Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cardiac transplantation is an accepted therapeutic option which provides long-term survival for many patients with end-stage heart failure. Over 140,000 heart transplants at over 400 centers worldwide were recorded by the International Society for Heart and Lung Transplantation (ISHLT) Registry between 1982 and 2017; approximately 4000 per year are presently done worldwide . The success of cardiac transplantation has been attributed to refinement in candidate selection, use of the endomyocardial biopsy (EMB) to monitor cardiac allograft rejection, and improved immunosuppressive therapies. Actuarial survival is approximately 80% at 1 year and almost 70% at 5 years. The median survival is 13 years for transplant patients surviving past the first year.
The median age of heart transplant recipients has increased from 40 years in 1982 to 55 years in the last two decades because of increasing proportion of recipients greater than 60 years of age. This trend can be attributed to comparable survival rates between younger and older recipients. Moreover, hearts from older donors that would otherwise not be used for younger patients have been allocated to patients 70 years and older as an alternate cardiac transplantation strategy.
Relative contraindications for heart transplantation include pulmonary artery hypertension and high pulmonary vascular resistance, active infection (unless associated with left ventricular assist device; VAD), preexisting neoplasms (generally must be malignancy-free for at least 5 years to be eligible), body mass index >35 kg/m 2 , diabetes mellitus with end-organ damage, irreversible renal dysfunction, severe peripheral vascular or symptomatic cerebrovascular disease, active tobacco smoking or substance abuse, frailty, severe psychiatric or cognitive impairment, noncompliance with medications, and lack of family or social support .
Donor hearts are procured from individuals with brain death and intact circulation. Brain deaths are usually the result of blunt injuries sustained in motor vehicle accidents, penetrating head injuries such as gunshot wounds, or primary central nervous system events. The decision to use higher risk donor hearts from patients aged 50 years and older, patients with history of cocaine or alcohol abuse or dying from severe infection, sepsis or poisoning must be weighed against the individual’s risk of dying while on the waiting list. Conditions in the donor which may serve as absolute or relative contraindications for organ procurement include intractable arrhythmias, excessive need for inotropic support, echocardiographic evidence of wall motion abnormalities, left ventricular wall hypertrophy of 14 mm or more, obstructive coronary artery disease, and the presence of transmissible infectious disease including human immunodeficiency virus (HIV) and hepatitis B. The use of antivirals for hepatitis C has expanded the pool of heart donors with excellent outcomes The time from donor heart procurement until reestablishment of circulation in the recipient (ischemic time) ideally should be less than 4 hours , but slightly longer ischemic times are becoming more acceptable with younger recipients and donors . A donor heart with impaired cardiac function on significant inotropic support or one from an older donor with left ventricular hypertrophy is likely to be adversely affected by prolonged ischemic time.
The heart allocation policy in the United States follows a multitiered algorithm developed by the Organ Procurement and Transplantation Network that prioritizes patients depending on medical urgency, waiting time, blood group compatibility, and geographic location . Heart donors and recipients are matched for ABO blood group compatibility and body size. A panel-reactive antibody testing is performed to screen for humoral sensitization and to assess the risk of a positive crossmatch. Prospective human leukocyte antigen (HLA) matching is not routinely performed for logistical reasons, but retrospective tissue typing is useful for evaluation of donor-specific antibodies (DSA).
Heart transplantation may be orthotopic in which the recipient’s heart is removed and replaced by a donor organ or heterotopic in which a donor heart is added in parallel circuit with the recipient’s heart. The orthotopic technique is the one employed by virtually all transplant centers and is described in detail below . The heterotopic technique has very limited indications, primarily irreversibly high pulmonary vascular resistance in the recipient .
The potential donor heart is carefully examined in situ by the surgeon for appropriate size match and any evidence of traumatic injury, coronary artery disease, valvular heart disease, or congenital anomaly. The heart is perfused with a cardioplegic solution to achieve electromechanical arrest and is removed by transecting the superior and inferior venae cavae, pulmonary artery, aorta, and pulmonary veins. The organ is further cooled in cold saline and placed in an air-tight sterile container for transport. Clinical trials on the use of portable perfusion devices during transport are ongoing, and the pathology of human donor hearts preserved in this fashion has not been studied.
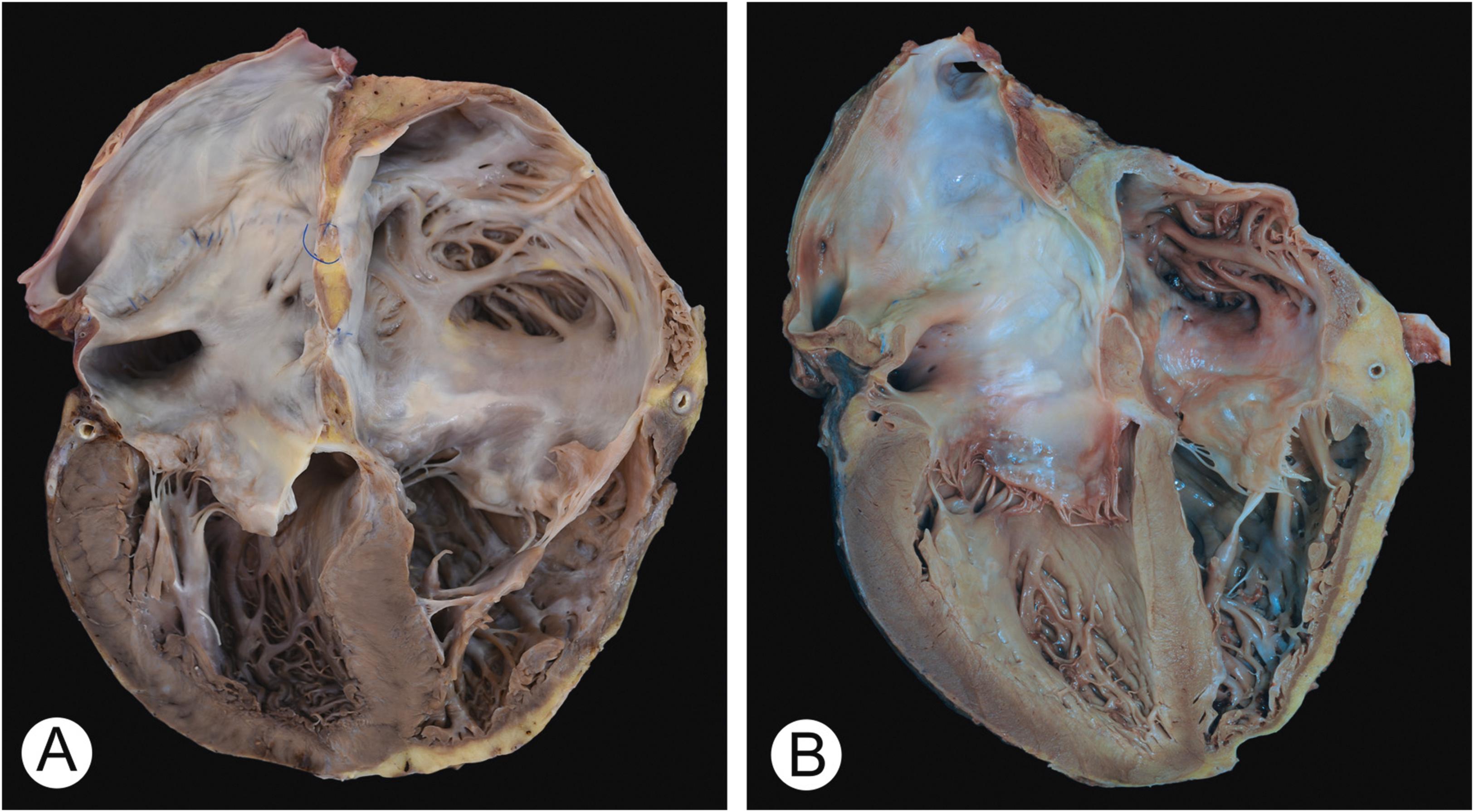
Following receipt of the donor heart in the operating room where the recipient has been prepared, including institution of cardiopulmonary bypass, the recipient’s diseased heart is removed by incising the right atrium and atrial septum so that the coronary sinus remains with the explanted heart. The aorta and main pulmonary artery are divided distal to their respective semilunar valves. The left atrium is then incised, making sure that its atrial appendage is excised and an adequate cuff of atrial tissue remains anterior to the pulmonary veins for suturing. Traditionally, the respective left and right donor and recipient atrial cuffs are sewn to produce a biatrial anastomosis, followed by anastomosis of the pulmonary artery and aorta ( Fig. 20.1A ). Potential complications of this biatrial technique include sinus node dysfunction, valvular insufficiency, and thrombus formation. A modified procedure, the bicaval technique ( Fig. 20.1B ) employs standard left atrial and separate bicaval anastomoses which maintains an intact right atrial anatomy . This latter method is increasingly being used, although it is technically more difficult and results in a slightly longer ischemic time. It is associated with improved early postoperative hemodynamics and lower incidence of atrial tachyarrhythmias and tricuspid regurgitation but does not appear to offer a better long-term outcome .
The contribution of pathology to the success of cardiac transplantation is well-established. The most visible role is that of the pathologist who interprets posttransplantation EMBs. The diagnosis and grading of acute rejection and assessment of numerous other biopsy findings are important in guiding the clinical management of recipients. Close collaboration between the pathologist and transplant clinician is essential for the optimal care of these patients. The pathologist also makes important contributions in the evaluation of the recipient’s native heart biopsy as part of the etiologic determination of cardiac failure, the examination of explanted recipient hearts, and the evaluation of a failed allograft. Moreover, the pathologist has the opportunity and, indeed, is in a rather unique position to add to existing knowledge of the pathobiology of heart failure and transplantation.
The two most common causes of end-stage heart failure leading to transplantation are cardiomyopathy and ischemic heart disease in the adult and cardiomyopathy and congenital heart disease in the pediatric age group ( Table 20.1 ) . Less common indications for transplantation include valvular heart disease, retransplantation, and miscellaneous other conditions. Pathological examination of the explanted hearts has a role in confirming the clinical diagnosis of the etiology of heart failure and, in some cases, yielding a more accurate diagnosis . The presence of previously undiagnosed conditions or unexpected findings are not infrequent and may affect the subsequent management and prognosis of the recipient.
| Age (in years) a | ||||||||
|---|---|---|---|---|---|---|---|---|
| < 1 | 1–5 | 6–10 | 11–17 | 18–39 | 40–59 | 60–69 | 70+ | |
| Cardiomyopathy (%) | 41 | 54 | 59 | 66 | 74 | 56 | 41 | 37 |
| Coronary artery disease (%) | 0 | 0 | 0 | 0 | 7 | 37 | 53 | 58 |
| Congenital heart disease (%) | 55 | 40 | 32 | 23 | 10 | 2 | 1 | 0 |
| Retransplantation (%) | 0.3 | 3 | 7 | 9 | 5 | 3 | 2 | 3 |
| Valvular heart disease (%) | 0 | 0 | 0 | 0 | 2 | 3 | 3 | 2 |
| Other (%) | 3 | 2 | 2 | 2 | 1 | 1 | 0 | 1 |
a Data from January 2006 through June 2013 as reported to the International Society for Heart and Lung Transplantation.
Eosinophilic, or hypersensitivity, myocarditis has been reported in up to 22% of explanted hearts from patients undergoing cardiac transplantation . It is usually considered an incidental finding and not related to any form of underlying pathology. Eosinophilic myocarditis has been related to one or more of the many drugs used to treat heart failure including digoxin, furosemide, and dobutamine infusion. The eosinophil-rich mixed inflammatory infiltrate is generally present in a focal or multifocal distribution and is confined to the interstitial and perivascular spaces with little or no associated myocyte necrosis . Epithelioid granulomas can sometimes be observed. Multinucleated giant cells are rare. Peripheral eosinophilia is often present but is not a consistent finding. Recurrence of eosinophilic myocarditis after heart transplantation has not been observed, and there is no apparent adverse effect on patient survival .
A number of case reports have documented diseases and pretransplant complications which recurred in an allograft ( Table 20.2 ) . An EMB of the recipient’s native heart prior to transplantation may help document such conditions. Clinicians should be made aware of the presence of any of these findings in the explanted heart, since their recurrence after transplantation, often discovered on routine surveillance EMB, may produce allograft dysfunction. Of the myocarditides, giant cell myocarditis and sarcoidosis have been reported to recur in the allograft , thus recipients are usually maintained on low-dose corticosteroids for immunosuppression. On the other hand, a retrospective multicenter analysis of 12 patients with active lymphocytic myocarditis in their explanted hearts suggested that those with active myocarditis rejected their transplanted heart early, at higher frequency, and with increased severity compared to heart transplant recipients with other preoperative diagnoses . Patients with amyloid heart disease undergo extensive evaluation before cardiac transplantation to establish the amyloid type and to rule out extracardiac involvement. These patients may require autologous stem cell transplantation or orthotopic liver transplantation, depending on the amyloid typing. Recurrent amyloidosis in the allograft is usually due to light chain deposition and rarely due to hereditary amyloidosis . An increased risk of thrombotic complications was found in heart transplant patients with prothrombin G20210A single nucleotide polymorphism . Vascular complications of aortic dissection and pseudoaneurysm have been reported in a patient with Marfan syndrome and Behcet disease, respectively . Management of primary cardiac sarcomas with cardiac transplantation is controversial as these tumors are known to have recurred in the allograft .
| Chagas disease |
| Amyloidosis |
| Iron overload |
| Giant cell myocarditis |
| Sarcoidosis |
| Primary cardiac sarcomas |
| Complications related to thrombosis, connective tissue, and collagen vascular disease |
In a small percentage of cases, pathologic evaluation of the explanted recipient heart yields findings that do not support the pretransplant clinical diagnosis. One study of over 200 transplants found a discordance rate of 8% between clinical and pathologic diagnoses . In another large series of nearly 300 transplants, incongruity between morphologic and clinical diagnoses occurred in 13% of cases . The discrepancy rate may be higher in centers that have a low incidence of pretransplant EMB evaluation . In most cases, the discrepancies involve conditions presenting as dilated cardiomyopathy and found to have obstructive coronary artery disease, active myocarditis, sarcoidosis, hypertrophic cardiomyopathy, noncompaction left ventricular cardiomyopathy, and arrhythmogenic right ventricular cardiomyopathy/dysplasia .
VAD are implanted in patients with refractory end-stage heart failure either as a bridge to transplantation or as destination therapy. Situations where there are relative contraindications for transplantation at the time of VAD implantation in which improvement in the patients’ conditions eventually make them eligible for transplantation after a period of VAD support are referred to as “bridge to decision” or “bridge to candidacy” . Recovery of left ventricular function after VAD support is infrequent, although young age, nonischemic etiology of heart failure, and symptom duration of less than a year are favorable factors for device explantation and sustained recovery .
Continuous flow pumps are the most commonly used type of VAD currently (see Chapter 5: Pathophysiology of Heart Failure and an Overview of Therapies, and Chapter 19: Tumors of the Cardiovascular System: Heart and Blood Vessels ). At the time of transplantation, the explanted heart and mechanical device should be examined for possible device-related complications . These complications include thrombosis, infections, and device malfunction . Device thrombosis results in hemolysis and pump dysfunction with a high mortality if left on medical management only . Mechanical causes of thrombosis include malpositioned inflow cannula and deformation of the outflow graft secondary to bend relief disconnection . Impingement on the interventricular septum or lateral wall and malpositioning after ventricular remodeling are possible causes of partial occlusion of the inflow cannula. Most of the cases, however, are without clearly identifiable mechanical etiology for thrombosis. Thrombi should be looked for in the inflow cannula, within the pump housing, and in the outflow cannula and conduit. VAD infection can be classified according to site into endocarditis/pump or cannula infection, device pocket infection, or driveline infection, with driveline infection being the most common. Soft tissue or material adherent to the driveline or pump and its connections should be submitted for microscopic evaluation in cases of VAD infections. Device malfunction could be secondary to percutaneous lead damage located either external to the patient or adjacent to the pump .
Acquired commissural fusion of the aortic valve can be observed in patients on long-term VAD support and is occasionally associated with clinically significant aortic insufficiency . The commissural fusion is due to diminished flow across the aortic valve as the left ventricle is unloaded and blood is diverted through the pump into the aorta.
Another complication associated with the use of VAD is the development of HLA antibodies. Patients with left VAD (LAVD) seem to have a higher incidence of sensitization, likely because of immunogenicity of the VAD, upregulation of cytokines during implantation, and blood product transfusion. While some have proposed increased risk of acute rejection in sensitized bridged patients with a VAD, current data suggest that highly sensitized patients have similar rates of treated acute rejection episodes in the first year after transplantation regardless of VAD utilization .
The success of cardiac transplantation has increased the need for an expanded supply of donor hearts. Gross abnormalities of donor hearts may be detected at the time of procurement or during preparation for implantation. Incidental abnormalities such as a bicuspid aortic valve or a patent foramen ovale do not typically preclude use. A patent foramen ovale is sutured at the time of transplantation. Bench repair of valvular abnormalities and valvular replacement have been successfully performed prior to transplantation .
Atherosclerosis in the donor heart may preclude adequate preservation during procurement and transport, particularly if ventricular hypertrophy is also present. Even in young adults, significant coronary artery disease is not unusual . Nineteen percent of 94 male Korean War casualties (mean age 21 years, range 18–37 years) had at least one coronary artery narrowing that exceeded 50%; 6% had narrowing in one or more coronary artery that exceeded 75%. Although routine coronary angiograms of donor hearts are generally not feasible, angiography can be selectively performed for male donors >45 years and female donors >50 years or when cardiac risk factors are known . In the absence of pretransplant angiogram, donor-transmitted coronary atherosclerosis defined as stenosis of at least 50% is reported in approximately 7% of cases. Intravascular ultrasound (IVUS) study reveals occult atherosclerotic plaques in more than 50% of recipients early after transplantation . Atherosclerosis involving two or three vessels in the donor heart is associated with early graft failure (EGF) .
Transmission of infectious diseases, including cytomegalovirus (CMV) and Toxoplasma gondii , from donors to recipients has been well-documented . The presence of antibodies to CMV in a donor does not preclude transplantation, but recipients may be at increased risk for primary infection or reactivation, depending on their serologic status before transplantation. CMV-seronegative recipients receiving CMV-positive organ have a 25%–40% chance of developing CMV infection . While most of these infections occur in recipients of CMV-seropositive donors, CMV infection may also occur in 10%–20% of seronegative recipients of seronegative organs . Primary CMV infections can cause serious complications in the immunosuppressed transplant recipient. In addition, CMV has been considered as a possible etiologic factor in the development of cardiac allograft vasculopathy (CAV) . Despite the absence of active infection, a donor may transmit T. gondii to a recipient through latent myocardial cysts which become reactivated during immunosuppression . Less than 5% of Toxoplasma -seropositive recipients, regardless of donor serology, develop a mild clinical infection. However, Toxoplasma -seronegative recipients who receive hearts from Toxoplasma -seropositive donors develop a clinical illness in up to 75% of instances . These infections carry substantial morbidity and mortality, requiring prophylaxis in seronegative patients.
Other infectious agents, such as hepatitis B and C , HIV , malaria , and Trypanosoma cruzi can potentially be transmitted from donor to recipient. On the other hand, donor hearts from patients dying of septic shock or meningitis due to bacterial infections could be utilized and have not been associated with significant recipient bacteremia or other infectious complications . Intensive monitoring and prompt implementation of therapy or effective prophylaxis lessens the risk of developing symptomatic disease. The advent of direct-acting antiviral agents has allowed heart transplantation from HCV-viremic donors to uninfected recipients. While nearly all HCV-negative recipients become infected, HCV viremia was cleared with early treatment and was associated with comparable 1-year survival to those with HCV-negative donors .
Except for those with low-grade skin cancers and primary central nervous system tumors, persons with history of active or recent malignancy are generally not eligible for organ donation. The most common malignancies transmitted from donors to recipients in solid organ transplantation are renal cell carcinoma, melanoma, and choriocarcinoma . However, donor-transmitted malignancies are extremely rare in heart transplantation. In a series of heart transplant recipients with donor-derived malignancies, the tumor histologic types identified were medulloblastoma, melanoma, choriocarcinoma, lung, and prostate adenocarcinoma . One of the most common reasons for donor-transmitted malignancies is a misdiagnosed etiology of spontaneous intracranial hemorrhage resulting in brain death that is subsequently determined to be caused by a brain metastasis.
Brain death in the donor may induce segmental or global myocardial dysfunction. Although the mechanisms are not fully understood, they may be related to (1) high catecholamine levels preceding brain death with norepinephrine release leading to coronary vasospasm or direct myocardial injury; (2) hemodynamic deterioration after brain death leading to stunned myocardium (prolonged postischemic ventricular dysfunction); and (3) reduced circulating cortisol, thyroid hormone, insulin, and antidiuretic hormone levels, resulting in a reduction in oxidative metabolism . Moreover, the administration of large doses of vasopressive drugs to support a donor heart prior to procurement may cause direct myocyte toxicity or constriction of small intramyocardial vessels with resultant microinfarcts. Lesions resulting from donor or perioperative ischemia may coexist with, and must be differentiated from, acute rejection.
The major sources of morbidity and mortality following cardiac transplantation are EGF, allograft rejection, multisystem organ failure, and infection in the first 3 years while CAV, malignancy, and renal failure become more common after 5 years . In the longer-term, malignancy becomes the most important cause of death. Despite the risk of complications after transplant, nearly 60% of recipients are free from hospitalization in the first year after transplantation .
EGF, defined as a composite endpoint of death or retransplantation associated with graft failure within the first 30 days after transplant, is the leading cause of early mortality after heart transplantation . EGF may be due to factors involving the donor, recipient, or surgical procedure. The differential diagnosis of graft failure very early in the posttransplant period includes impaired contractility due to ischemia in the donor or perioperative period, unrecognized coronary artery disease, donor–recipient weight mismatch, technical surgical problems such as uncontrolled bleeding, hyperacute rejection, right ventricular failure due to pulmonary hypertension in the recipient, and postoperative vasoplegia syndrome . In the absence of an identifiable cause, graft dysfunction within the first 24 hours after the transplant surgery is referred to as primary graft dysfunction. This can be further classified into left or biventricular or primarily right ventricular dysfunction for appropriate pharmacologic management and institution of mechanical circulatory support. Retransplantation may be indicated in select patients.
Hyperacute rejection is a rare event with a reported rate of <1% that continues to decline in frequency with improved pretransplant DSA screening. It is a complement-meditated injury to the graft which occurs immediately or within a few hours of heart transplantation . Settings in which hyperacute rejection may occur include the presence of (1) preformed ABO antibodies in the recipient; (2) preformed antibodies to the HLA system present in the allograft; (3) preformed antibodies to donor vascular endothelial cell antigens; and (4) following xenotransplantation. Predisposing factors to hyperacute rejection include prior blood transfusions, repeated pregnancies, multiple cardiac surgeries, and previous transplantation. With the development of VAD therapies, some patients can survive hyperacute rejection by being supported by short-term VAD usage and rituximab or plasmapheresis to remove preformed antibodies .
The pathologic principle underlying hyperacute rejection is that of an antibody-mediated toxicity by antibodies present in the recipient at the time of transplantation and directed against antigens in the graft resulting in its destruction . Preformed IgG and/or IgM antibodies deposit on donor organ vascular endothelial cells leading to activation of recipient complement. The combination of antibodies plus complement as well as other serum factors leads to endothelial cell activation and disruption. This, in turn, results in the loss of vascular integrity, enhanced expression of cell surface molecules, cytokine secretion, and activation of clotting and fibrinolytic cascades. The end result is microvascular thrombosis with hemorrhage, myocardial and vascular necrosis, and graft failure .
A diagnosis of hyperacute rejection may be made on EMB, but this type of rejection is more often encountered in an explanted heart of a recipient undergoing retransplantation or at autopsy. The heart is typically heavy with diffuse hemorrhagic discoloration of the myocardium. Histologically, there is diffuse interstitial hemorrhage and edema. Small vessels contain aggregated red cells and fibrin thrombi. If the patient survives long enough, myocyte and vascular degeneration and eventual necrosis with a neutrophilic response ensues.
While right ventricular failure is an important factor in early postoperative cardiac dysfunction following heart surgery in general, acute right ventricular failure or biventricular dysfunction with low output are common causes of death early after cardiac transplantation. Isolated acute right ventricular failure usually results when the normal right ventricle of a donor heart is unable to contract effectively against an elevated pulmonary vascular resistance in the recipient. The right ventricle becomes dilated with impaired contractility. Inadequate right ventricular output leads to inadequate left ventricular filling and hypotension. An EMB in this setting is frequently not helpful and may show early ischemic injury that may, or may not, account for the extent of myocardial dysfunction.
Left ventricular or biventricular dysfunction is most often caused by myocardial stunning due to ischemia or suboptimal myocardial preservation during the operative procedure and usually resolves within 48–72 hours. During this initial time course, patients can be aided by inotropic support, the use of temporary VADs , or extracorporeal membrane oxygenation .
Both functional tricuspid and mitral valve regurgitation have been observed in patients following cardiac transplantation, possibly related to altered chamber geometry and size. In most instances, the regurgitation is mild and is asymptomatic. In some cases, however, clinically significant regurgitation may require valvular repair or replacement.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here