Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Plain radiographs are often used in the postoperative abdomen to evaluate lines and tubes, bowel gas pattern, retained foreign bodies, and the presence of pneumoperitoneum.
Fluoroscopic upper gastrointestinal (GI) examination with water-soluble or barium enteric contrast can be used to evaluate for leaks in the areas of postoperative change. Depending on the institution, postoperative “leak studies” may be routine following certain procedures (such as roux-en-Y gastric bypass or sleeve gastrectomy). Fluoroscopic enema examination with water-soluble contrast can be used to evaluate a low anterior resection before diverting ostomy takedown. Loopograms can be used to evaluate ileal conduits following cystectomy if there is concern for stricture or recurrent disease.
Depending on the surgical procedure, ultrasound (US) can be used to image certain suspected postoperative complications. In the superficial soft tissues, ultrasound can be used to evaluate for localized fluid collections along the abdominal incision. Ultrasound can also be used to evaluate for large intraabdominal collections, although it has lower sensitivity in the detection of small volumes of fluid within the abdomen compared with computed tomography (CT).
CT plays a crucial role in the diagnosis and management of a variety of postoperative abdominal complications.
Aside from magnetic resonance cholangiopancreatography (MCRP), magnetic resonance imaging (MRI) plays a limited role in the postoperative abdomen.
Fluoroscopic examination in the setting of a suspected leak should always be performed initially with water soluble contrast.
If initial trial with water soluble contrast demonstrates no leak and suspicion for a leak remains low, barium may then be given.
CT with intravenous (IV) and enteric water-soluble contrast is ideal in evaluating for postoperative fluid collections and other potential complications in the postoperative abdomen.
Should extend from the dome of the diaphragm to the pelvic floor.
At least 500 mL of dilute water-soluble oral contrast media given 1 hour before scanning.
100 mL of IV contrast administered and scan performed in the portal-venous phase.
For assessing complications from urinary collecting system related procedures (cystectomy, etc.), consider CT urography protocol instead.
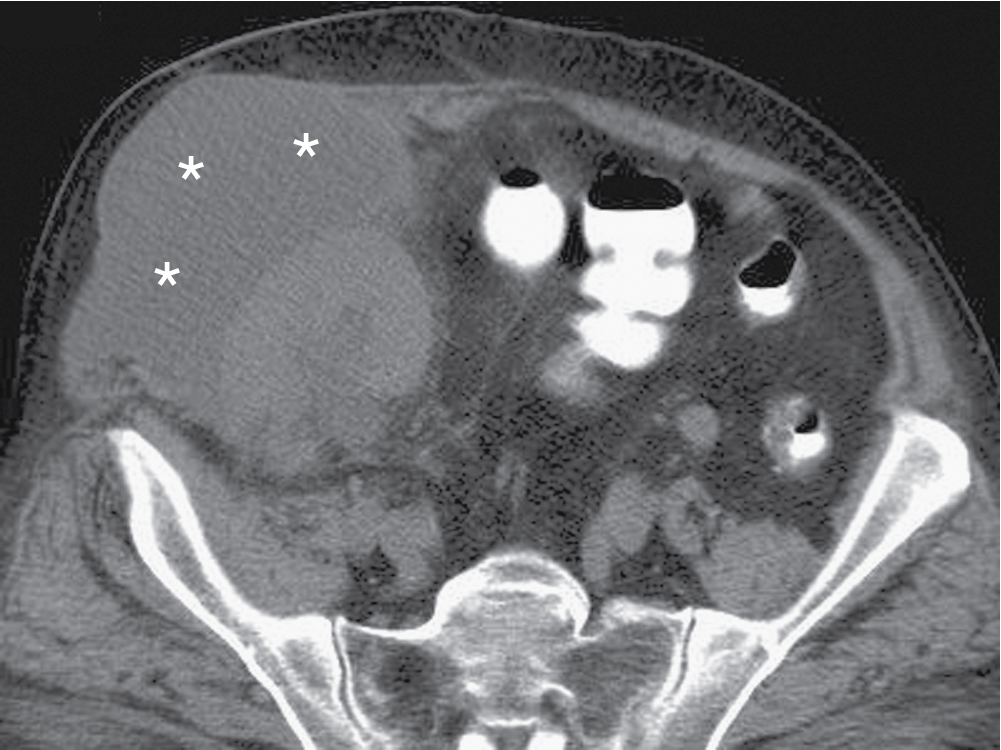
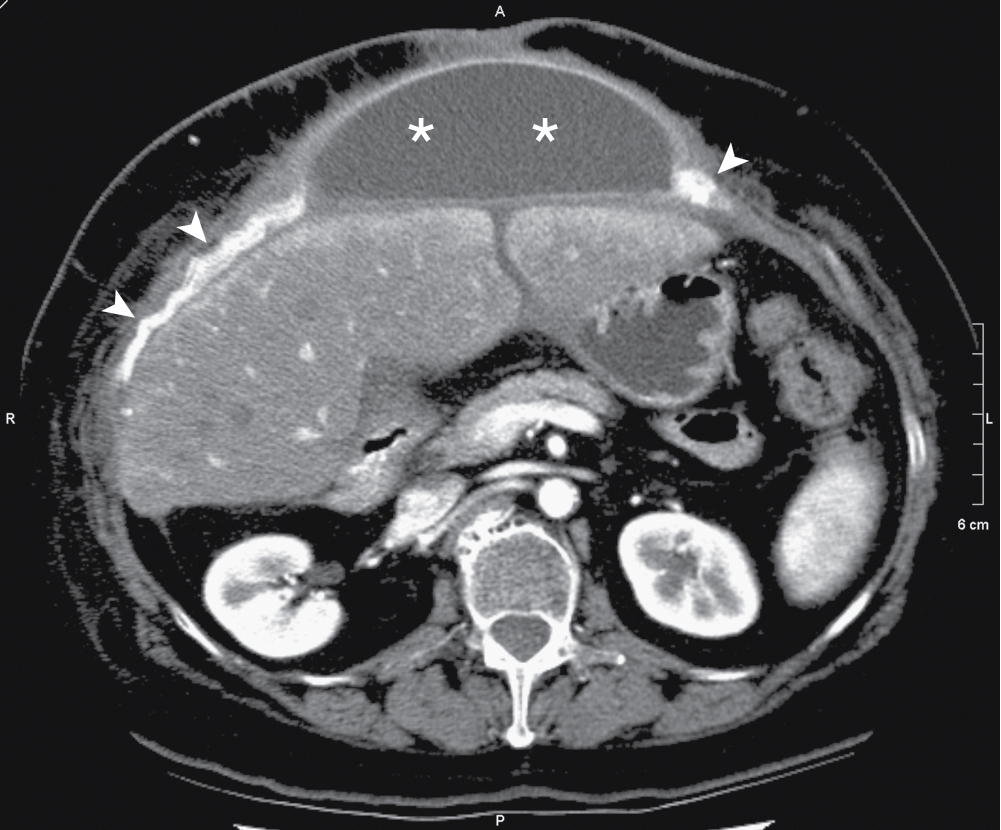
Postoperative seromas may be differentiated from abscesses with their lower attenuation values, typically in the 12 to 24 Hounsfield unit (HU) range ( Figs. 37.1 and 37.2 ).
Infections involving the incision are reported to be as high as 15% to 25% ( Fig. 37.3 ).
Although more easily identified by clinical examination, cross-sectional imaging can identify a drainable collection early for percutaneous intervention/drainage.
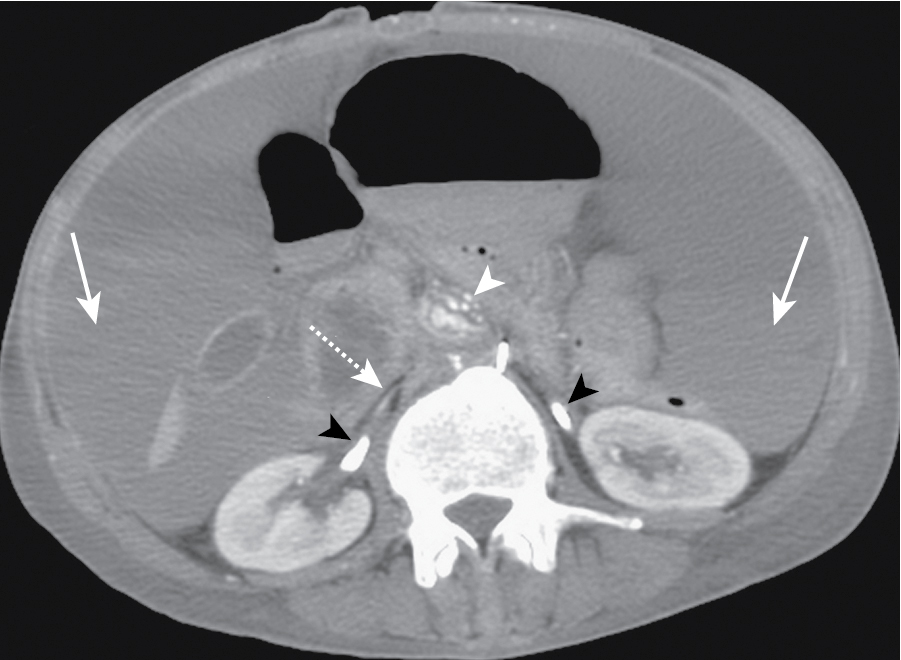
Rectus sheath hematomas may develop as the result of intraoperative injury to the epigastric vessels, and typically resolve within 2 weeks with conservative management ( Fig. 37.4 ).
Heterogeneous hypoechoic area with surrounding increase in vascularity.
Extent may be underestimated if large enough.
Peripheral rim enhancement of a collection suggests organized infection.
Small volumes of fluid and pneumoperitoneum can be seen in the immediate postoperative period following open or laparoscopic surgery.
Fluid is naturally absorbed by the peritoneal membrane, and should reduce spontaneously over the postoperative period.
Most accumulations of fluid are sterile (seromas), representing reactive fluid, appearing crescent-shaped and unencapsulated.
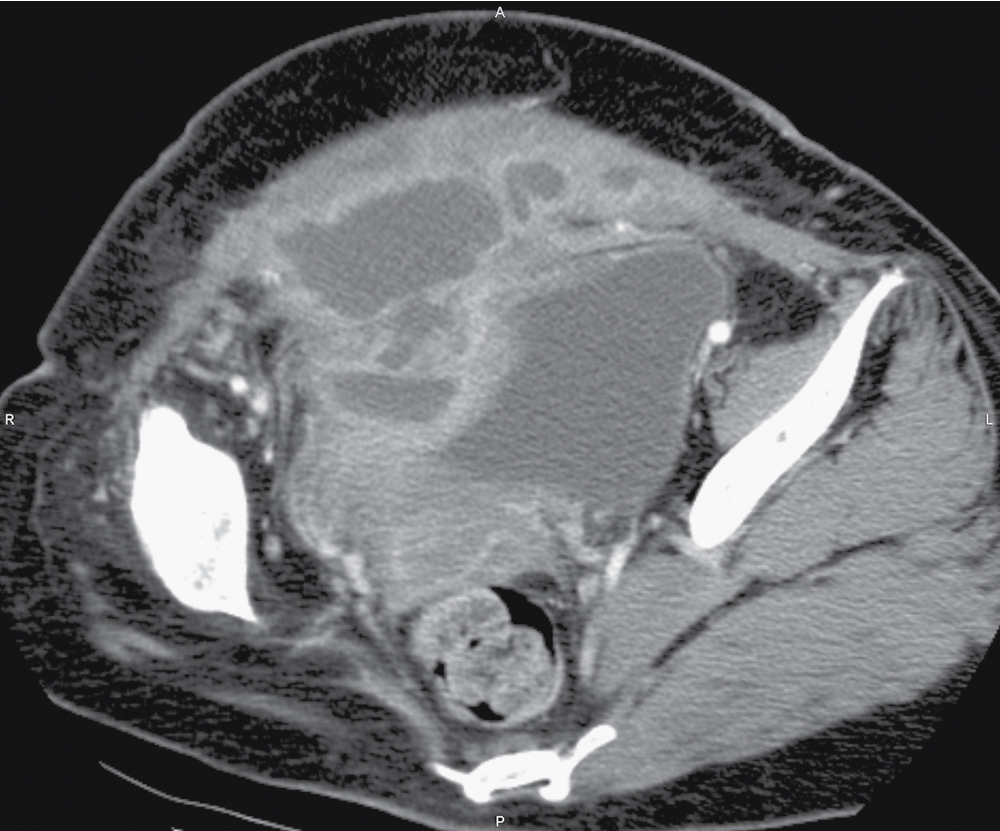
Abscess and pathologic fluid typically takes on an ellipsoid or spherical shape ( Fig. 37.5 ).
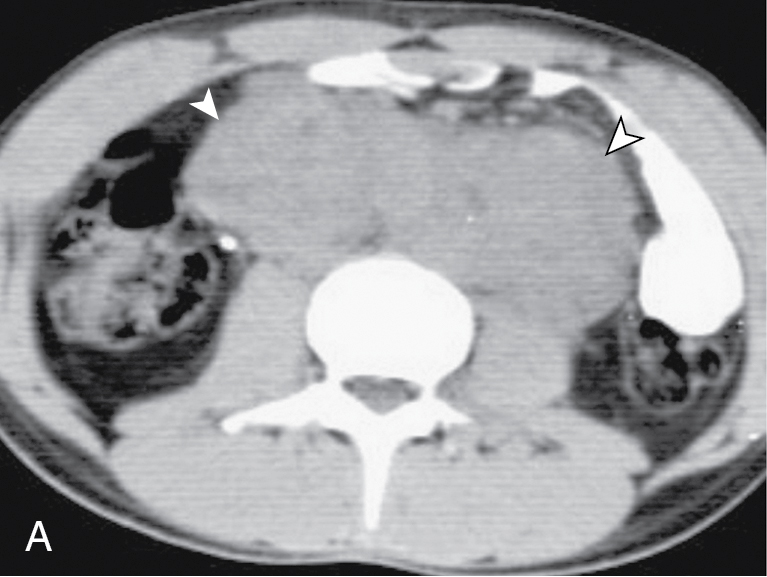
Hematomas/hemorrhage and extravasated enteric contents (such as from anastomotic leak) tend to be of higher density ( Fig. 37.6 ).
Not sensitive or specific for the detection of collections.
Abnormal mass effect on bowel and gasless areas can be a secondary sign in the presence of a large enough collection.
Can be used to follow large collections, especially if ionizing radiation is a concern (such as in the pediatric population).
Primary way of detecting and measuring intraabdominal fluid collections.
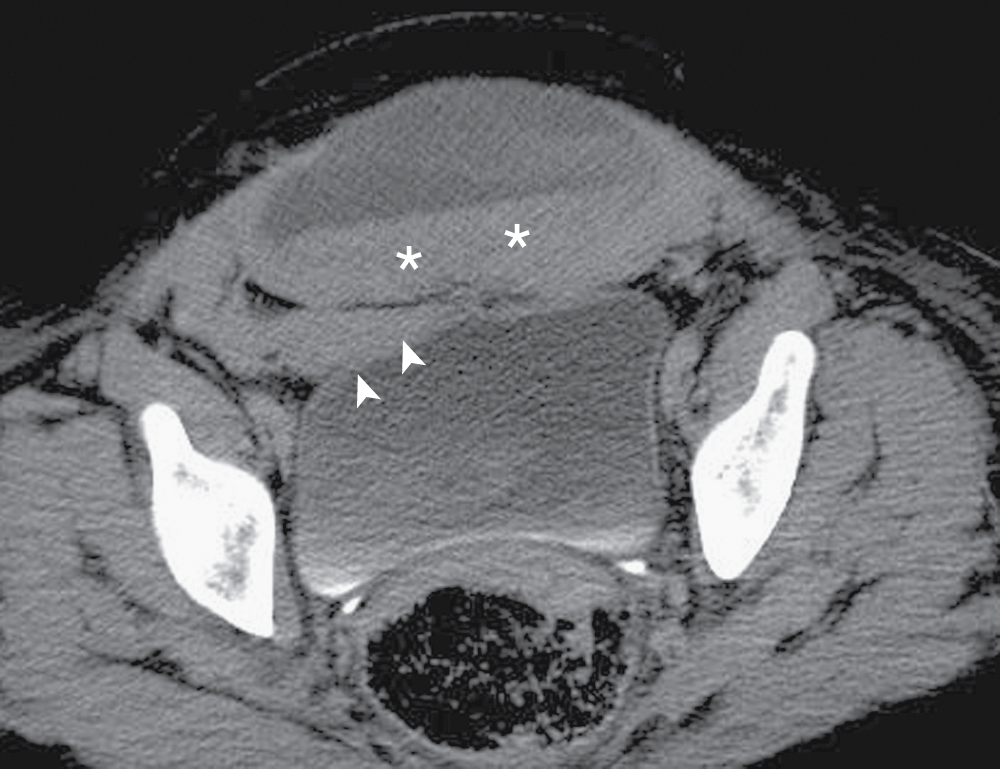
Peripheral rim enhancement of a collection suggests infection ( Fig. 37.7 ).
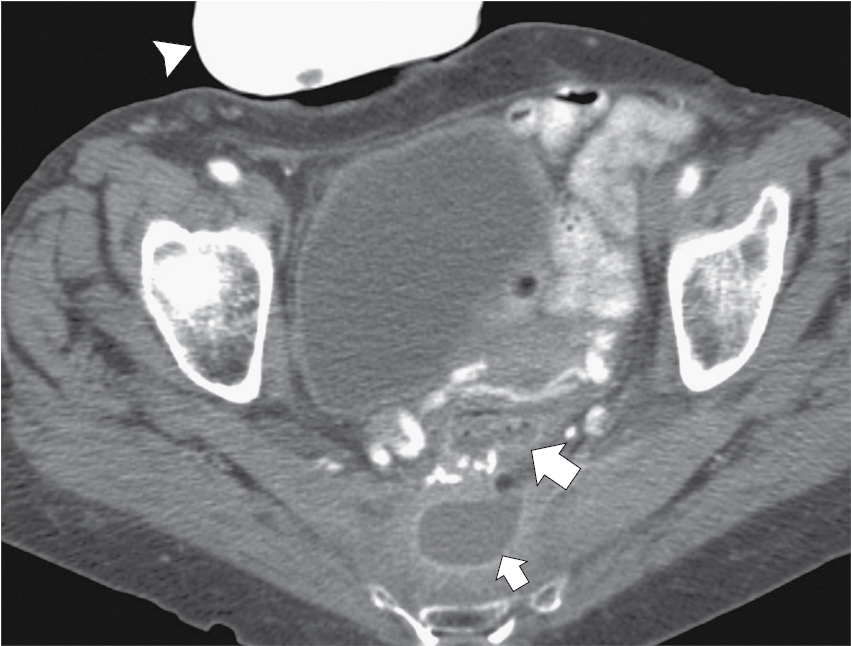
Presence of extravasated enteric contrast within the peritoneum can confirm anastomotic leak or viscus perforation ( Fig. 37.8 ).
Persistent or increasing pneumoperitoneum can also suggest the possibility of an anastomotic leak.
Can guide management with percutaneous interventional procedures and planning for placement/removal of drainage catheters.
Some hemostatic agents contain air and can mimic an abscess (e.g., Surgicel).
In the immediate postoperative period, manipulation of bowel can manifest as ileus.
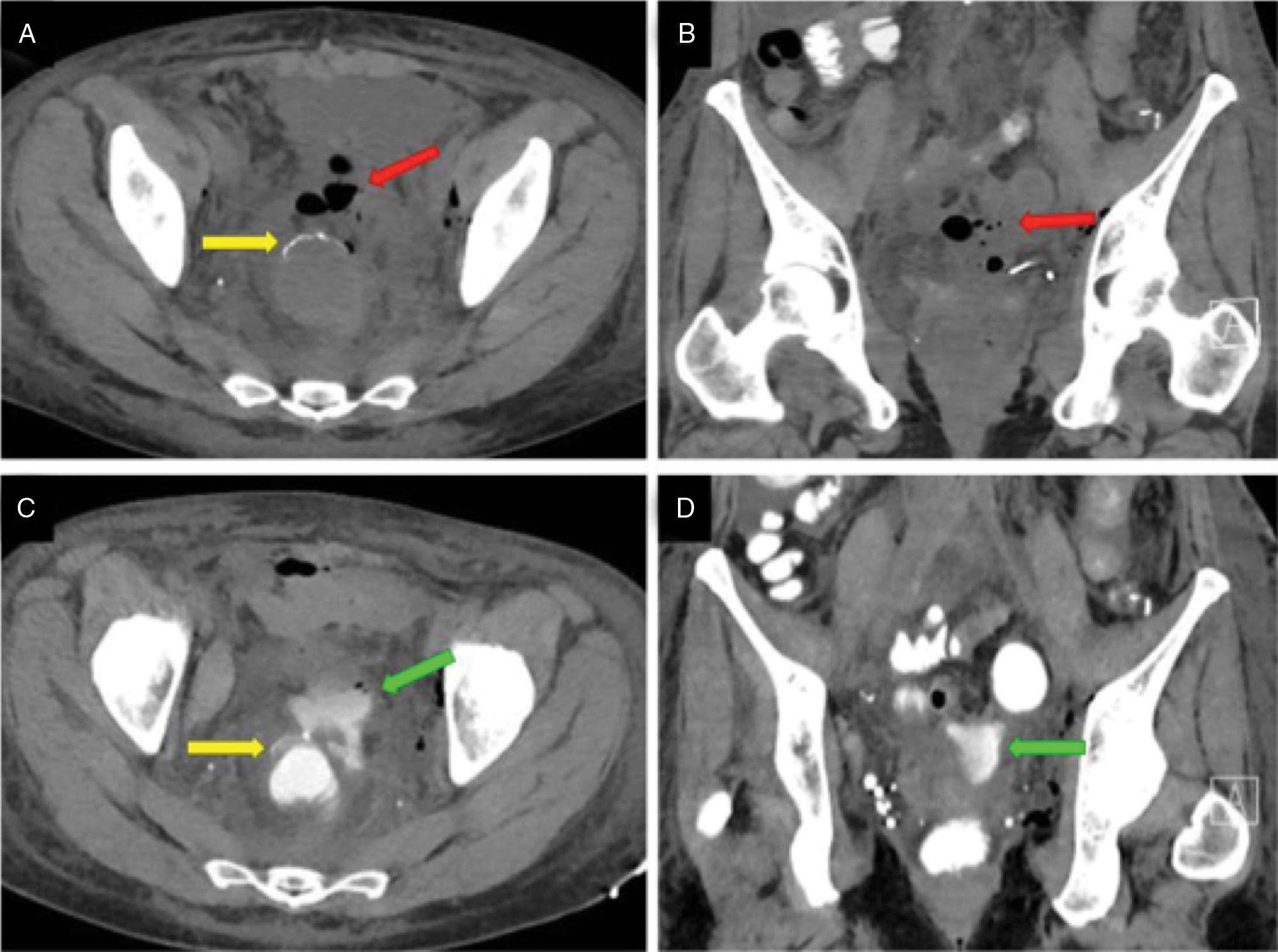
Mechanical small bowel obstruction may be the result of adhesions or internal hernias in the postoperative abdomen.
Please refer to chapter on Small Bowel Obstruction.
Retained surgical instruments or sponges are most frequently diagnosed in the intraabdominal cavity.
Can be asymptomatic or result in a granulomatous response with abscess development.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here