Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Percutaneous therapies have changed how the modern cardiothoracic surgeon approaches the treatment of valvular heart disease. Although much of this evolution has come with the advent of transcatheter aortic valve replacement, considerable obstacles inherent to mitral valve disease have been overcome to develop multiple percutaneous technologies.
Surgery is often difficult because mitral valve disease is both caused by and develops in parallel to many comorbidities that increase surgical risk. This has been demonstrated by reports that as many as 50% of patients with severe mitral regurgitation (MR) are not candidates for surgery.
The challenge of developing effective percutaneous mitral valve repair technology stems from the complexity and variation of both the pathophysiology of mitral valve disease and the anatomy of the mitral valve apparatus.
Degenerative MR (DMR; ) develops when disease of the valve itself prevents sufficient mitral leaflet coaptation via leaflet or chordal elongation, chordal rupture, or annular deformation, whereas functional MR (FMR) develops when left ventricular dysfunction and deformation prevent sufficient coaptation of anatomically normal leaflets via annular dilation or leaflet tethering.
Patients with central, discrete regurgitant jets with relatively narrow bases and single-leaflet prolapse or flail may benefit from percutaneous edge-to-edge repair.
Patients with enlarged hearts, annular dilation, minimal tenting, and central jets may benefit from percutaneous annuloplasty. 3
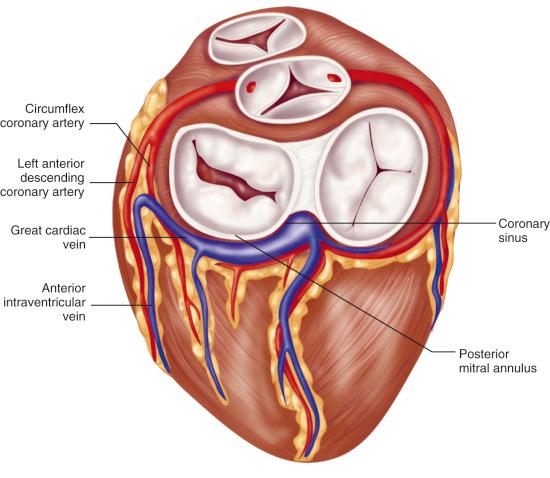
Successful coronary sinus–based annuloplasty is more easily achieved in patients with a large coronary sinus and a large great cardiac vein, with minimal tortuosity. Moreover, effective reduction of the septolateral diameter can only be achieved if the coronary sinus and great cardiac vein lie in the same plane as the mitral annulus ( Fig. 22.1 ).
The goal of any percutaneous procedure is to achieve a durable correction of mitral disease with clinical efficacy similar to that of well-established open surgical interventions. Most approaches to percutaneous mitral valve repair are modeled after established surgical techniques.
By applying concepts that have made surgical repair successful to the engineering of percutaneous technologies, restoring proper mitral valve function can be performed without the risks inherent to surgery.
Worldwide, mitral stenosis (MS) most commonly results from rheumatic valvular disease, typically with fusion of the leaflets at the commissures.
Balloon mitral valvuloplasty (BMV) splits the fused commissures, allowing the mitral valve to open more fully, and is the most well-established catheter-based repair of mitral disease since the 1990s.
The applicability and efficacy of BMV are limited, with optimal outcomes in patients with a mitral valve that is relatively thin and free of calcification, resulting in greater leaflet mobility when the fused commissures are divided and minimizing the risk of embolic complications.
BMV lacks utility when concomitant left atrial clot or more than mild to moderate MR is present. Once either of these is present, mitral valve surgery is preferred unless the patient is at prohibitive surgical risk.
BMV has limited efficacy in those with senile calcific MS because it is caused not by commissural fusion but by calcification that extends into the leaflets from their origination in the annulus.
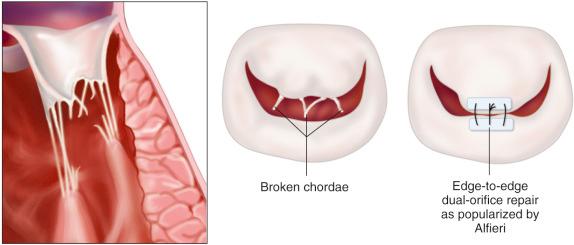
Although uncommonly used in conventional surgical repair of MR, the edge-to-edge repair, first described by Alfieri in 1991, has been shown to be effective at decreasing MR without significant risk of MS in selected patients. The MitraClip procedure (Abbott Laboratories, Abbott Park, IL) is a percutaneously delivered device that mimics the sutures placed in an Alfieri repair. Whereas the original Alfieri technique ( Fig. 22.2 ) combined an edge-to-edge suture with annuloplasty, the MitraClip procedure is currently performed in isolation without annuloplasty. Although debated, isolated reports have documented adequate outcomes with surgical edge-to-edge repair without annuloplasty, providing the basis for the use of the MitraClip procedure as a sole therapy.
Degenerative and functional MR often necessitate very different treatment approaches but, as an intervention that was hoped to offer benefit to patients with either cause, the MitraClip procedure was initially studied in a heterogeneous population. Surgical mitral repair has provided excellent outcomes for patients with DMR, but the benefit to patients with FMR is controversial. Although there exists a gold standard for treating FMR in nonsurgical patients, no such standard exists for treating DMR. Given the inferior efficacy when compared to surgical repair and the lack of a gold standard for nonsurgical patients with degenerative pathology, the US Food and Drug Administration (FDA) approved the MitraClip procedure in 2013 as an alternative treatment option for symptomatic patients with severe (≥ 3+) DMR at prohibitive surgical risk.
Currently, a functional cause of MR is not an approved indication for the MitraClip procedure. Severe FMR certainly worsens heart failure physiology and symptoms by contributing to volume overload and progressive dilation, but it is yet unclear whether correcting the MR actually improves survival. The EVEREST II (Endovascular Valve Edge to Edge Repair Study) trial has shown that FMR is a significant predictor of mortality on multivariable analysis (hazards ratio [HR], 2.7; confidence interval [CI], 1.4–5; p = 0.003), so although the repair of MR may improve symptoms, it may not address the causal pathophysiology or affect the clinical trajectory likely determined by the underlying left heart dysfunction. FMR is primarily treated via goal-directed medical therapy aimed at improving underlying left ventricular dysfunction with beta blockade, diuretic use, angiotensin-converting enzyme inhibitors and, if indications are found, cardiac resynchronization. It is therefore recommended to ensure that patients receive maximal medical therapy prior to considering mitral intervention.
Patients with DMR must meet many anatomic criteria to have the MitraClip device placed. Although reported to have caused only one case of MS after 5 years of follow-up in the clinical trial, there have been other reports of MS following MitraClip placement. As such, a resting effective orifice area over 4 cm 2 is required to minimize this long-term risk of MS.
Considering that the Alfieri technique can only address poor coaptation at one place along the valve orifice, multiple foci of MR preclude the use of the MitraClip. Ideally it should be used when a single primary regurgitant jet is present.
Although initial studies excluded patients with excessively calcified leaflet edges out of concern for capture failure, this has often been overcome in subsequent clinical experience with multiple clip placement, with reports of as many as 40% of patients receiving a second clip and some even receiving a third.
Surgical repair of MR is often accomplished by reducing the septolateral diameter of the mitral annulus, thereby increasing coaptation with the placement of a rigid, undersized annuloplasty ring. Several technologies have been developed to accomplish annuloplasty percutaneously and, because it can halt the progressive dilation of the mitral annulus often responsible for FMR, it may be of greater benefit than MitraClip placement for those with functional pathology. These therapies have been developed either to anchor a device to the annulus directly or indirectly reduce septolateral diameter with a device in close proximity to the annulus.
As the only available technology that indirectly reduces mitral annular diameter, the Carillon Mitral Contour System (Cardiac Dimensions, Kirkland, WA) takes advantage of the proximity of the coronary sinus to the mitral annulus.
Although the Carillion System obtained CE Mark approval in 2011 for commercial use in the European Union, it continues to be investigational in the United States with the first randomized controlled trial anticipated to begin enrollment in 2017. It is yet to be seen whether this technology will be able to overcome the challenges encountered in initial efficacy studies. Sufficient reduction in MR could not be achieved in many patients because anatomic variability led to device placement in a coronary sinus too far removed from the annulus or above the annular plane in the wall of the left atrium.
Furthermore, because as many as 80% of patients have been reported to have a coronary artery course between the coronary sinus and mitral annulus, the device had to be withdrawn in 16% of patients due to impingement of the left circumflex artery or its major branches.
Several technologies have emerged to anchor either an annuloplasty ring or plication sutures directly to the mitral annulus via transvenous, transseptal, or retrograde transaortic valve delivery systems.
Although the company that developed the only technology available for percutaneous placement of individual suture plication stitches has shifted focus to its application to tricuspid disease, the various technologies that accomplish more complete annuloplasty are in the early stages of development, and the patient populations that will most likely benefit from each have yet to be identified.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here