Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In recent years, there has been considerable growth in arthroscopic hip surgery as a modality for both investigation and treatment of hip pathology. In this chapter, the postoperative imaging appearances of the hip are described following arthroscopic surgery.
Postoperative MR arthrography in patients who have undergone traditional labral débridement portray the normal triangular labrum as a blunted structure with volume loss proportional to the degree of surgical resection. The residual tissue should still have decreased signal intensity on T1- and T2-weighted images, but the normal triangular morphology no longer exists. It is important to ensure that the residual labral tissue remains firmly adhered to the acetabular margin.
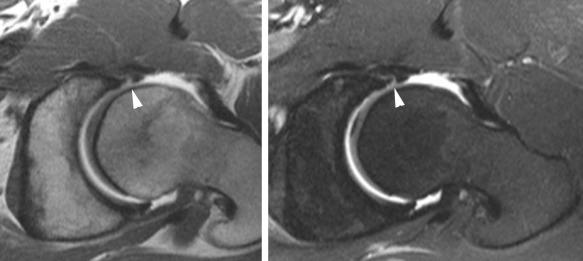
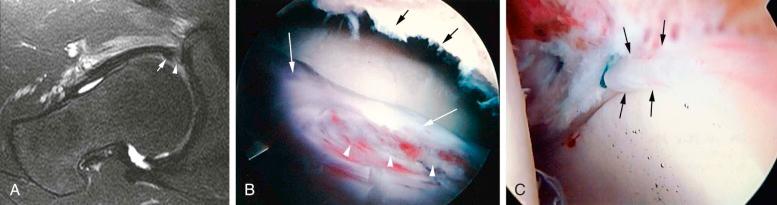
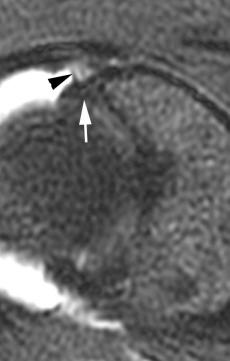
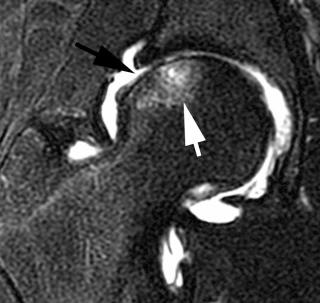
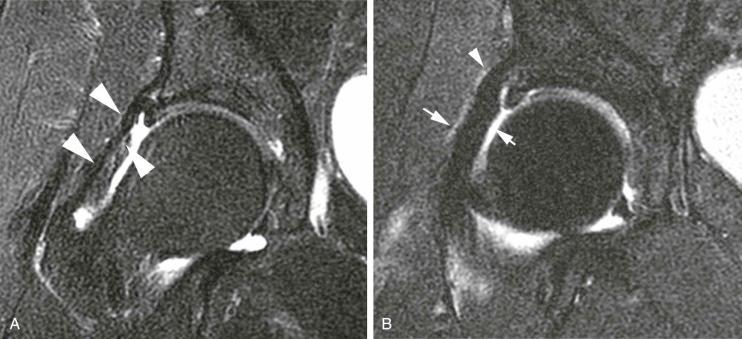
The postoperative appearance of the labrum that has undergone surgical intervention with suture banding or acetabular reattachment can have a different appearance. In these cases, the volume of labral tissue should be similar to that shown on preoperative imaging. The labral morphology, however, may be altered with loss of the normal triangular structure. The residual labral tissue should be closely approximated to the acetabular rim. Complications from prior surgery include primarily recurrent tears. Intrasubstance suture material may have mildly increased signal on long and short echo time sequences, which can last months or longer; but interposition of contrast/fluid between the labrum and the acetabular margin or within the labral tissue itself suggests recurrent detachment or tearing (see eFigs. 109-1 and 109-2 ). Postoperative adhesions may also occur between the labrum and capsule, which appear as thin, fibrous strands and may be symptomatic (see eFig. 109-3 ).
Femoroacetabular impingement can be treated through an arthroscopic or an open approach. In general, one can remove 30% of the diameter of the femur without risk of postintervention fracture. Postoperative radiographs can assess the degree of residual bony impingement ( Fig. 109-1 ). Postoperative appearances for arthroscopic repair demonstrate focal notched defects at the site of surgical intervention. Radiographs are obtained for documentation and assessment of the amount of bone removed. If symptoms persist, recurrent labral injuries can be a source of this pain.
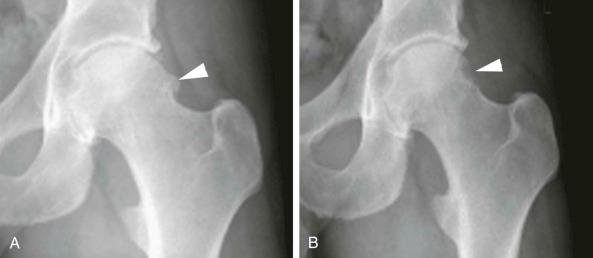
Postoperative fractures would be a potential complication but are very uncommon. Excessive bone removal can be detected with radiographs. Post-procedural avascular necrosis during long open procedures is also a theoretic concern that could be visualized with MRI. Intraarticular bleeding is a possible complication as well but rarely imaged. If the original symptoms persist, an MR arthrogram may demonstrate recurrent labral injuries or progression of chondrosis.
Postoperative imaging may also be performed in the evaluation of patients post-repair of ligamentum teres injury, post-capsular repair or post-microfracture repair of chondral defects. MR arthrography demonstrates uniform decreased T2 signal intensity following ligamentum teres repair. MR arthrography may also be used to identify recurrent tears.
MR is rarely used for imaging post-chondral repair because MR often underestimates the degree of chondrosis when compared with arthroscopy. Postoperative appearance of microfracture technique in the first few months includes subchondral marrow edema (see eFig. 109-4 ).
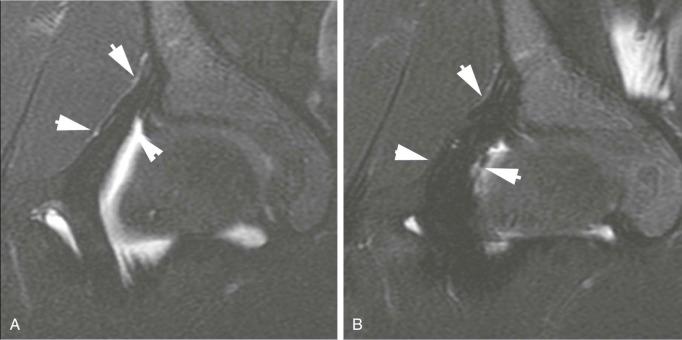
Following arthroscopic repair of capsular injury with thermal capsulorrhaphy or suture plication, the capsule may appear thicker than on preoperative images (see eFig. 109-5 ). Depending on the type of suture, there is minimal magnetic field inhomogeneity artifact (see eFig. 109-6 ).
Chondral injuries of the hip may be difficult to see because of the relative thinness and curvilinear articular surfaces of the hip with cross-sectional imaging. This area is not evaluated with weight-bearing anteroposterior views of the hip; therefore, cross-sectional imaging and/or arthroscopic visualization is needed when a chondral injury is clinically suspected and radiographs are negative. MR arthrography can help identify chondral injury; however, MR often underestimates the degree of chondrosis when compared with arthroscopy. Rarely is post-procedural imaging performed and in refractory cases only. Postoperative appearance of microfracture technique in the first few months includes subchondral marrow edema ( eFig. 109-4 ).
Although considered a stable joint because of large bony contact areas and coverage, the hip can be subject to soft tissue instability. The role of arthroscopic treatment is unclear at this time but consists of either thermal capsulorrhaphy or suture plication.
Postoperatively, the capsule appears thicker as compared with preoperative imaging, using either thermal treatment or plication ( eFig. 109-5 ). Depending on the type of suture, there is minimal magnetic field inhomogeneity artifact ( eFig. 109-6 ). Occasionally, patients may experience an inflammatory reaction, possibly to the suture material, and develop synovitis, resulting in hip pain. This is not seen on conventional MR arthrography. Postcontrast imaging with an intravenous contrast agent may have a role. Occasionally, additional surgery may be needed to remove excessive granulation tissue.
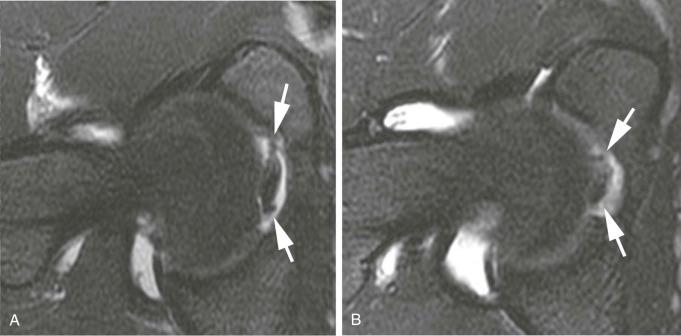
Tears of the ligamentum teres are a recently recognized source of hip pain. In one large series, this was the third most common cause of hip pain among athletes. Other studies have shown that tears of the ligamentum teres can affect at least 8% of patients. These tears have been arthroscopically classified previously as complete, partial, and degenerative. Partial tears of the ligamentum teres are often treated by débridement with an arthroscopic shaver to remove excessive or irregular tissue, which may be a source of impingement or pain. Complete tears of ligamentum teres may also be resected and rarely reconstructed in patients in whom their hips undergo extremes of motion and are exposed to high axial forces, such as enthusiasts of the martial arts. Postoperative imaging is often unremarkable using MR arthrography. The ligament often has a smooth surface with decreased volume due to partial resection. Signal characteristics on MR arthrography demonstrate uniform decreased T2 signal intensity ( eFig. 109-7 ). Recurrent tears are a possibility.
No known complications of ligamentum teres débridement have been identified as of yet with MRI. Complications associated with arthroscopy, in general, however, remain.
Radiographic evaluation of the hip, both before and after any operative procedure, is the cornerstone of radiologic assessment. Radiographic evaluation serves as the first line of investigation in the postoperative hip, providing an overall view of the hip joint, where the diagnosis is often made, before the introduction of cross-sectional imaging, which may be used for disease confirmation and determination of severity and extent. The relative ease of radiographic comparison allows for accurate monitoring of disease progression. Importantly, in the post-arthroplasty patient, subtle changes are often indicators of loosening and therefore hardware failure. More sophisticated imaging and image-guided interventions may then be used to determine the cause of hardware failure, primarily to exclude sepsis.
The high prevalence of hip pathology and the general success of hip replacement surgery have resulted in hip arthroplasty becoming a routine procedure, with an estimated 170,000 procedures performed on an annual basis in the United States as a primary procedure and approximately 35,000 as revision surgery. Although the types of prostheses continuously evolve, hip prostheses may be divided simply into unipolar, bipolar, and total arthroplasty, with the latter further divided into metal on polyethylene, metal on metal, and ceramic on ceramic systems. Hip fractures requiring orthopedic fixation are also very common, with many types of internal fixation devices currently available. Given sufficient time, all prostheses and fixation devices eventually fail. Because component failure may have a protracted subclinical course, detecting any findings of malfunction relies heavily on routine radiographic assessment. Although these findings may be subtle, a high index of suspicion of hardware failure is critical. Close monitoring is paramount to prevent complications, which may limit the success of possible future revision surgery, such as the loss of adequate bone stock.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here