Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Although one-third of SWs to the anterior abdomen do not penetrate the peritoneum, 80% of GSWs violate the peritoneum. Additionally, of those wounds that penetrate the peritoneum, 95% of GSWs have associated visceral or vascular injuries, while only one-third of SWs do ( Fig. 25.1 ).
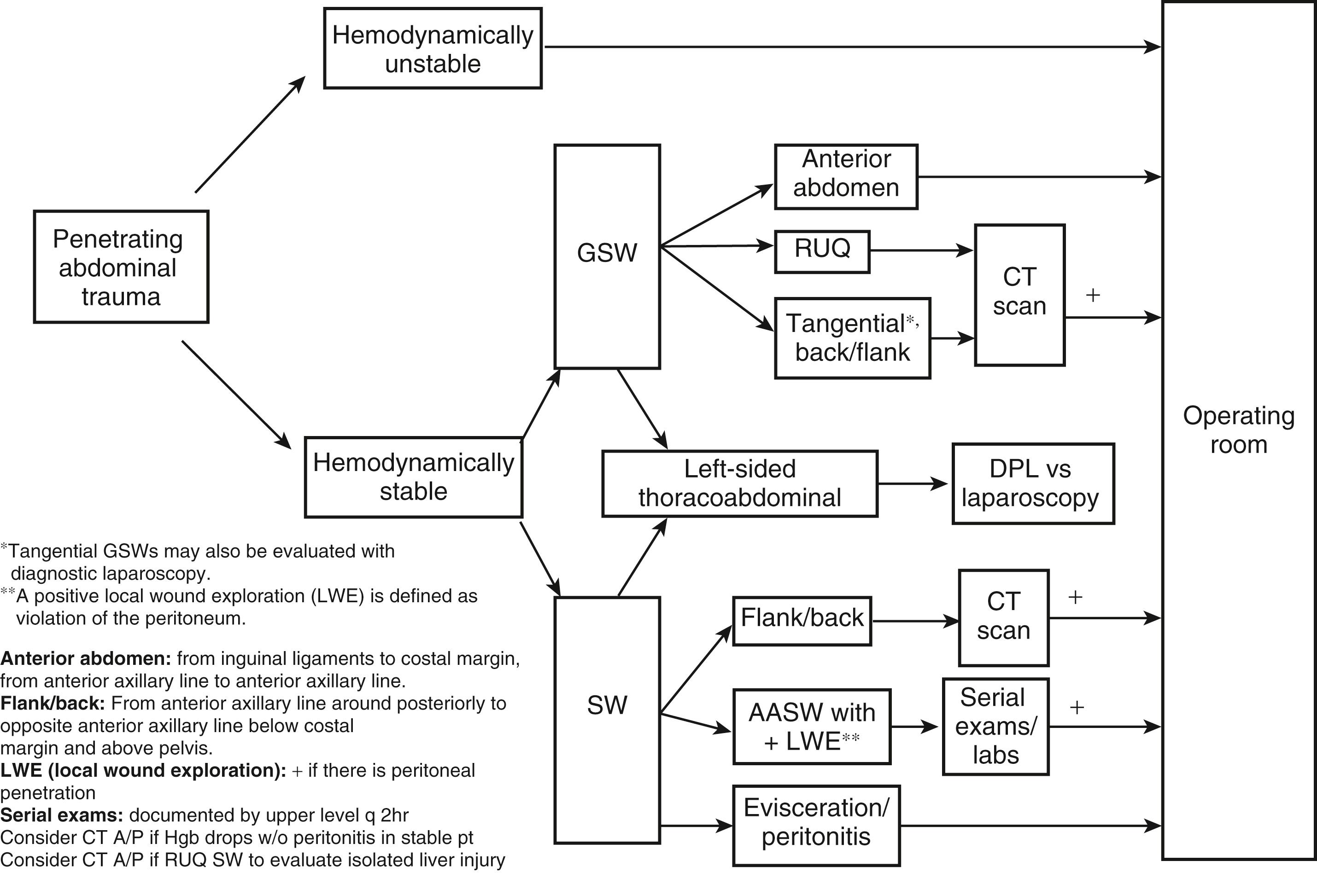
Hypotension, peritonitis, other signs of abdominal visceral injury (hematemesis, proctorrhagia, palpation of diaphragmatic defect on chest tube insertion, and radiologic evidence of injury to the gastrointestinal [GI] tract) mandate immediate exploration. Most authorities also advocated prompt exploration for omental or intestinal evisceration because of the high risk of visceral injury.
Because of the high incidence of visceral injury, early exploration is indicated for virtually all GSWs that violate the peritoneum. The exception is penetrating trauma isolated to the right upper quadrant; in hemodynamically stable patients with bullet trajectory confined to the liver by computed tomography (CT) scan, nonoperative observation may be considered. Similarly, in obese patients, if the GSW is thought to be tangential through the subcutaneous tissues, CT scan can delineate the tract and exclude peritoneal violation. Laparoscopy is another option to assess peritoneal penetration.
Resuscitative thoracotomy should be considered when a patient presents in cardiac arrest (cardiopulmonary resuscitation <15 minutes) or with profound hypotension (systolic blood pressure [SBP] <60 mm Hg) that is refractory to initial resuscitation. Although external wounds may point to penetrating abdominal injury, intrathoracic structures may be injured as well. Therefore, following anterolateral thoracotomy, the heart should be assessed for injury; if cardiac tamponade is present, the pericardium is opened vertically in a plane anterior to the phrenic nerve. If an injury is identified, hemorrhage from the injury is controlled. Once the cardiac injury is controlled, or if no injury is identified, the descending aorta is cross-clamped to decrease subdiaphragmatic hemorrhage and improve coronary and cerebral perfusion. Open cardiac massage is performed if necessary. If these measures restore circulatory perfusion to a SBP >70 mm Hg, the patient is transferred to the operating room for definitive repair.
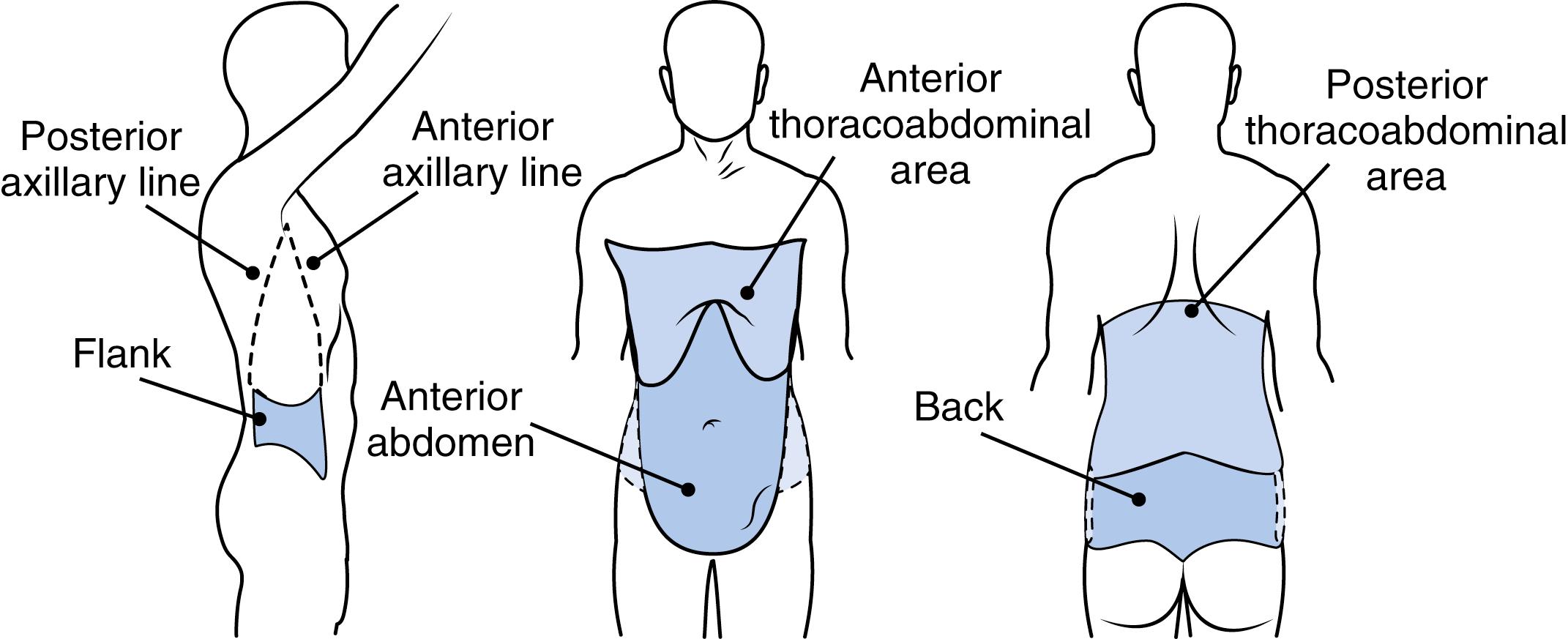
Examine the patient systematically; it is easy to overlook synchronous injuries. The examination includes looking for additional sites of penetrating wounds; be sure to look thoroughly in the axilla and perineum as wounds can be hidden in folds of skin. Evaluation for blood in the GI, genitourinary, and gynecologic systems should be done, and associated blunt mechanisms of injury should be considered; some patients are assaulted with both knives and fists ( Fig. 25.2 ). A neurologic exam is important to document any deficits prior to operative intervention as well as to determine the etiology.
A chest radiograph ensures that the bullet did not traverse the diaphragm causing a hemothorax or pneumothorax; the chest film also determines the position of any new tubes or lines (e.g., central venous catheters endotracheal tubes, nasogastric tubes, and thoracostomy tubes). Biplanar abdominal radiographs are helpful in locating retained foreign bodies (i.e., bullets) and may reveal pneumoperitoneum. In penetrating abdominal trauma from GSWs, it is important to obtain a plain radiograph of the abdomen plus films one space above and below the site of injury; this helps locate retained missiles and gain information regarding the trajectory of the bullet. A general idea of trajectory is helpful to direct abdominal exploration at the time of laparotomy. For example, a single wound at the umbilicus with an abdominal film demonstrating a bullet in the pelvis would heighten one’s concern for an iliac or rectal injury versus identifying a bullet in the right upper quadrant. Determining trajectory utilizing plain films to identify retained bullets is especially important when only one wound is evident. Radiopaque markers applied to the skin at the site of evident wounds are also helpful in determining the trajectory of missiles. Injuries in proximity to the rectum obligate sigmoidoscopy (see Chapter 29 ), and those with proximity to the urinary tract should be evaluated with CT scanning (see Chapter 31, Chapter 32 ).
Focused abdominal sonography for trauma (FAST) exams are performed to assess for hemoperitoneum and may be an adjunct in the initial evaluation of the patient sustaining penetrating trauma. FAST includes examining four locations: the right supra-renal recess (Morrison’s pouch), the pelvis around the bladder, the splenorenal fossa, and the pericardium. The extended FAST (eFAST) includes examining the pleura for normal lung slide, which if absent indicates a pneumothorax. All of this imaging is performed in the ED resuscitation bay. Only hemodynamically stable patients should undergo CT scanning. Of note, FAST may be unreliable in anterior abdominal SWs. FAST may not reveal fluid if less 250 cc is not present. Initial labs should include a spun hemoglobin, complete blood count, basic metabolic panel, lactate, arterial blood gases, and coagulation studies (ideally thromboelastography or rotational thromboelastography). These studies guide transfusion and resuscitation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here