Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]()
Glaucoma drainage devices (GDDs) are a very important and effective tool for glaucoma surgery, especially in complicated and secondary glaucoma. Complications are not uncommon and are varied in nature. The risk of many of the complications associated with the used of these devices may be minimized and most complications can be managed while maintaining good success rates. The use of GDDs for the treatment of less advanced glaucoma might change the complication profile. Postoperative complications have been shown to be a major risk factor for failure of GDD surgery. Consequently, the focus should be on avoiding complications by a careful preoperative plan, detailed surgical technique, and watchful postoperative care in order to obtain the best possible result for the eye and the patient.
Glaucoma drainage devices (GDDs) have become the surgical procedure of choice for many types of glaucoma such as neovascular, uveitic, congenital or infantile with failed trabeculotomy, iridocorneal endothelial syndrome, glaucoma related to penetrating keratoplasty, keratoprosthesis or following retinal detachment repair. Additional indications include contact lens dependence, chemical burns, surface disease, or trauma precluding standard surgery. More recently, drainage devices have been used as primary surgical therapy as an alternative to trabeculectomy in cases of primary or secondary open- and narrow-angle glaucoma.
The evolution of surgical indications and surgical techniques of GDDs has led to a change in the profile of complications seen. Some complications are seen more often with certain devices or due to implantation technique, but most are seen with all GDDs. Postoperative complications have been shown to be statistically related to failure of glaucoma control. Two major randomized, controlled clinical trials recently reported results, including complications. The Tube Versus Trabeculectomy (TVT) study compared the Baerveldt 101-350 (BGI 350) with trabeculectomy in eyes with prior eye surgery and has published its 5-year results, while the ABC study compared the Ahmed valve FP7 and the Baerveldt 101-350 and has published one year results.
Complications of tube shunt surgery can be divided by anatomical location or mechanism ( Box 116-1 ). Table 116-1 is a comparison of the rates of the most common complications. The surgeon performing tube shunt surgery must be aware of the possible complications and minimize their incidence by careful and detailed surgical planning and patient selection.
Mechanical
Diplopia
Ptosis
Acquired Brown's syndrome
Proptosis
Extrusion or exposure of plate
Infectious
Orbital cellulitis
Endophthalmitis
Inflammatory/scarring
Reactivation of prior existent orbital myositis
Encapsulated cyst or fibrosis over plate
Fibrovascular growth into plate
Eyelid extension of filtering bleb
Bleeding
Peribulbar/retrobulbar hemorrhage
Mechanical
Peritubular filtration
Tube kinking
Obstruction of internal ostium by iris, blood, fibrous membrane, vitreous, silicone
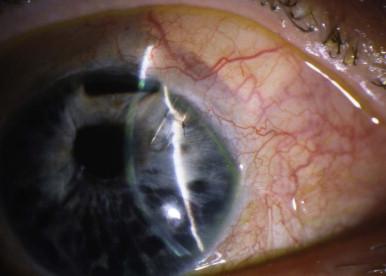
Corneal touch or erosion
Misshaped pupil
Tube migration out of the anterior chamber
Capsular bag distention syndrome (CBDS) with shallow AC (combined with phaco/IOL)
Corneal drying/dellen
Inflammation/scarring
Corneal decompensation
Fibrous ingrowth into the tube external ostium
Epithelial downgrowth
Bleeding
Hyphema
Flat AC
Choroidal effusion
Wound leak
Short-term IOP raise or hypertensive phase
Encapsulated bleb
Retinal detachment
Vitreous hemorrhage
Choroidal effusion
Delayed suprachoroidal hemorrhage
Endophthalmitis
Aqueous misdirection/malignant glaucoma
Hypotony maculopathy
Macular edema
Decompression retinopathy
Cataract
Phthisis
Ripcord suture migration
Ripcord suture hypopion
| Author Date Type | GDD Type | Patients F/U Time (mean) | Extrusion Exposure Plate/Tube | Hyphema (%NVG) | Persist. Diplopia | NLP | Choroidal Effusion Early/Late | Persist. Corneal Edema (%PK) | Shallow Anterior chamber | Tube Occlusion | Endophthalmitis | RD | Supra-choroidal Hemorrhage | Persistent hypotony | Cystoid Macular Edema | Hypotony Maculopathy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gedde 2007 Prospective | Baerveldt 350 | 107 eyes 1 year results | 0% | 2% (0%) | 5% | 0% | 16% | 7% (0%) | 11% | 0% | 1% | 1% | 2% | 0% | 3% | 1% |
| Gedde 2009 Prospective | Baerveldt 350 | 107 eyes 3 year results | 5% | 2% (0%) | 5% | 0% | 16% 2% |
9% (0%) | 1% | 3% | 1% | 1% | 0 | 5% | 1% | |
| Budenz 2011 Prospective | Baerveldt 350 | 133 eyes 1 year | 1% | 17% (29%) | 8% | 5% | 10% 2% |
12% (NR) | 20% | 9% | 2% | 0% | 2% | NR | 2% | 2% |
| Ahmed FP7 | 143 eyes 1 year | 1% | 9% (29%) | 10% | 1% | 15% 1% |
6% (NR) | 19% | 2% | 0% | 2% | 0% | NR | 6% | 3% | |
| Gedde 2012 Prospective | Baerveldt 350 | 107 eyes 5 years | 5% | 2% (0%) | 6% | 0% | 14% 2% |
13% | 1% | 3% | 1% | 1% | 0% | 1% | 5% | 1% |
| Harbick 2006 Retrospective | Baerveldt 250–425 Infranasal | 182 eyes 19 ± 15 months | <1% | 7.5% (NR) | 2% | 1% | 6% | 10% (2%) | NR | 4.3% | <1% | <1% | 2% | 1% | 3% | NR |
| Wilson 2003 Prospective | Ahmed S2 | 59 eyes 31 months | 5.1% | 16.9% (0%) | 0% | 0% | NR | 0% (0%) | 15% | 0% | 0% | 0% | 0% | 0% | 0% | 0% |
| WuDunn 2006 Retrospective | Baerveldt 250 | 108 eyes 23 months | 1.8% | 21% (35%) | 4% | 1% | 7.4% | 5.5% (9.2%) | NR | 11% | 0% | 3% | 4% | 4% | 0% | NR |
| Broadway 2001 Retrospective | Molteno Single-plate | 119 eyes 43 months | 7.6% | <1% (16%) | 2.5% | NR | 15% | 10% (20%) | 7.6% | 8.4% | 0% | 5% | <1% | 0% | 0% | 0% |
| Topouzis 1999 Prospective | Ahmed S2 | 60 eyes 30.5 months | 0% | 20% (23%) | 2% | 3% | 23% | 27% (26%) | NR | 12% | 0% | 3% | 2% | 0% | 2% | 0% |
| Ishida 2006 Prospective | Ahmed S2 | 66 eyes 15months | 1.5% | 4.5% (12%) | 0% | 0% | 6% | 1.5% (3%) | 7.6% | 4.5% | 0% | 0% | 3% | 0% | 0% | 0% |
| Ahmed FP7 | 66 eyes 13months | 0% | 1.5% (21%) | 0% | 0% | 6% | 0% (4.6%) | 3% | 3% | 0% | 0% | 1.5% | 0% | 0% | 0% |
The most common early complications of tube shunt implantation are hypotony and associated problems. Until a fibrous tissue capsule forms around the plate to provide adequate resistance to flow, aqueous humor may flow through the tube more readily than desired. Even valved implants such as the Ahmed Glaucoma Valve (AGV) are at risk for hypotony-related complications during the early postoperative period.
In the TVT study, choroidal effusions and shallow or flat anterior chambers were the two most common postoperative complications of the Baerveldt 350 implant (BGI). Sixteen percent of eyes had at least one of these complications during the first postoperative month, although in most cases the problem resolved without intervention. The prevalence of hypotony is generally reported to be lower with the Ahmed Glaucoma Valve (AGV), especially the older S2 model. The one-year results of the ABC randomized trial comparing the BGI 350 with the newer AGV FP7 device showed a somewhat higher rate of choroidal effusion and shallow anterior chamber for the AGV than previously reported.
During the early postoperative phase, excess aqueous fluid leakage may occur (1) through tube fenestrations that are too large; (2) through the tube if not occluded with a ligature; or (3) around the tube through the sclerostomy, especially if performed with a needle larger than 23 gauge. Some eyes, particularly those with uveitis, ocular ischemic syndrome or following laser cyclophotocoagulation, may have reduced aqueous production and thus be more prone to hypotony following tube shunt implantation. Ahmed valves may be a better option for these cases.
Various methods are used to prevent early hypotony, especially for the non-valved implants such as the Baerveldt and Molteno devices ( Fig. 116-1 ). The most commonly used method is temporary ligation of the tube with an absorbable suture ligature that dissolves in 4–6 weeks along with anterior fenestrations of the tube for early IOP control. Other methods include a two-stage procedure, which requires a return to the operating room, and filling of the anterior chamber with high-viscosity viscoelastic substances.
Early postoperative hypotony following tube shunt surgery usually resolves without intervention within a few weeks as the fibrous capsule forms around the plate. Thus, in most cases, hypotony can be treated with cycloplegia to maintain the anterior chamber and restriction of patient activities that involve Valsalva-type movements. However, the presence of hypotony increases the risk of more severe complications such as flat anterior chamber, corneal decompensation or suprachoroidal hemorrhage. Thus, it may be prudent to correct the hypotony in patients at high risk for these complications. The simplest procedure to treat hypotony is injection of a high-viscosity viscoelastic solution into the anterior chamber. Since the effect of this injection will only last a few days, multiple injections may be needed. However, by 1–2 weeks following the tube shunt surgery, a fibrous capsule has usually started to form around the plate to maintain an adequate intraocular pressure and formed anterior chamber.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here