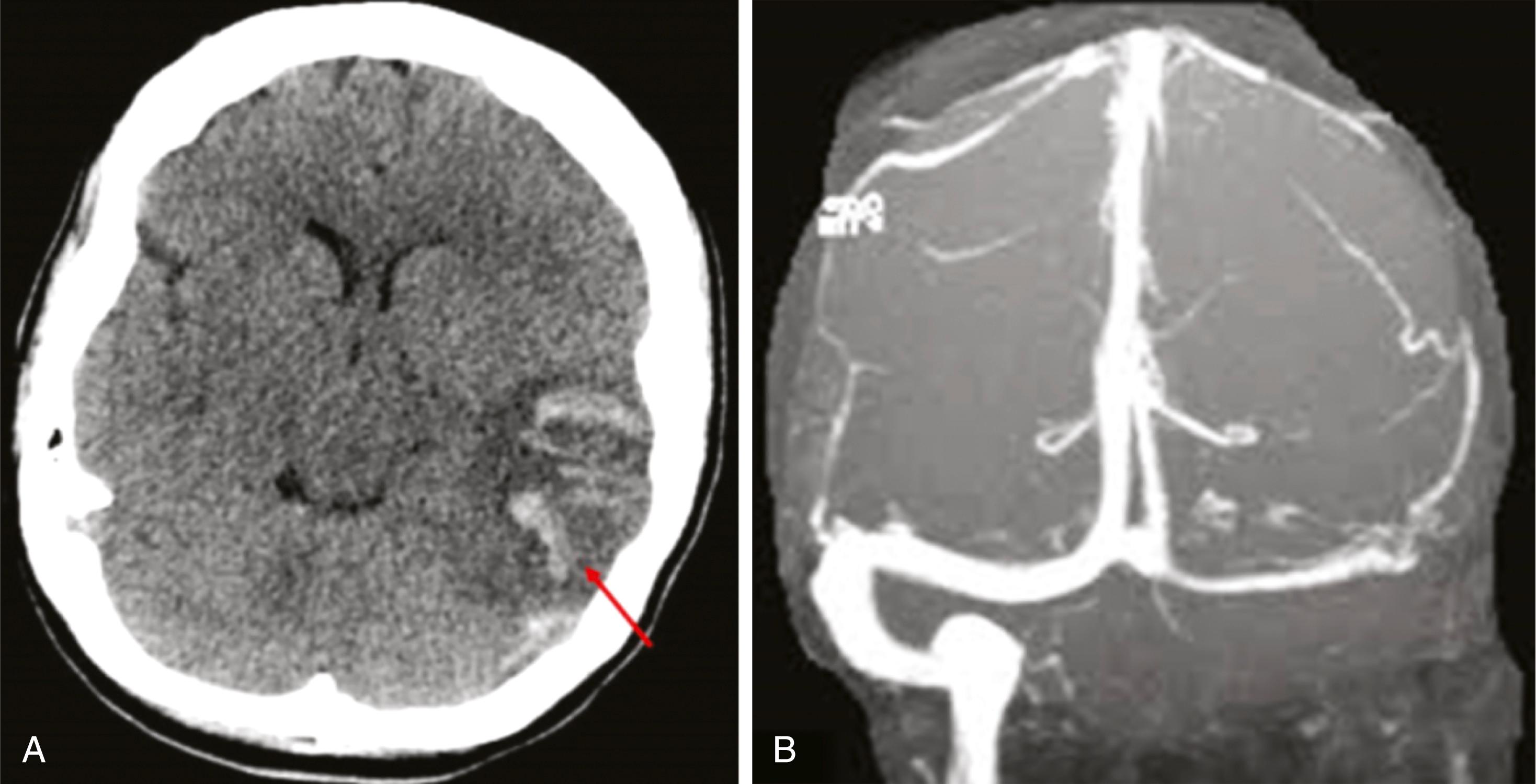
There is another uncommon stroke type or mechanism, a cerebral venous/sinus thrombosis (CVST). The sinus does not refer to nasal structures; rather the term “sinus” refers to large venous pathways typically at the base or surface of the brain. When one of the veins (i.e., superior sagittal sinus, transverse sinus, internal jugular vein) becomes occluded, it often leads to obstruction of venous outflow ( Fig. 45.2A ). Arterial inflow will then back up, leading to congestion of cerebral arteries and veins, increased intracranial pressure, headaches, and venous infarction. Such infarcts typically display substantial edema and mass effects and often undergo hemorrhagic transformation ( Fig. 45.2B ). They often do not follow usual arterial territories. Risk factors include pregnancy or postpartum state, sickle cell disease, dehydration, cancer, and hypercoagulable states. CVST has also been associated on rare occasions with adenovirus vector COVID-19 vaccines (see Chapter 94 ). CVST can be difficult to diagnose and visualize, especially if it involves the deep venous system. Magnetic resonance imaging (MRI) and magnetic resonance venography are key for making the diagnosis. Systemic anticoagulation is the initial treatment of choice. ,
This chapter will next focus on the risk factors and prevention strategies for ischemic stroke and TIA, followed by the acute care of these patients. Readers are directed to American Heart Association guidelines reviewing the use of carotid endarterectomy and angioplasty/stenting for primary and secondary prevention of stroke and for the chapters noted earlier for the treatment of common cardiac diseases such as AF, acute MI, and related conditions that can cause a stroke.
This section will begin by focusing on identifying stroke risk factors, assessing their impact, and reviewing treatment options. Chapter 25, Chapter 26, Chapter 27, Chapter 31 also address common CVD risk factors and their treatment.
Approximately 78% of strokes are first events, which makes primary prevention of paramount importance. Approximately 18% of survivors will have a second stroke within 4 years. Various studies have suggested that up to 80% to 90% of all strokes could theoretically be prevented with proper identification and optimal use of medications and behavior modification. Of course, identification of risk factors in asymptomatic patients represents a significant challenge in part because of a lack of access to healthcare, screenings for risk factors, the need for high levels of compliance, and the resources for adequate long-term treatment. This strategy also implies treatment of many asymptomatic patients for years to accrue the benefit of stroke prevention. Such an approach is challenging because of the long-term commitment needed, the high expense, and the lack of an immediate benefit.
Some common and clinically important risk factors are listed in Table 45.5 . These mirror some risk factors for CVD and coronary artery disease (CAD). These risk factors can be divided into modifiable (i.e., hypertension, diabetes, smoking, diet) and nonmodifiable (i.e., age, race, inherited/genetic conditions and traits ( Table 45.6 ). Other environmental risk factors (secondhand smoke, place of residence [such as the Stroke Belt]) are also modifiable, but not in the traditional way via medications or daily behaviors. In the past few years, additional and novel risk factors for stroke have been identified (see Table 45.5 ); these include sleep apnea, acute COVID-19 infection, and acquired hypercoagulable states. (see Chapters 89, 94, and 95 ).
| Risk Factor | Stroke Type/Vessel | Treatment Options | Comment |
|---|---|---|---|
| Elevated blood pressure | All types and vessels | Antihypertensive medications; diet, weight loss | Most modifiable risk factor |
| Diabetes | Small vessel > large vessel | Blood glucose control with medications; weight loss; diet; exercise | Requires long-term treatment; unclear benefits for primary prevention |
| Atrial fibrillation | Cardioembolic; medium and small vessels | Anticoagulation | Often asymptomatic |
| Hyperlipidemia | Large > small vessels | Diet, statins | Impacts large vessel strokes |
| Smoking/tobacco use | All types and vessels | Behavioral modification; medications | Applies to any use of tobacco; especially powerful for subarachnoid hemorrhage |
| Physical inactivity | All types and vessels | Behavior modification | Very common |
| Nutrition | All types and vessels | Change diet | Mediterranean diet helpful |
| Kidney disease | Small/medium > large vessel | Treat CVD risk factors | Related to glomerular filtration rate |
| Pregnancy | Medium/small vessel; venous infarction | Treat elevated blood pressure; possible coagulation disorder | Highest risk in third trimester and postpartum |
| Hormone therapy/OCPs | Small and medium vessels; venous thrombosis | Avoid if possible | Risk of ischemic stroke and venous thrombosis |
| Migraine headaches | Small and medium vessels | Avoid hormone therapy, smoking, vasoconstrictive agents | Highest risk if >30, complicated migraine, hormone replacement therapy use |
| Obstructive sleep apnea | All types | Sleep posture control, weight loss, CPAP | Underrecognized and undertreated |
| Psychosocial issues | All types | Treat underlying depression, stress | Address environmental factors |
| Inherited disorders | Variable | Variable | See Tables 45.6 and 45.10 |
| COVID-19 infection | All types and venous infarction | Possible anticoagulants | Evolving science |
| Geographic factors (Stroke Belt) | Small and medium vessel | Address CVD risk factors; consider moving | Complex environmental interactions |
| Air pollution | All types | Filters | Complex public health issue |
| Drug abuse | Large/medium vessels | Cessation of drug abuse | Cocaine can cause vasospasm and a vasculitis |
| Acquired Diseases (Modifiable) | Non-Modifiable | Inherited Disorders | Other |
|---|---|---|---|
| Hypertension | Age | Vasculopathy | Place of residence |
| Diabetes | Gender | Fabry’s disease | Medications (ethical and drug abuse) |
| Hyperlipidemia | Race | Hematologic | COVID-19 infection |
| Cardiac disease | Ethnicity | Clotting disorders | Sleep apnea |
| Smoking/second-hand smoke | Genetic | Cardiac disorders | |
| Obesity/lack of exercise | Many acquired disorders may often have a genetic component (i.e., some forms of hypertension, diabetes, lipid disorders) |
Overall, the modifiable risk factors for stroke largely mirror those for CAD and peripheral artery disease (PAD), although the impacts of these risk factors are not always equivalent. The American Heart Association/American Stroke Association (AHA/ASA) and other groups provide detailed, current evidence-based guidelines for prevention of a first stroke. ,
In general, the identification and treatment of these risk factors do not differ very much from a primary versus secondary prevention perspective. Although some studies have failed to show convincing evidence that treating certain risk factors impacts the primary prevention of stroke, there is considerable cross-risk among stroke, CAD, and PAD. Therefore, treating the systemic risk factors almost always has a positive impact on disease prevention. Hence, primary and secondary prevention will be discussed together.
Modifiable risk factors are a focus for primary and secondary stroke prevention. High-priority areas include improving physical activity, treatment of dyslipidemia with statins and other agents (as well as diet), diet and nutrition, glycemic control, hypertension, treatment for obesity, and smoking cessation. The international INTERSTROKE study is an important resource to understand risk factors for all types of stroke. More than 13,000 patients with an acute stroke and 13,000 controls were used to identify major risk factors for stroke. Ten risk factors were estimated to account for about 90% of the modifiable risks for stroke ( Table 45.7 ). Because of how INTERSTROKE was designed, these 10 risk factors differ from other common risk factors; however, both are relevant in certain clinical circumstances (i.e., pregnancy, migraine headaches). Although these risk factors varied by region, they do provide a reasonable starting point to identify opportunities and targets for treatment.
| Risk Factor | Odds Ratio | PAR (99% CI) | Comment |
|---|---|---|---|
| Hypertension | 2.64 | 48 (45-51) | Most important treatable risk factor |
| Current smoking | 2.09 | 12 (10-15) | |
| Waist to hip ratio | 1.65 | 19 (13-25) | Obesity is a growing concern |
| Diet risk score | 1.35 | 23 (18-29) | Underappreciated |
| Physical activity | 0.65 | 36 (28-45) | Underappreciated |
| Diabetes mellitus | 1.36 | 4 (2-8) | Less impact on stroke |
| Alcohol intake | 1.51 | 6 (3-10) | More important in men than women |
| Psychosocial stress/depression | 1.30-1.35 | 17 (13-23) | Various definitions |
| Cardiac disease | 2.38 | 9 (8-10) | |
| Ratio of apolipoprotein B to A1 | 1.89 | 27 (22-42) | May be a biomarker of obesity |
When discussing the various risk factors, we must be aware that the risk factors are not just present or absent, as the severity and duration of the exposure have a significant impact. One approach to optimize primary (as well as secondary) prevention is to use the population attributable risk (PAR) to identify which risk factors will result in the largest number of prevented strokes.
As shown in Table 45.7 , the most prominent modifiable stroke risk factor with the highest PAR (48) is hypertension. This is consistent with many other epidemiologic studies of stroke. Other factors with high PARs include lack of physical activity (PAR 35.8), apolipoprotein ratios (26.8), diet (23.2), psychosocial factors (17.4), and smoking (12.4). Other well-recognized risk factors seem to have a lower impact on PAR; these include cardiac etiologies (PAR 9.1), heavy alcohol use (5.8), and diabetes (3.9). Fortunately, many of these factors can be modified with proper medical interventions such as the use of antihypertensives, weight loss, and exercise. Reducing BP has more of an impact in hemorrhagic stroke than ischemic stroke, but it clearly reduces the risks of all types of stroke.
Because hypertension is such a pervasive and important risk factor for all types of stroke, this chapter will provide additional details about its diagnosis and treatment ( see Chapter 2, Chapter 26 ). Overall, the prevalence of hypertension is 45.7 among non-Hispanic whites, 59.0 among non-Hispanic Blacks, 46.1 for Mexican Americans, and 45.2 for people of other races and ethnicities in the United States (see Chapter 93 ). This somewhat mirrors the stroke risk for different populations. In NHANES, the overall study population had BPs of 122.4/70.7 mm Hg. Among the patients with hypertension, the average BPs were 133.0/74.4 mm Hg for non-Hispanic whites, 136.8/76.1 mm Hg for non-Hispanic Blacks, and 134.8/76.1 mm Hg for Mexican Americans. This overall pattern closely matches the risks of stroke among the various groups. The risk of all CV events is further increased by the presence of additional CVD risk factors. The INTERSTROKE study found that untreated hypertension was associated with a higher risk of ischemic stroke (odds ratio [OR] 4.76, confidence interval [CI] 3.99 to 5.68), and a younger age at onset for all strokes (61.4 versus 65.4 years).
The 2020 International Society of Hypertension (ISH) guidelines recommend that for BPs in the <130/85 mm Hg range, monitoring every 3 years is reasonable. For patients with BPs in the 135/85 to 150/99 mm Hg range, confirmation with repeated measurements is recommended. If the BP is >160/100 mm Hg, confirmation within a few days is now recommended. Because >50% of patients with hypertension have other CVD risk factors, an assessment for these other factors (diabetes, hyperlipidemia, etc.) is recommended.
The ISH guidelines are somewhat different from the 2017 AHA/ACC hypertension guidelines. The 2017 guidelines, based largely on the results of the SPRINT (Systolic Blood Pressure Intervention Trial) study, redefined a normal BP as less than 120/80 mm Hg. , A BP of 120 to 129 mm Hg systolic and diastolic >80 mm Hg is now defined as “elevated BP.” Stage 1 hypertension is now defined as a systolic BP of 130 to 139 mm Hg or diastolic BP of 80 to 89 mm Hg ( Table 45.8 ). This has implications for hypertension awareness, treatment, and potential risk reduction in large populations.
| Blood Pressure Reading (mm Hg) | Classification |
|---|---|
| <130 SBP and <85 DPB | Normal BP |
| 130-139 SBP and/or 85-89 DBP | High-normal BP |
| 140-159 SBP and/or 90-99 | Grade 1 hypertension |
| ≥160 SBP and/or >100 DBP | Grade 2 hypertension |
Although a specific antihypertensive regimen must be individualized, the actual reduction in BP is generally more important than the specific agent or agents used. SPRINT compared the benefit of treatment of systolic BP to a target of lower than 120 mm Hg with treatment to a target of lower than 140 mm Hg in patients at increased risk of CVD events who had systolic BP of 130 to 180 mm Hg. Stroke occurrence fell from 1.5% to 1.3% annually, but the difference was not significant (HR, 0.89; 95% CI 0.63 to 1.25; P = 0.50).
Although the landmark SPRINT trial did show the benefits of aggressive BP reduction to <120/80 mm Hg in patients at high risk for CVD events, there did not appear to be an overt benefit in terms of stroke reduction. This may have been due in part to the exclusion of patients with a prior stroke from the SPRINT trial. Other factors might have been the relatively small number of stroke events in the study, choice of medications, and duration of follow-up. Otherwise, CVD death, overall mortality, and heart failure were all significantly reduced with BP reductions.
The HOPE-3 trial also evaluated an antihypertensive in people at intermediate risk but without CVD; no overall benefit for stroke reduction was found. Explanations for this neutral result might include the choice of antihypertensives (candesartan and hydrochlorothiazide) and the small reduction in BP with treatment (mean, 6/3 mm Hg).
A large meta-analysis (>300,000 patients) of BP reduction for the primary prevention of stroke and other major CVD outcomes, along with other large analyses, did show a benefit for stroke prevention. There was a clear association between the magnitude of the benefit and the baseline BP. Patients with the highest BP (defined as >160 mm Hg systolic) showed the most significant benefit of BP reduction on primary stroke prevention. People with lower baseline BPs showed only marginal benefits for stroke prevention. However, benefit was found for the prevention of other CVD events. Nonetheless, because stroke patients have a high risk of other CVD events and related outcomes, treatment of hypertension is supported by neurologists (and especially vascular neurologists).
Treatment of patients with hypertension to prevent CVD and strokes is centered on lifestyle modification ( Table 45.9 ), avoidance of drugs that might exacerbate high BP (some nonsteroidal anti-inflammatory drugs, oral contraceptives, etc.) and specific pharmacologic interventions. Several classes of antihypertensive medications have shown efficacy for stroke prevention; these include thiazide type diuretics, angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers, and calcium channel blockers.
| Risk Reduction Strategy | Comment |
|---|---|
| Reduce salt intake | Modify diet, additives |
| Eat healthy diet | High in grains, fruits, vegetables |
| Healthy drinks | Moderate use of coffee and tea; beet juice, cocoa OK |
| Moderate alcohol consumption | 2 drinks per day for men; 1 drink per day for women |
| Weight reduction | Ethnic specific guidance |
| Smoking cessation | Specific programs, medications |
| Reduce stress | Meditation daily if possible |
| Reduce exposure to air pollution | Air filters, rural environment |
A systematic review of seven studies and eight control groups using a variety of BP reduction agents found overall a 23% to 25% reduction in recurrent stroke, fatal stroke, and MI, but no reduction in vascular or all-cause mortality (see Rashid, Classic References). The overall sample size was 15,527 patients.
Whether ACE inhibitors have a specific benefit in reducing recurrent stroke risk also remains uncertain. The HOPE study compared the effects of an ACE inhibitor and placebo in high-risk persons and reported a 24% reduction in the risk for stroke, MI, or vascular death in 1013 patients with a history of stroke or TIA (see Yusuf, Classic References). The PROGRESS (Perindopril Protection Against Recurrent Stroke Study) study tested the effects of a BP-lowering regimen, including an ACE inhibitor, in 6105 patients with stroke or TIA within the previous 5 years (see PROGRESS, Classic References). Randomization was stratified by intention to use single (ACE inhibitor) or combination therapy (ACE inhibitor plus the diuretic indapamide) in hypertensive (>160 mm Hg systolic or >90 mm Hg diastolic) and in normotensive patients. The combination, which reduced BP by an average of 12/5 mm Hg, led to a 43% reduction in recurrent stroke and a 40% reduction in major CVD events. This effect was present in both hypertensive and normotensive groups. Monotherapy with either agent showed no significant benefit. Specific patient characteristics and comorbid conditions should guide the choice of a specific antihypertensive regimen.
A more recent analysis of 93 trials examined BP reduction with various agents. The combined studies had >504,000 enrolled subjects who were followed for an average of 3.3 years. Using pairwise comparisons, relative benefits were seen for calcium channel blockers over ACE inhibitor, and combination therapy, particularly ACE inhibitor plus a calcium channel blocker, showed significant efficacy.
In clinical practice we often encounter patients with resistant hypertension despite treatment with three or more medications. In addition to optimizing adherence to current medications and maximizing lifestyle changes, such patients may warrant additional medical interventions. These might include adding medications such as a mineralocorticoid receptor antagonist, a beta- or alpha-adrenergic receptor antagonist, and minoxidil. Consultation with a hypertension specialist is warranted if multiple medications are needed for BP control (see Chapter 26 ).
Elevated low-density lipoprotein (LDL) cholesterol is an important risk factor for ischemic stroke in a primary or secondary prevention setting. This is especially true in patients with diabetes and other CVD risk factors. Lifestyle modification is a key component to reduce the risk of strokes. The use of statin agents has the potential to significantly reduce stroke risk in a primary-prevention population (see Chapter 27 ). Treatment of patients with coronary heart disease (CHD) or those at elevated risk for CHD with hydroxymethylglutaryl–coenzyme A reductase inhibitors (statins) reduces not only cardiac events but also the risk for a first stroke. A meta-analysis of statin therapy has shown that for each 39 mg/dL decrease in LDL cholesterol there is a 21% decline in the relative risk of a first ischemic stroke. , Statin therapy did not appear to be associated with a significant increase in the occurrence of intracerebral hemorrhage (ICH).
JUPITER (Justification for the Use of Statin in Prevention: An Intervention Trial Evaluating Rosuvastatin) evaluated the effect of a statin in persons with higher than median (>2 mg/dL) level of high-sensitivity C-reactive protein who were not otherwise candidates for statin treatment. In this group, treatment with rosuvastatin 20 mg daily reduced stroke by approximately 50%. The benefit of stroke reduction with statin therapy may extend to those at lower (5% to 10% 5-year) risk for vascular events. The HOPE-3 trial assessed the effect of rosuvastatin (10 mg daily) in CVD-free patients at intermediate risk (approximately 1% per year). Over 5.6 years, randomization to treatment led to a reduction in death from CVD causes, nonfatal MI, or nonfatal stroke from 4.8% to 3.7% (HR, 0.76; 95% CI 0.64 to 0.9; P = 0.002).
The HPS (Heart Protection Study) included 3280 patients with a history of stroke (including 1820 with stroke and no history of CHD) who were treated with either a statin or placebo (see Collins, Classic References). In those with a previous history of stroke, statin treatment reduced the frequency of major vascular events (MI, stroke, revascularization procedure, or vascular death) by 20%, but did not lower the risk for recurrent stroke (occurring in 10.5% of placebo versus 10.4% of statin group). The most reasonable explanation might be that patients were randomized an average of approximately 4 years after the index event. Most recurrent strokes occur soon (within the first few years), so those randomized in the HPS had a relatively low risk for recurrent stroke. More recent studies have shown clear benefits for stroke reduction (see later).
The SPARCL (Stroke Prevention with Aggressive Reduction in Cholesterol Levels) trial randomly assigned more than 4700 patients within 6 months of a noncardioembolic stroke or TIA and no known CHD to high-dose statin (atorvastatin 80 mg daily) or placebo for a primary endpoint of the first occurrence of a nonfatal or fatal stroke (see Amarenco, Classic References). Those randomized to high-dose statin treatment had a 16% relative reduction in nonfatal or fatal stroke as well as a 35% relative reduction in major coronary events. Added to the previous data on prevention of a first stroke, SPARCL showed that treatment with a high-dose statin can reduce the risk for recurrent stroke after stroke or TIA. On the basis of this trial, patients with atherosclerotic ischemic stroke or TIA and without known CHD should receive high-intensity statin therapy to reduce the risk for stroke and other CV events.
In the FOURIER (Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk) trial, adding the PCSK9 inhibitor evolocumab to standard therapy in patients with evidence of atherosclerotic disease significantly reduced the risk of a first or recurrent ischemic stroke (but there was no effect on hemorrhagic stroke). The risk of ischemic stroke was reduced by 25%, and the risk of stroke or TIA was reduced by 23%. Interestingly, the use of other lipid-lowering agents such as fibrates, niacin, and ezetimibe, as well as dietary modifications, did not impact stroke rates (although such interventions did reduce rates of other CV events in some populations).
The mechanism(s) by which statin therapy might reduce stroke rates include reducing intima-media thickness growth, slowing plaque progression, and reducing arterial inflammation. Despite some concerns about myalgias and the rare occurrence of significant myopathy, overall statin therapy is well tolerated and widely accepted as a mainstay of primary and secondary stroke prevention.
Diabetes is a common and major risk factor for all types of cardiovascular disease, including stroke (see Chapter 31 ). Currently >30 million adults in the United States have diabetes, and more than 84 million have prediabetes, which is a major precursor to diabetes. It is associated with a 2 to 6 times increased risk of stroke compared with nondiabetic patients. A recent meta-analysis of more than 100 studies of diabetes has shown that diabetic patients have a 2.3 times increased risk of ischemic stroke and 1.6 times increased risk of hemorrhagic stroke. Almost a quarter (24%) of people with diabetes are unaware they even have the disease.
Aggressive medical therapies as well as lifestyle changes are recommended to mitigate elevated blood glucose, prevent diabetic complications, and reduce the risk of cardiovascular events including death and stroke. However, numerous studies of patients with diabetes for the primary prevention of strokes have not shown an overwhelming positive effect. For example, the Euro Heart Survey on Diabetes and the Heart, the UK Prospective Diabetes Study, the ACCORD Study, the Veterans Affairs Diabetes Study, and the DCCT/EDIC study, among others, did not show evidence of a reduction in stroke as an isolated endpoint (although other CVD endpoints were reduced). An analysis of 9 large studies with more than 59,000 patients treated with intensive glycemic control did not find evidence for a reduction in stroke. Based on these data, aggressive treatment of diabetes and/or intensive glycemic control does not appear to have a significant impact on stroke reduction—although it is beneficial for the reduction of other CV events.
There is evidence that tight control of diabetes decreases stroke risk in a secondary prevention setting. As previously reviewed, management of BP and use of statins reduce stroke risk in patients with diabetes. The Insulin Resistance Intervention after Stroke (IRIS) trial tested the hypothesis that pioglitazone reduces the rates of stroke and MI after ischemic stroke or TIA in patients without diabetes who have insulin resistance. Over 4.8 years, stroke or MI occurred in 9.0% of the pioglitazone group and 11.8% of the placebo group (RR of 24%). The primary complications of treatment were a greater frequency of more than 4.5 kg weight gain, peripheral edema (35.6% versus 24.9%), and bone fracture requiring surgery or hospitalization (5.1% versus 3.2%).
What might explain this dichotomy between an effect on many CVD events and outcomes, but not stroke, for primary prevention? One factor may be the heterogeneity of stroke etiologies. Ischemic strokes can be due to atherothrombosis of small and large cerebral and cervical arteries, emboli from a cardiac source or the aorta, carotid dissection, hypercoagulable states, etc. Perhaps only some of these processes are directly related to diabetes and respond to glycemic control. See Chapter 31 for a discussion of newer diabetic medications that can reduce cardiovascular events and may do so by mechanisms that do not depend on glucose-lowering per se.
Cigarette smoking appears to increase the risk of stroke in a dose-dependent manner based on the number of pack-years of exposure (see Chapter 28 ). It is now well established that smoking cigarettes increases the risk of subarachnoid hemorrhage and possibly ICH although the data are somewhat conflicting. Secondhand smoke is a recently identified risk factor for stroke also. The good news is that within 2 to 4 years of smoking cessation, the risk of stroke related to smoking appears to return to a baseline level. Smoking cessation can be achieved via various behavioral modification programs and counseling, with or without specific pharmacologic interventions. Specific medications that are effective for smoking cessation include nicotine replacement therapies, bupropion, and varenicline. Furthermore, community and state restrictions on smoking appear to reduce smoking rates and related complications.
Diet and nutrition play an important role in stroke risk (see Chapter 29, Chapter 34 ). This may be mediated in part via impacts of diet on important stroke risk factors such as hypertension, lipid levels, and diabetes. Although data proving specific cause and effect relationships directly between diet and stroke may be lacking, there are some general recommendations that appear reasonable to address this important lifestyle modification (see Table 45.9 ). Some recommendations such as reducing sodium intake, increasing potassium intake, and using a DASH diet may improve outcomes in some high-risk populations such as Blacks and people with hypertension. ,
Being overweight (BMI 25 to 29) or obese (BMI >30) are both associated with an increased risk of stroke, particularly ischemic stroke. This is being seen with increased frequency in young adults, where obesity and CVD risk factors are increasing (see Chapter 30 ). A reduction in BMI and weight has been associated with a reduction in BP and in some cases a reduced risk of stroke. It is difficult to separate the effects of weight loss on various stroke risk factors such as BP, lipid status, exercise, etc. But overall aggressive weight loss combined with a healthy diet and exercise may mitigate some of the stroke risk in a general population.
Lack of physical activity and a sedentary lifestyle have been associated with an increased risk of stroke (see Chapter 32 ). Although rigorous randomized studies have not proven that exercise reduces the incidence of a primary stroke, current AHA/ASA recommendations support vigorous exercise 3 to 4 days/week for at least 40 minutes to combat the negative effects of physical inactivity. To the extent that lack of exercise leads to weight gain, obesity, diabetes, and other detrimental cardiovascular outcomes, the AHA recommendations are quite reasonable. A summary of lifestyle interventions to reduce stroke are shown in Table 45.9 .
Obstructive sleep apnea (OSA) is emerging as a common risk factor for stroke as well as for ischemic heart disease and all-cause mortality (see Chapter 89 ). However, it is often not recognized, not diagnosed, or not properly treated. OSA is related to obesity as well as CVD and related conditions such as diabetes. Furthermore, there appears to be a dose-effect relationship, with more severe OSA being associated with high rates of stroke, CVD events, and death. Patients with severe sleep apnea appear to have worse outcomes after a stroke. OSA can be treated using weight loss, continuous positive airway pressure, and other devices and approaches. Research is underway to determine how treatment of OSA may affect primary and secondary stroke prevention.
Stroke incidence and mortality are elevated on the Stroke Belt region of the United States, which generally encompasses the southeast region from Washington, DC to Florida and west to Texas. Within the Stroke Belt, there is a “belt buckle” that is generally defined as eastern regions of North Carolina, South Carolina, and Georgia. Studies have determined that demographic imbalances, an excess of CVD risk factors, and socioeconomic factors largely explain the excess stroke risk in the Stroke Belt.
Elevated homocysteine is associated with an increased risk of cardiovascular ischemic events, including ischemic stroke. Mutations in the MTHFR gene can lead to elevated homocysteine levels that are associated with an increased risk of ischemic vascular events such as stroke and MI. Elevated homocysteine can occur without an underlying gene mutation. Detailed analysis of this association after controlling for confounding factors has shown that it is most pronounced in younger patients with hypertension. Although treatment with multivitamins such as B 6 , B 12 , and folate is successful in reducing homocysteine levels, it is unclear if this leads to a reduction in ischemic vascular events. The recent Chinese Stroke Primary Prevention Trial did show some benefits of folate or B 12 supplements in some groups who had not received folate or B 12 supplements in the past.
There are a number of generally nonmodifiable risk factors for stroke (see Table 45.6 ). They include age, low birth weight, race/ethnicity, and a host of genetic factors ( Table 45.10 ). Age is the most important nonmodifiable stroke risk factor. Studies have shown that in general the risk of stroke doubles every 10 years above the age of 55 in men and women. However, there are also trends toward more strokes occurring at somewhat younger ages. This may reflect earlier onset of stroke risk factors as well as environmental influences. Approximately 10% of strokes occur in persons 18 to 50 years of age.
| Vasculopathies | Clotting | Blood Diseases | Metabolic | Other |
|---|---|---|---|---|
| CADASIL | Prothrombin gene mutation | Sickle cell disease | Hyperhomocysteinemia | Fabry disease |
| CARASIL | Factor V mutation | Hemoglobinopathies (thalassemia) | Diabetes | MELAS |
| RVCL | Antiphospholipid antibodies and lupus anticoagulants ∗∗ | Hyperlipidemia | Marfan syndrome | |
| Moya-moya disease | Protein C and S deficiency | Renal artery stenosis | ||
| Antithrombin III deficiency |
∗ Only the most common genetic disorders are listed. Clotting disorders are typically more common with venous (not arterial) mechanisms.
There are some genetic factors and diseases that increase stroke risk and may be amenable to therapy. These are listed in Table 45.10 . Genetic factors also play a variable role in some traditional risk factors such as hypertension, diabetes, and hyperlipidemia, among others. Specific mutations may lead to the premature development of a risk factor, or a severe form of the phenotype. In other cases, a gene mutation leads to a specific disease that directly causes a stroke. Examples include CADASIL, Fabry disease, and sickle cell disease. Other disorders such as hypercoagulable conditions may be inherited or sporadic. Sickle cell disease is common in Black patients and carries an increased risk of ischemic and hemorrhagic stroke. The judicious use of regular blood transfusions may reduce the risk of strokes. Gene therapy is also being explored for the long-term treatment of patients with sickle cell disease.
An acute or recent infection with COVID-19 appears to be a newly appreciated stroke risk factor (see Chapter 94 ). Stroke (mostly ischemic) can be seen in up to 1% of patients with an acute COVID-19 infection. Overall, about 75% of the strokes are ischemic, 21% hemorrhagic, and 4% CVST. The ischemic strokes tend to be large vessel, but all sizes are possible. Most of the strokes occur while the patient is hospitalized for severe COVID disease. The mechanism in some cases is thought to be increased coagulability and/or inflammation. The use of some COVID-19 vaccines (those with an adenovirus vector) is associated with rare cases of CVST and thrombocytopenia, perhaps mediated by antibodies to platelet factor 4.
Antithrombotic agents (antiplatelet therapy and anticoagulation) are key for the acute therapy, primary prevention, and secondary prevention of ischemic stroke. This section will address these various scenarios.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here