Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The development and maturation of the elbow is complex in children. Many cartilaginous structures are incompletely ossified until late in skeletal development and are weaker in tensile strength in comparison to the surrounding ligamentous and muscular attachments. Thus, isolated elbow dislocations are uncommon in children, accounting for approximately 3% to 6% of all elbow injuries in children. Up until 2 years of age, any malalignment of the elbow joint should be suspected to be a transphyseal fracture separation of the distal humeral physis. After 2 years of age, the incidence in elbow dislocations increases until a peak is noted at 12 years of age. Then the gradual ossification of the coronoid and olecranon, along with the corresponding decrease in ligamentous laxity noted in later development, decreases the incidence of dislocations in older children. Boys are more likely to experience an elbow dislocation, and the nondominant extremity is more frequently affected. Associated fractures are extremely common in pediatric elbow dislocations and warrant additional scrutiny and occasionally advanced imaging.
The purpose of this chapter is to describe the etiology, diagnosis, and management of elbow dislocations and their associated fractures in pediatric patients. The pediatric elbow is a complex joint, and readers should familiarize themselves with the chapter on anatomy and imaging ( Chapter 25 ) as well as chapters dealing with associated elbow injuries ( Chapter 26, Chapter 27, Chapter 28, Chapter 29, Chapter 30, Chapter 31, Chapter 33, Chapter 34 ).
As noted previously, the skeletal components of the elbow joint ossify in a predictable pattern, although the majority of the distal humerus, predominantly the trochlear and medial condyle, does not begin ossification until 6 years of age. The distal humeral epiphysis consists of four separate ossification centers, which in order of appearance are the capitellum (1–2 years of age), the medial epicondyle and trochlea (4–6 years of age), and the lateral epicondyle (9.5–11.5 years of age). The radius and ulna each contributes a single ossification center, at the radial head epiphysis (2–4 years of age) and the olecranon apophysis (9–11 years of age). In many cases, the olecranon and trochlea may have multiple small ossific nuclei that merge together with maturation. This is a normal variant in development that should not be misinterpreted as a fracture. Overall, the appearance of ossification centers occurs 1 to 2 years earlier in females than in males. This principal also applies to the fusion of ossification centers and closure of the physes around the elbow, where females precede males by 2 to 3 years. The trochlea, lateral epicondyle, and capitellum fuse around 11 years of age in girls and 12 to 13 years of age in boys, followed by the radial head and olecranon at 12 to 13 years of age in girls and 14 to 15 years of age in boys. Lastly, the medial epicondyle fuses to the distal humerus at 13 to 14 years of age in girls and 15 to 16 in boys. When an elbow is dislocated, the physician should always search for the medial epicondyle in age-appropriate children, as it is frequently avulsed and can be entrapped in the elbow joint. This injury necessitates extraction of the incarcerated fragment from the joint. The lateral epicondyle has been noted to be entrapped in the elbow joint as well, although this injury is rare and much more difficult to assess given the late ossification of this structure.
Knowing the predictable pattern of ossification about the elbows allows the physician to interpret radiographs based on patient age. The evaluation of the elbow should include evaluation of a line drawn down the neck of the radius on the anteroposterior (AP) and lateral radiographs to evaluate the radiocapitellar line. Due to irregularity of the ossific nuclei, the standard radiocapitellar line (RCL) may not always intersect with the capitellum in young children. However, this fact should not preclude the use of the RCL when evaluating the pediatric elbow, as an RCL anterior or medial to the capitellum would indicate radial head subluxation or dislocation in these patients ( Fig. 32.1 ). In cases where radiographs are unclear, advanced imaging modalities, such as ultrasound, arthrography, and magnetic resonance imaging (MRI), can be used to help establish a diagnosis.

Due to the ossification pattern of the pediatric elbow, much of the elbow joint is cartilaginous during early adolescence. This imparts flexibility to the elbow joint despite being one of the most congruent joints in the body. As such, 10 to 15 degrees of elbow hyperextension is commonly noted in young children. The main stabilizing ligaments of the elbow, the medial ulnar collateral ligament (MUCL) and the lateral ulnar collateral ligament (LUCL), are attached to the medial and lateral epicondyle apophyses, respectively. These apophyses are structurally weak and prone to avulsion injury, which can lead to increased risks of articular incongruity following injury.
The coronoid and olecranon processes of the ulna also do not fully ossify until late in adolescence. When fully ossified, these structures provide stability to the elbow, especially with the coronoid process protecting against posteriorly directed forces that most frequently result in elbow dislocations. The cartilaginous coronoid and olecranon processes additionally hamper the ability of the elbow joint to “lock in” place during terminal flexion and extension.
The radiocapitellar joint is also predisposed to laxity due to the cartilaginous volume of the radial head and capitellum, as well as the stability of this joint that is provided by the annular ligament. A nursemaid's elbow, commonly seen in children under 6 years of age, presents as the radial head is pulled out of the annular ligament, which subsequently gets trapped in the radiocapitellar joint or, less commonly, torn. A simple reduction maneuver with forearm supination and elbow flexion can replace the annular ligament around the radial head, typically noted with immediate relief of pain. Radiocapitellar laxity may additionally allow for dislocation of the radial head either by itself or in conjunction with an ulnar fracture, commonly referred to as a Monteggia fracture (see Chapter 31 ).
The complex ossification of the cartilaginous structures of the elbow, combined with the inherent ligamentous laxity seen in children, predisposes the elbow joint to subluxate and ultimately dislocate given the appropriate traumatic forces.
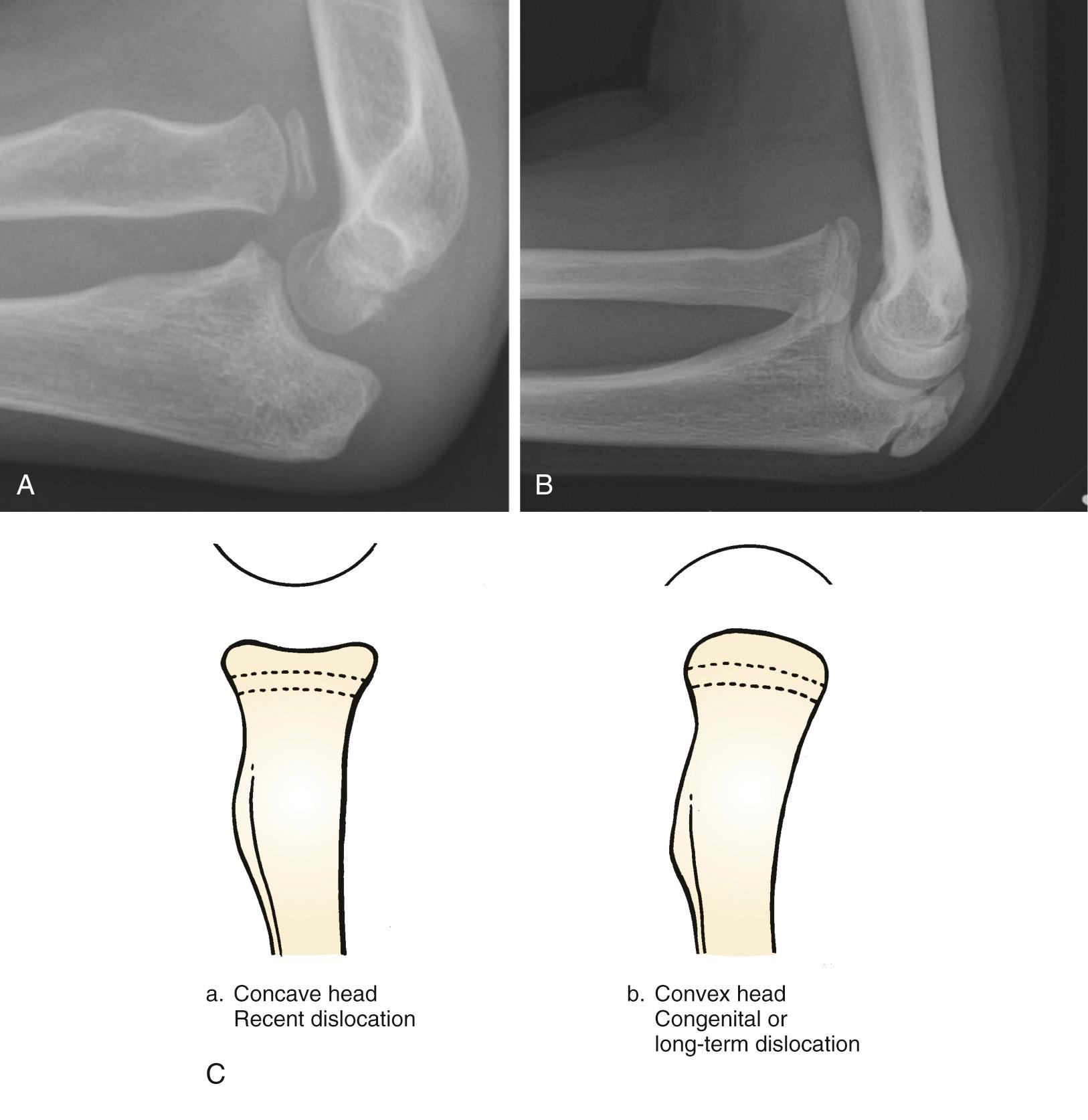
A congenital dislocation of the radial head implies that the radiocapitellar joint formation was altered during embryologic formation of the elbow joint. This process is fundamentally different from a developmental radial head dislocation where abnormal forces in the forearm can lead to progressive radial head subluxation and, ultimately, dislocation from the capitellum. While the end result of both forms of dislocations is an elongated radial neck, convex radial head, and dysplastic capitellum, knowing the underlying mechanism is important to guide appropriate treatment.
A congenital radial head dislocation should be diagnosed only when other congenital abnormalities are present ( Fig. 32.2A,B ). Failure to find evidence of other malformations is indicative of an isolated radial head dislocation, which is more likely developmental or posttraumatic in nature. Additional congenital malformations that are found with congenital radial head dislocation include a hypoplastic capitellum (see Fig. 32.2C ), increased ulnar length relative to the radius, proximal radioulnar synostosis, and transverse forearm deficiency. Posterior dislocation is found in 40% of congenital dislocations and is also associated with increased posterior bowing of the ulna, similar to what is found in a chronic posterior Monteggia fracture.

Radial head dislocation that is not associated with additional congenital findings typically develops over time due to altered mechanical forces about the forearm and elbow. Any entity that leads to asymmetric growth of the radius and ulna can lead to progressive subluxation and dislocation. This phenomenon is commonly seen in multiple hereditary exostosis (MHE), where up to one in seven individuals can have a progressive radial head dislocation. Exostoses of the distal ulna retard growth of the distal ulnar physis, leading to progressively increasing radial length and dislocation. Radial head dislocation is also seen in Madelung deformity, where dysplasia of the volar/ulnar physis of the radius can tether growth of the distal radius, leading to increased bowing of the radial shaft and dislocation of the radial head. Radial head dislocation has additionally been described in patients with Klinefelter syndrome, Cornelia de Lange syndrome, nail-patella syndrome, Ehlers-Danlos syndrome, Nievergelt syndrome, Silver syndrome, Apert syndrome, arthrogryposis, and cleido-cranial dysostosis.
Spasticity or weakness of elbow musculature has also been associated with radial head dislocation. In brachial plexus birth palsy, denervated muscle does not grow as effectively as the skeleton, leading to contractures of the elbow flexors and subsequent progressive radial head dislocation. This phenomenon has been noted in up to 6% of all patients with a neonatal brachial plexus injury. Similarly, in cerebral palsy, centrally mediated spasticity of the elbow flexors can lead to progressive radiocapitellar joint subluxation and dislocation. Posttraumatic growth asymmetry of the forearm and malunion of the radial neck have also been implicated in developmental radial head dislocations.
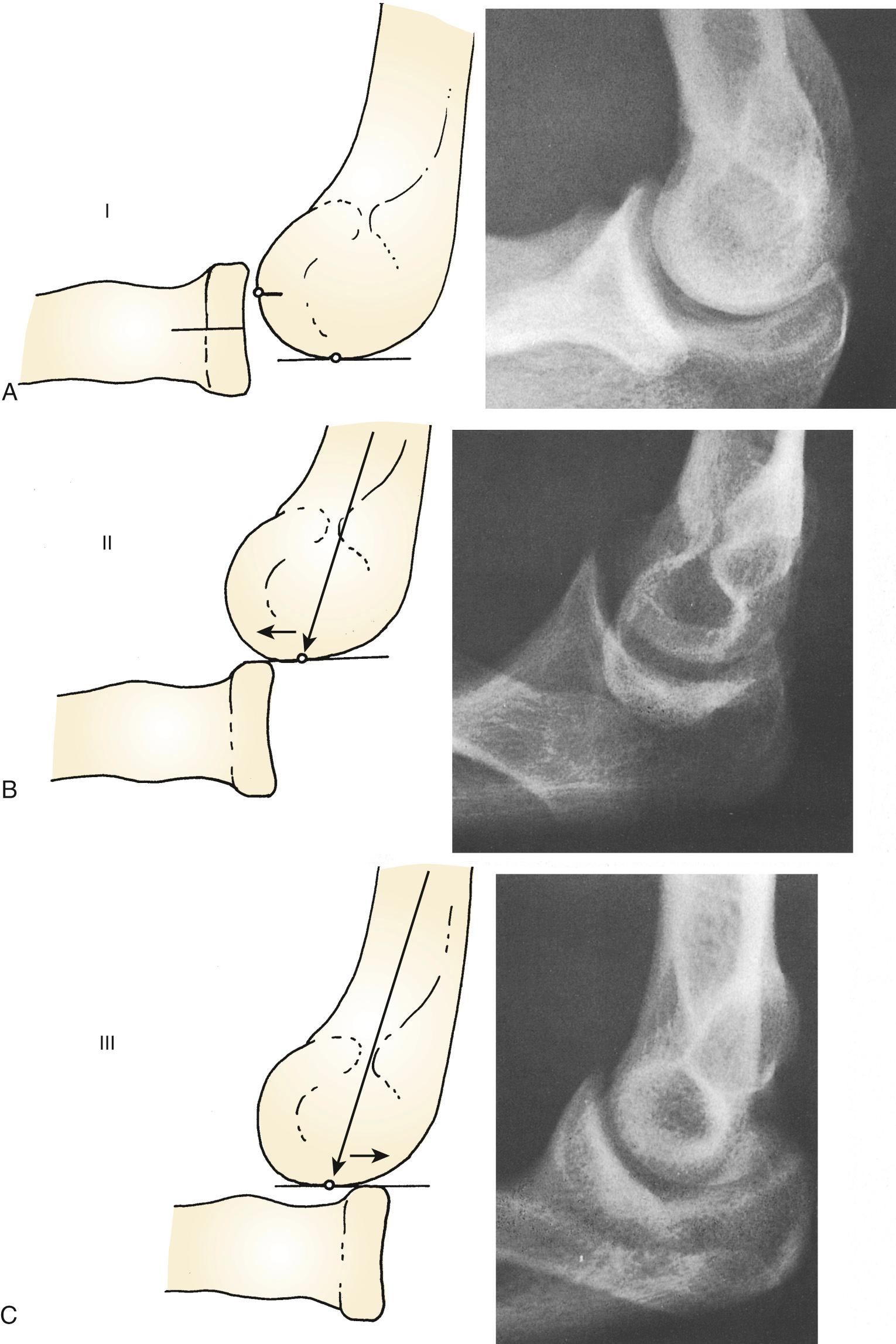
Posterior radial head dislocations are categorized by the degree of displacement using the Mayo classification ( Fig. 32.3 ). Type I is characterized by mild to moderate posterior subluxation of the radial head and can lead to limitations in range of motion (ROM) and considerable pain. Type II dislocations are displaced outside the capitellum without relative lengthening of the radius, which is seen in type III dislocations.
Congenital and developmental radial head dislocations share common radiographic features of dysplasia. Once the radial head dislocates from the capitellum, the radial head loses the contact pressures that help it maintain its concave shape. Over time the radial head epiphysis develops a rounded, convex shape, which would no longer articulate in the capitellum if reduction were attempted ( Fig. 32.4A–C ). For posterior dislocations, the lack of contact forces across the radial head epiphysis lead to lengthening of the radius via the Heuter-Volkmann principle. Often the radial neck will articulate with the inferior capitellum, leading to thinning of the radial neck. Additionally, the posterior bow of the ulna will be accentuated in long-standing posterior dislocation.
In anterior dislocations, the radial head will also develop a convex shape, and the radial shaft may straighten out of the normal dorsoradial bow, but overgrowth is limited by the pressure of the radial head abutting the anterior humerus during flexion of the elbow joint. Long-standing dislocations may also present with ulnar positive variance at the wrist due to the lack of a capitellar buttress to maintain forearm alignment with loading at the wrist.
Isolated, acute radiocapitellar dislocations are rare in children. As such, developmental dislocations are frequently misdiagnosed as acute injuries following minor arm trauma. In these cases, radiographs demonstrate a radiocapitellar dislocation, and care must be taken to evaluate the radiographs for the features of a developmental dislocation noted previously. In acute traumatic dislocations, the radial head dislocation will be accompanied by significant soft tissue swelling. Additionally, the elbow and forearm should be carefully evaluated clinically and radiographically for an associated ulnar fracture, which can be a subtle plastic deformation injury or occult fracture.
In anterior dislocations, the patient will likely demonstrate disuse of the arm and significant pain with attempted active or passive motion of elbow flexion/extension and pronation and supination. Once the initial pain and swelling have subsided, patients may present with limited elbow flexion due to the bony block of the radius on the anterior humerus but may have nearly normal pronation and supination. Long-standing anterior dislocations can be clinically silent in children, with minimal symptoms and near normal ROM. Over time, patients may develop excessive valgus and tardy ulnar nerve palsy in addition to limited range of elbow motion. In posterior or lateral dislocations, the radial head will be prominent posterolaterally, even in the setting of significant soft tissue swelling.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here