Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The science and practice of modern neonatology evolved as a medical specialty in the United States and the Western world over the last 70 years. Neonatology as a specialty in developing countries is still evolving. The increased attention to improving newborn care at a global level can be traced to the recognition by the World Health Organization (WHO) of unacceptably high infant mortality in low- and middle-income countries (LMICs). The Alma Ata Declaration was the first serious effort by WHO to address the problem of high infant mortality rate (IMR) among developing countries. Since then, several policies have been proposed and implemented to decrease the IMR and neonatal mortality rate (NMR) across the globe. Since the latter part of the twentieth century, there has been steady improvement in overall global newborn care resulting in the reduction of NMR and IMR in LMICs. These developments can be attributed to rapid globalization of health-related information and technology from developed high-income countries (HICs) to LMICs. Also, increased awareness of health and change in health care–seeking behavior among women during the past decade has improved maternal and child health. The major factors responsible for overall improvements in maternal and child care in LMICs probably include: (1) improved access to medical and technical information, (2) rapid transfer of technology, and (3) international campaigns such as the advocacy of the Millennium Development Goals (MDGs) and the Sustainable Development Goals (SDGs). Several large controlled trials have demonstrated the benefits of selected interventions, including packages of care such as the Mother-Baby Package and the Essential Newborn Care program. Considerable progress is being made in reducing maternal and child mortality in developing countries; however, many challenges remain. This chapter provides an overview of global neonatal and perinatal problems, presents data on the changing trends in IMR and NMR, and discusses strategies to decrease the IMR and NMR in developing countries.
Because of concerns of high global IMR, numerous interventions have been proposed and implemented by world organizations over the past four decades ( Table 8.1 ). The Alma-Ata Declaration of 1978 by the WHO and the United Nations Children's Fund (UNICEF) set a goal to achieve “Health for all by the year 2000.” The declaration included a goal for the reduction of maternal and infant mortality through primary care. In 1987, the International Conference on Safe Motherhood drew attention to high maternal mortality rates (MMRs) in developing countries and encouraged policymakers to develop new strategies to reduce maternal mortality. This action led to the worldwide program of Safe Motherhood, placing an emphasis on antenatal care. A similar resolution, the Bamako Initiative, was instituted at the annual meeting of the African Ministries of Health in 1987. The objective was the achievement of universal maternal-child health coverage at the periphery by 2000. In 1988, the Task Force for Child Survival set objectives for a reduction in MMR and IMR. One of these objectives was a worldwide reduction in mortality by at least half, or by 50 to 70 per 1000 live births, whichever can be achieved first, for children 5 years old and younger. Another objective was the reduction of MMR worldwide by at least half.
| Initiative | Organization | Year and Occasion | Goals |
|---|---|---|---|
| Declaration of Alma-Ata | WHO, UNICEF | Sept 1978, USSR, International Conference on Primary Health Care | Health for all by 2000 |
| Safe Motherhood Initiative | WHO, UNICEF, UNFPA, World Bank, and others | 1987, Nairobi, International Safe Motherhood Conference | Reduce maternal mortality to half the present rate by 2000. |
| Bamako Initiative | UNICEF, WHO | September 1987, Bamako, Mali, Annual Meeting of African Ministers of Health |
|
| Task Force for Child Survival | WHO, UNICEF, World Bank, UNDP, Rockefeller Foundation | March 1998, Talloires, France, Protecting the World's Children, an Agenda for the 1990s |
|
| Mother-Baby Package | WHO | Sept 1994, Cairo, International Conference on Population and Development | Reduce maternal mortality to half of 1990 levels by 2000. |
| Reduce perinatal and neonatal mortality from 1990 levels by 30%-40% and improve newborn health. | |||
| Making Pregnancy Safer | WHO | 1999, Safe Motherhood Initiative | Accelerate reduction of high maternal and perinatal mortality and morbidity by refocusing WHO strategies in national and international health sectors. |
| Millennium Development Goals | WHO | 2000-2015 |
|
| Newborn Care Training | NIH | 2010 | Essential newborn care training of community-based birth attendants has reduced the stillbirth rate. * |
| Sustainable Development Goals | WHO | 2015-2030 |
|
* From Carlo WA, et al. Newborn-care training and perinatal mortality in developing countries. N Engl J Med . 2010;362:614.
In 1994, WHO developed the Mother-Baby Package to help reduce MMR and NMR further. Recognizing that MMR remained high, in 1999 WHO re-emphasized the need for an acceleration of national and international efforts to decrease MMR and perinatal mortality rate through the Safe Motherhood program. At the 48th World Assembly of WHO, the concept of integrated management of childhood illness was adopted to improve the well-being of the whole child younger than 5 years old. This concept included an emphasis on improved care of newborns. By the end of the twentieth century, a significant decrease in MMR and IMR was reported as one of the top 10 achievements of the century. However, the high IMR and NMR in the LMICs continued to be a major concern to global policymakers. The World Bank initiated the Global Burden of Disease study, which showed that perinatal conditions, including infant mortality, form a significant portion (39%) of the global burden of disease. It showed that developing countries are the major contributors to global perinatal and neonatal mortality. Perinatal mortality constitutes one of the 10 leading causes of death in developing countries. Neonatal mortality is the major part of perinatal mortality. These findings underscore the importance of improving perinatal and neonatal care in developing countries, as declared in the MDGs in 2000.
In 2000, the United Nations developed eight MDGs to be achieved by 2015. The targets were measured by preset quantifiable measures. The MDGs focus on some specific health issues but also emphasize social, economic, and public health and health-policy matters that affect the “health” of the people and addressed specific indicator goals for perinatal care ( Table 8.2 ).
| Goals | Targets | Indicators |
|---|---|---|
| MDG Goal 4 Reduce child mortality |
Reduce the under-5 mortality rate by two-thirds between 1990 and 2015. | Under-5 mortality rate (deaths per 1000 live births) |
| Infant mortality rate (deaths per 1000 live births) | ||
| Proportion of 1-year-old children immunized against measles | ||
| MDG Goal 5 Improve maternal health |
Reduce the maternal mortality rate by three-fourths between 1990 and 2015. | Maternal mortality ratio (deaths per 100,000 live births) |
| Proportion of births attended by skilled health personnel | ||
| SDG Goal 3 Good health and well-being |
|
Maternal mortality ratio (deaths per 100,00 live births) |
| Neonatal mortality rate (deaths per 1000 live births) | ||
| Under-5 mortality rate (deaths per 1000 live births) |
In addition to these developments, the series of landmark scientific publications in The Lancet provided evidence-based scalable interventions that could reduce NMR and IMR in resource-poor countries. These publications generated great interest among researchers and health policymakers around the globe. The Child Survival series examined the potential impact of scaling up 43 interventions that could reduce child mortality by 2015. In 2005, the series on newborn survival provided the first systematic estimates of neonatal deaths by cause and identified simple and cost-effective scalable interventions that could reduce neonatal deaths globally. The impact of some of the suggested interventions is described in the later part of this chapter.
In 2015, the United Nations proposed the Sustainable Developmental Goals (SDGs) to be achieved by 2030. These goals were adopted to end poverty, protect the planet, and ensure prosperity for all as part of a new sustainable development agenda. Each goal has specific targets to be achieved over the next 15 years. There are 17 goals ( Fig. 8.1 ). Goal 3 is focused on health and aims to ensure healthy lives and promote well-being for all at all ages. This goal includes specific targets for perinatal and childhood health outcomes. The maternal and childhood targets aim to reduce global maternal mortality ratios to less than 70 per 100,000 live births and end preventable deaths of newborns and children under 5 years of age, with all countries aiming to reduce neonatal mortality to at least as low as 12 per 1000 live births and under-5 mortality to at least as low as 25 per 1000 live births. These aspiring goals are ambitious and will require commitment from all stakeholders to achieve them.
Worldwide efforts are taking place to implement SDGs and track their impact. There is a need for accurate birth and death data from all participating countries. Unfortunately, collecting accurate NMR, IMR, and under-5 mortality data on a global scale remains a major problem. There are several hurdles to collect these data accurately. Whereas high-income countries have well-established vital statistics of births and deaths, the LMICs do not. Ostergaard and co-workers found that only 60 of the 193 countries studied had fully functioning sources of mortality data ; the rest of the countries depend on annual or periodic surveys. There is a need for improvement in accurate vital statistics to establish the true burden of MMR, NMR, and IMR and to develop appropriate strategies to monitor progress.
Maternal mortality has been a major global burden of disease. At the time of and preceding the declaration of MDGs, more than 600,000 women were dying annually from causes related to pregnancy and childbirth. Asia and Africa had the highest MMR and the highest number of maternal deaths, compared with only 4000 deaths per year in HICs. The causes of maternal death include maternal hemorrhage (25%), sepsis (15%), abortion (13%), hypertensive disorders of pregnancy (12%), and obstructed labor (8%). More than 50% of the deaths related to pregnancy and childbirth were estimated to be preventable using simple, well-accepted interventions. The MDG #5 aimed at reducing the MMR by 75% between 1990 and 2015.
On a positive note, global MMR in 2010 had decreased by 47% (from 400/100,000 in 1990 to 210/100,000), accounting for 287,000 maternal deaths in 2010. Although the overall number of maternal deaths has decreased, only 10 countries have reached the goal, 9 countries are “on track,” 50 countries are “making progress,” 14 countries have made “insufficient progress,” and 11 are categorized as having made “no progress” at all. Sub-Saharan Africa (56%) and South Asia (29%) continue to bear the major burden of global MMR (85%), accounting for 245,000 maternal deaths in 2010. Two countries, Nigeria and India, contribute one-third of the global MMR: India at 19% and Nigeria at 14%.
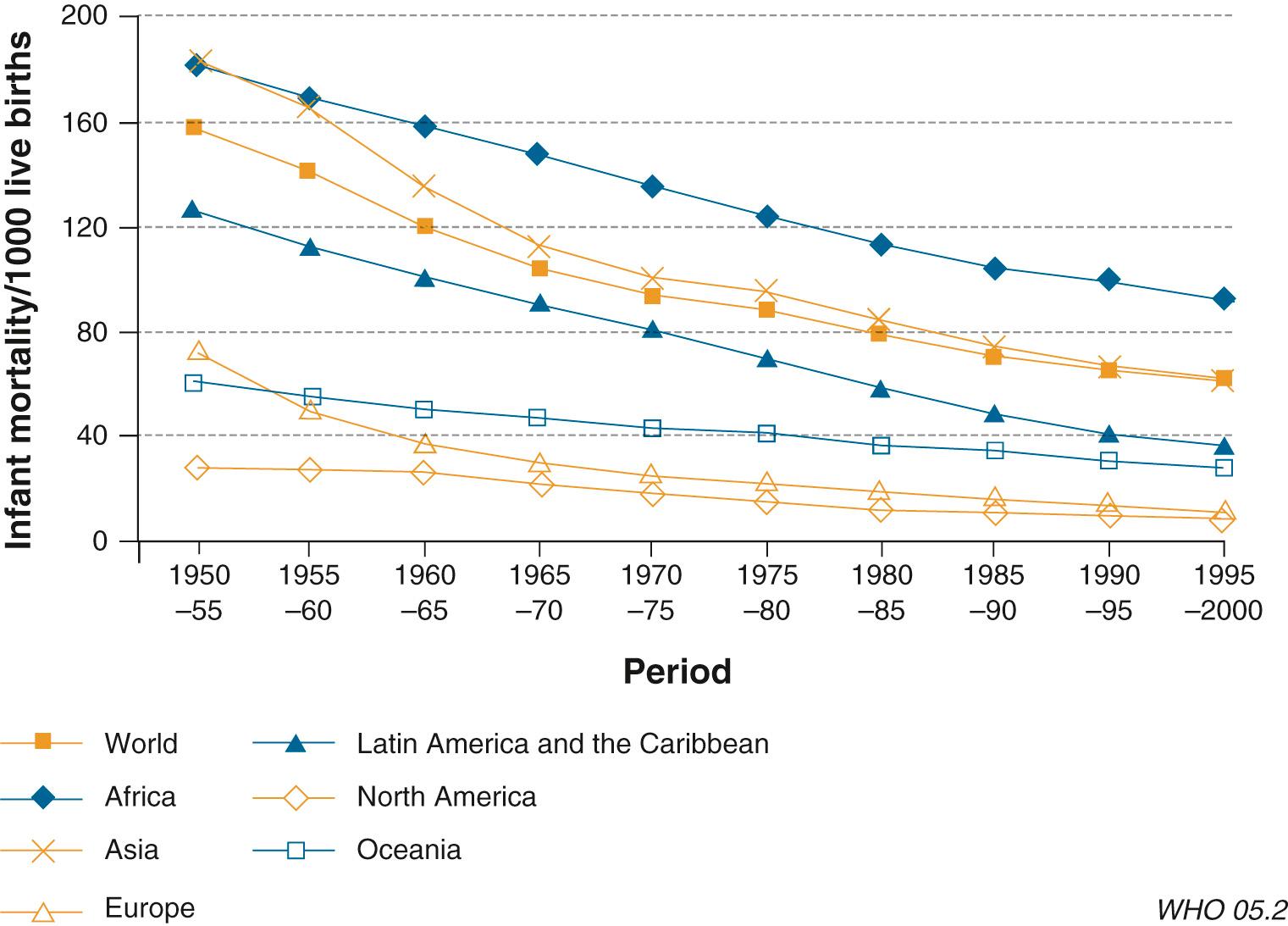
There are limited data on NMR or IMR that go back to the early twentieth century, but there were major reductions in mortality. Fig. 8.2 shows global trends in IMR during 1950 to 2000. In the 1950s, there were wide variations in IMR among different regions of the world. Infant mortality rate was lowest in industrialized Western countries (33 per 1000). It decreased to around 5 per 1000 by 2000, a reduction of 85%. In 1950, sub-Saharan Africa had the highest IMR (157 per 1000) and showed the least reduction (only 32%) among all the regions of the world during the next 50 years. South Asia, the Middle East/North Africa, and Latin America/Caribbean showed 53%, 70%, and 74% decreases, respectively. At the end of the twentieth century, IMR continued to remain significantly high: 70 per 1000 in South Asia, 45 per 1000 in the Middle East, and 27 per 1000 in Latin America.
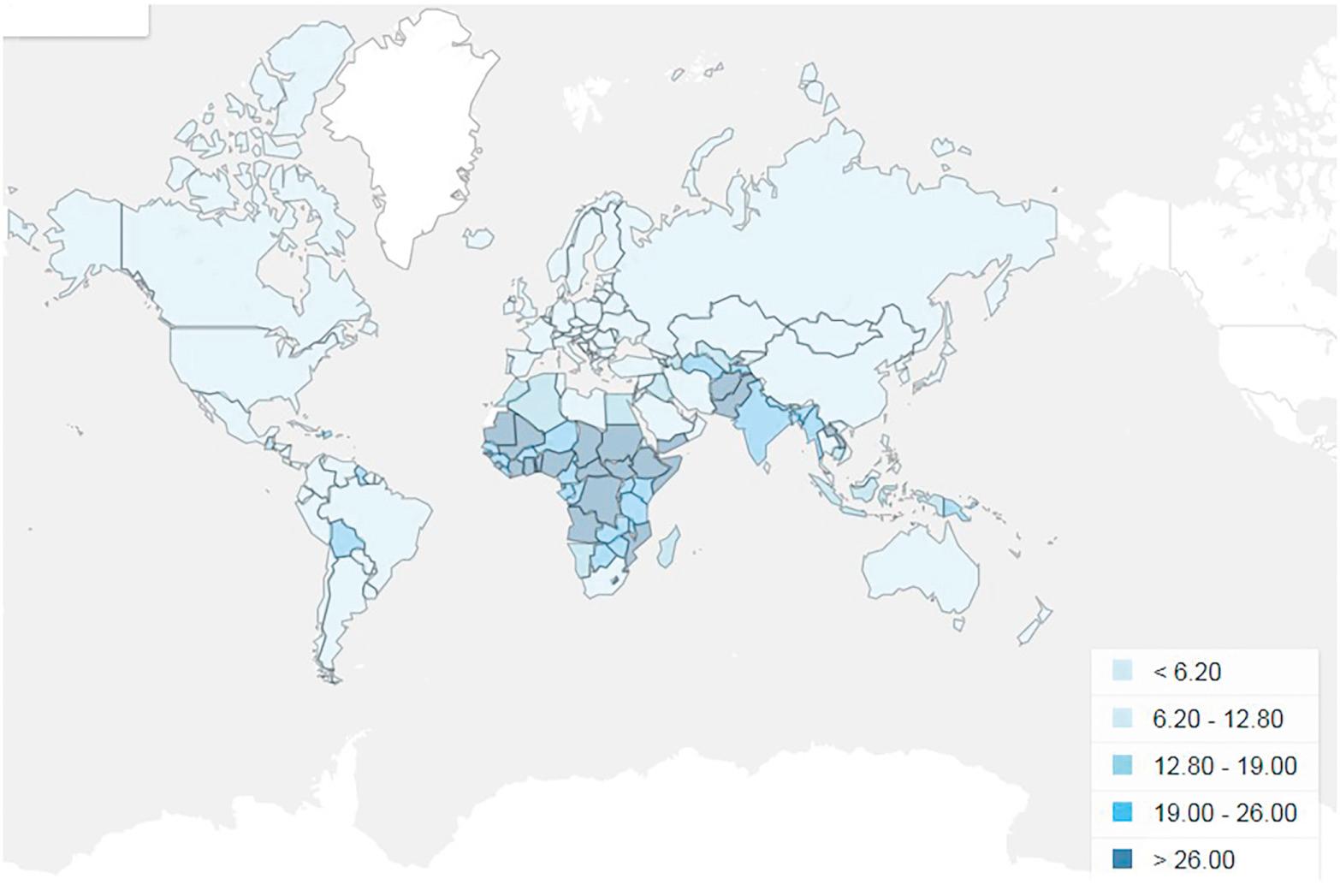
In an analysis of NMR, out of 193 countries from 1990 to 2009, the investigators found that only 38 countries had a system of civil registration of births and deaths. One hundred fifty-five other countries calculated NMR using statistical models. During the two-decade study, 79 million babies died. More than 98% of deaths occurred in LMICs, the majority of these deaths occur in South Asia and sub-Saharan Africa. The annual reduction rate of NMR was twice as high for the period 1999 to 2009 (2.3%) compared with the period 1990 to 1999 (1.1%). There was a lower rate of reduction of NMR in high-income countries (HICs) (1.7% in 1999 to 2009 vs. 3.7% in 1990 to 1999). In spite of these decreases in NMR across the LMICs, the annual rate of NMR reduction was still well below the MDG #4 goal of 4.4% and below the IMR and under-5 mortality rate reductions. Most importantly, NMR varies marginally between countries, with the highest neonatal mortality rates in sub-Saharan Africa and Southeast Asia ( Fig. 8.3 ).
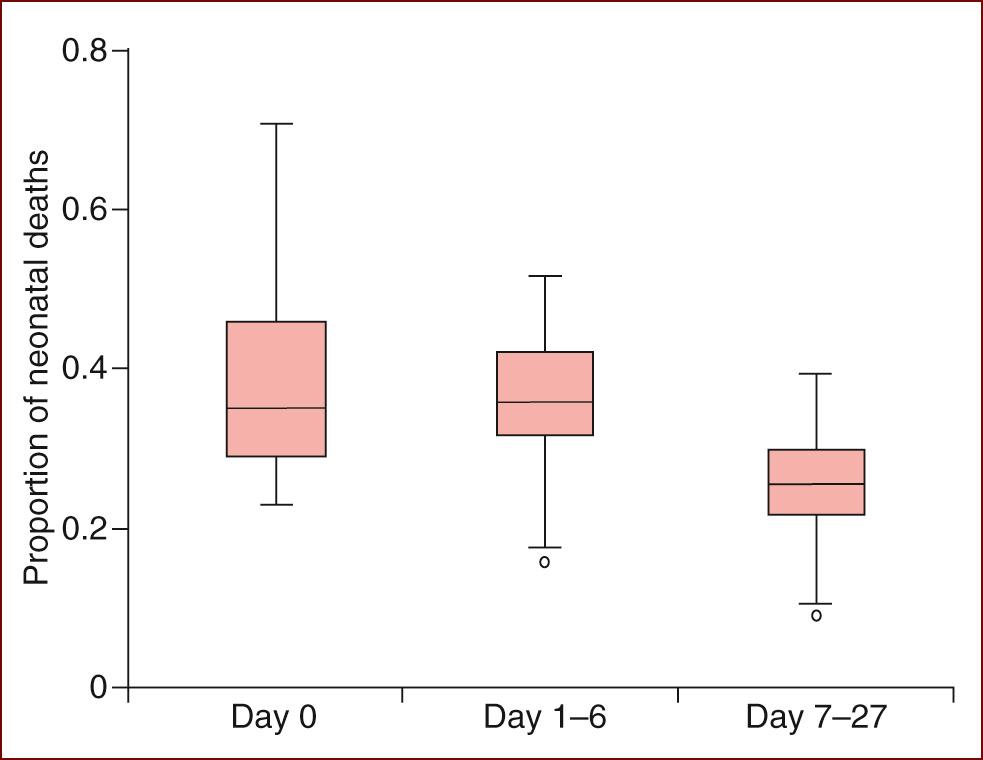
Of the 7.6 million deaths in children under 5 years in 2010, 40% were neonatal deaths ( Fig. 8.4 ). Preterm birth complications (14% of under-5 deaths), birth asphyxia (also called intrapartum-related) complications (9%), and sepsis/meningitis (5%) were the most frequent causes of death in the neonatal period. About 35% of the neonatal deaths occured on the day of birth with another ~35% occurring during the rest of the first week after birth ( Fig. 8.5 ). After a month of age, pneumonia (14%), diarrhea (10%), and malaria (7%) were the most frequent causes of death. To decrease under-5 mortality the most, efforts should concentrate on these causes of death, particularly soon after birth.
![Fig. 8.4, Global causes of childhood deaths in 2010. Causes that led to less than 1% of deaths are not shown. Of all infectious disorders, pneumonia, diarrhea, and malaria were the leading causes of death worldwide. Of all deaths in children younger than 5 years, pneumonia caused 1.396 million deaths (uncertainty range [UR] 1189–1.642 million; 18.3% of total deaths), diarrhea caused 0.801 million deaths (UR 0.555–1.182 million, 10.5%), and malaria caused 0.564 million deaths (UR 0.432–0.709 million, 7.4%). Fig. 8.4, Global causes of childhood deaths in 2010. Causes that led to less than 1% of deaths are not shown. Of all infectious disorders, pneumonia, diarrhea, and malaria were the leading causes of death worldwide. Of all deaths in children younger than 5 years, pneumonia caused 1.396 million deaths (uncertainty range [UR] 1189–1.642 million; 18.3% of total deaths), diarrhea caused 0.801 million deaths (UR 0.555–1.182 million, 10.5%), and malaria caused 0.564 million deaths (UR 0.432–0.709 million, 7.4%).](https://storage.googleapis.com/dl.dentistrykey.com/clinical/PerinatalandNeonatalCareinDevelopingCountries/3_3s20B9780323567114000080.jpg)
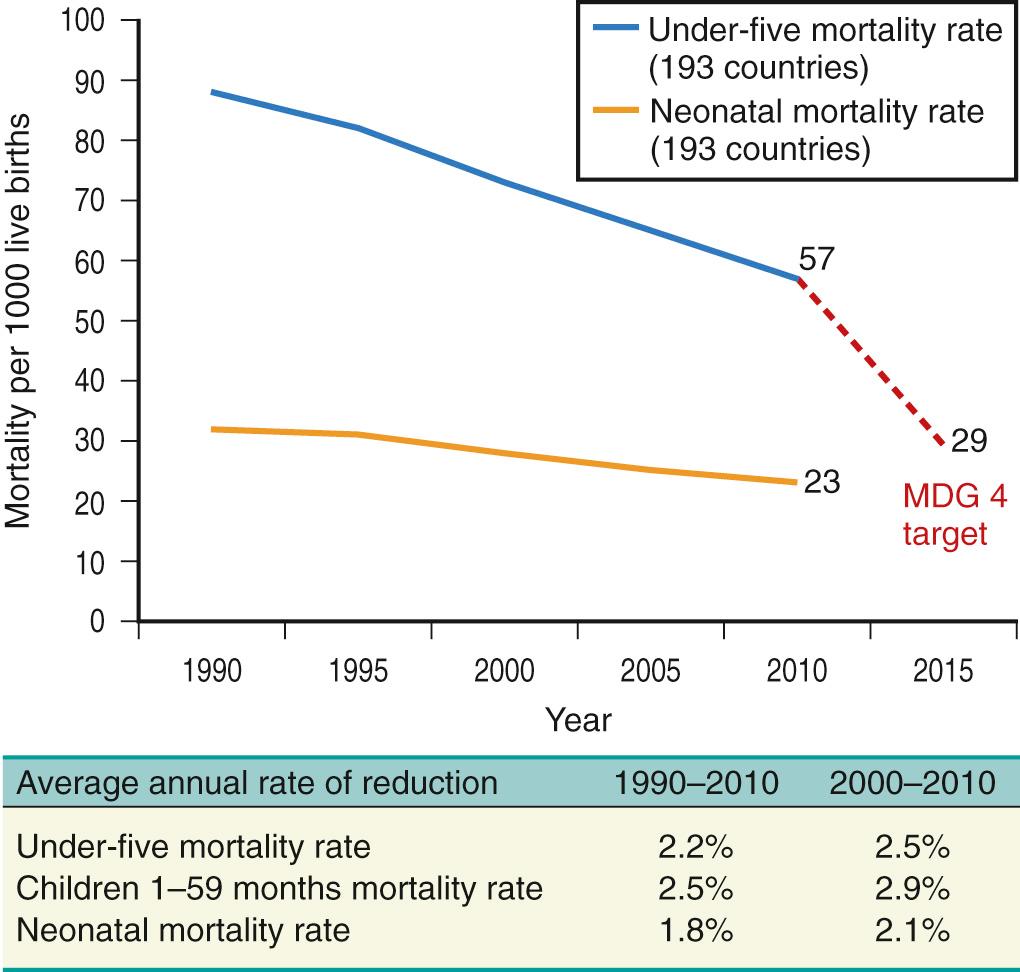
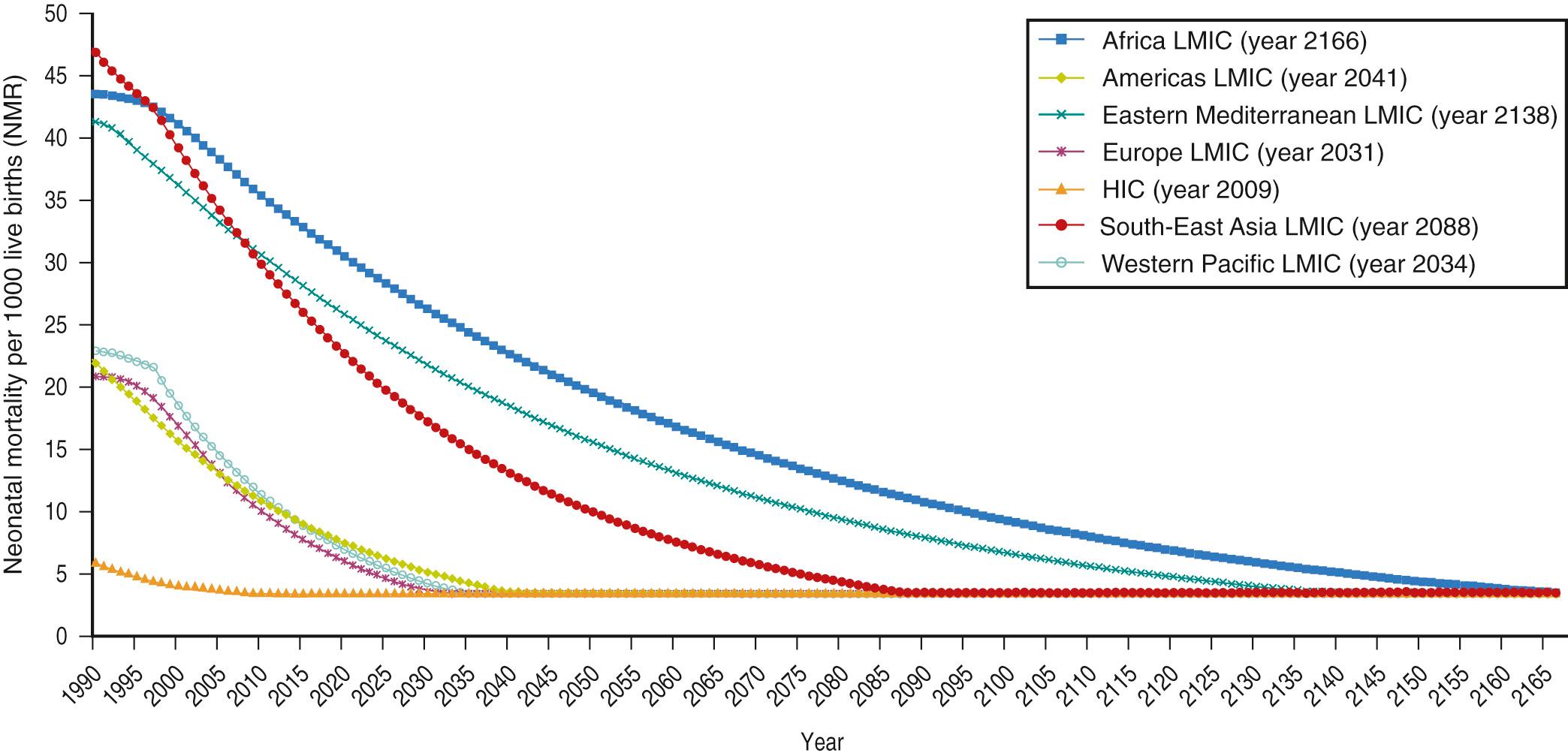
Compared with NMR, the under-5 mortality rate (U5MR) decreased considerably from 1990 to 2010. Fig. 8.6 shows trends in U5MR and NMR in 193 countries from 1990 to 2010. The U5MR showed a steady decrease during the period, whereas the NMR, although decreasing, did so at a slower rate. The NMR thus constituted a higher proportion of U5MR from 2000 to 2010 compared with 1990 to 2000. South Asia accounts for more than half of under-5 deaths. Almost 30% of global neonatal deaths occurred in India. Sub-Saharan Africa accounts for 38% of global neonatal deaths, with the highest NMR (34/1000 live births) and least progress in reducing that rate over the last two decades. Neonatal deaths in sub-Saharan Africa account for about one-third of U5MR (1.1 million neonatal deaths). Taking into consideration the current slow rate of reduction in NMR among the LMICs, the authors also calculated the number of years it will take various countries in different regions to achieve NMR levels similar to those currently in HIC ( Fig. 8.7 ). It is disconcerting to note that for some countries, it will take several decades to reach the low levels of HIC, whereas others may take more than 100 years to reach the low levels of HICs. These disappointing findings underscore the need for serious efforts with a stronger health policy to decrease NMR and IMR in sub-Saharan countries.
Factors that influence MMR and NMR include commonly known maternal and neonatal medical problems, socioeconomic conditions, gender inequality, environmental factors, and economic and political instability. Socioeconomic factors greatly influence the health of mother and baby, in particular, in LMICs, as discussed in the following section.
The socioeconomic factors adversely influencing IMR include gender bias against women, maternal education, and economic dependence. SDG #5 is aimed at eliminating gender inequity. Gender bias against women has a negative effect on every phase of a woman's life, interfering with her education, economic power, and health. Gender-biased discrimination begins its influence early in life, leading to poorer nutrition and health in girls compared with boys. Gender inequalities persist worldwide, depriving women and girls of their basic rights and opportunities. SDG #1 aims to end poverty in all its forms everywhere. SDG #4 aims to ensure inclusive and equitable quality education and promote lifelong learning opportunities for all. Evidence shows that a woman with more education has fewer children, better economic status, lower fertility rate, lower IMR, and improved quality of life. Even in developed countries, every additional year of education for women is associated with lower mortality rates at all ages. Education increases earning potential, and higher income is associated with lower mortality. Earning power provides women with economic, social, and political empowerment. In short, education is seen as a means of ensuring health. Health-seeking behavior during pregnancy, childbirth, and the neonatal period is influenced by regional, religious, and ethnic differences and by cultural beliefs. Understanding the cultural beliefs and their influences on care of the mother and infant is crucial to providing appropriate counseling to mothers. Health strategies to improve MMR and IMR in LMICs include implementation of programs that eliminate gender inequities, end poverty, and ensure equitable education will enable women to improve their health and that of their children. In addition, increasing awareness of maintaining health, improving health-seeking behavior, and improving access to health care will improve health outcomes.
Economic stability alone does not guarantee better health of the mother and child. For example, many oil- and mineral-rich countries in Middle East, Africa, and Latin America with a sizeable global income are a unique group with wide disparities of wealth and health. Despite high gross national product, some of these countries have high IMR, high U5MR, high MMR, and low life expectancy. Although the overall IMR has decreased from ~200 per 1000 in the 1950s to ~50 per 1000 in 2000, in some countries, IMRs are far higher than in Latin America and East Asia.
Women and children account for a disproportionate morbidity burden among conflict-affected populations. Political instability and wars have adversely affected perinatal and neonatal outcome. For example, infant mortality rate and under-5 mortality rate increased during the recent conflict in Syria. Similarly, natural disasters such as Hurricane Katrina and tsunamis call for preparedness to care for pregnant women, parturient mothers, and neonates. Pediatricians and neonatologists serving in areas of war conflicts and those working in the armed forces should be well-prepared to manage these situations.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here