Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Analysis. Analyze the problem in thirds.
Endpoint. Know what normal looks like, so you know your surgical endpoint.
Do not be destructive. Do not do anything to the ear that cannot be reversed.
Skin is precious but weak. Preserve skin in the sulcus, and do not rely on skin tension to maintain ear position.
Lobule. Consider lobule setback in every case.
Asymmetry. In asymmetric cases, operate on both ears most of the time.
Facelifts are otoplasties. Do not deform the tragus, lobule, or sulcus.
“Otoplasty” refers to surgical changes in the shape or position of the ear.
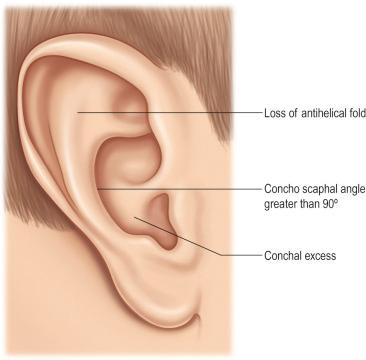
The most common indication is the patient with prominent but normally shaped ears.
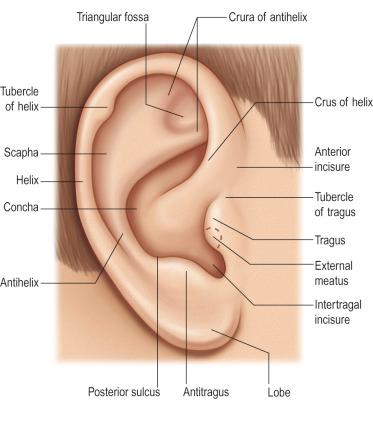
The single most important exercise for the surgeon, before performing any procedure in the otoplasty spectrum, is to have the characteristics of a normal ear firmly in his/her mind. With proper choice of technique, the surgeon can usually avoid the uncorrectable problems of overcorrection and unnatural contours ( Figs. 5.1 and 5.2 ).
It has also never been shown that an otoplasty retards auricular growth.
Otoplasty is unique in that it is perhaps the only cosmetic procedure that can be performed in childhood, and both parents and grandparents may be involved in surgical decision making for the patient who cannot yet express himself or herself.
The overall size and shape of the ear is evaluated to determine if the ear is prominent with an otherwise normal size and configuration, or if there are abnormalities in addition to the prominence.
The upper third of the ear is evaluated to determine if it is prominent, if the antihelix/superior crus of the triangular fossa is well formed, and if the helical rim is well defined.
The middle third of the ear is evaluated to determine if the concha is overly deep or protruding.
The relationship between the antihelix and the helix is examined to determine if any underdevelopment of the antihelix/superior crus in the upper third extends into the middle third or if it is confined to the upper third.
The lobule is evaluated to determine if it is prominent.
Even if the lobule is not particularly prominent on initial examination, it may become prominent once the upper two-thirds of the ear have been corrected.
Asymmetry is noted, mostly because patients and families will always comment on it.
In asymmetric cases, it is usually preferable to operate on both ears rather than attempt to set back only the prominent ear to match its less prominent counterpart (see Fig. 5.1 ).
The degree of prominence/deformity and the age at presentation will determine when a surgical recommendation is made.
For young children with very prominent ears and whose parents desire early correction, otoplasty is recommended as early as age 4 years.
Four years of age can be viewed as a minimum for most otoplasty procedures.
When the entire ear requires reconstruction, as in microtia, this author prefers to wait until approximately 10 years of age.
In some cases, the parents may want the child to participate in the decision process, and that will necessitate later intervention.
It is common to have patients present at approximately 18 years of age, when they are legally independent, or later when they have earned the money for the procedure.
It is not unusual for adults at almost any age to request correction, either because they have wanted it all their lives or because their desire to have other procedures (e.g., a facelift) has led to the realization that their ears are also prominent.
While the delicate, complex contours of the ear may be difficult to create de novo (i.e., microtia), anatomic considerations are minimal in standard otoplasty.
There is abundant blood supply, making almost any combination of incisions acceptable without the risk of necrosis.
There are no motor nerves in the neighborhood. The terminal branches of the great auricular nerve will always be injured, but normal sensory function usually returns.
The one anatomic structure that can be compromised in otoplasty is the external auditory canal (conchal setback narrows the meatus). Otherwise, the anatomic considerations of otoplasty are those of preservation:
Preservation of the sulcus.
Preservation of the natural softness of the auricular contours.
Preservation of the normal landmarks such as the posterior wall of the concha (i.e., the middle third of the antihelix).
Otoplasty surgery is all about the endpoint. The right endpoint can be achieved with a thorough knowledge of a normal ear. If the surgeon remembers the following regarding how the ear should look from various vantage points, it will aid tremendously in the intraoperative decision making:
From the front, the helical rim should be visible, poking out from behind the antihelix.
From the side, the contours of the ear should be round and soft, never sharp.
From behind (and this is the most helpful to the surgeon who is sitting behind the patient intraoperatively), the contour of the helical rim should be a straight line, not a “C”, or a “hockey stick”, or any other shape. If the helical contour is a straight line, it almost ensures that a harmonious correction will be achieved.
Regardless, if the ultimate correction is slightly under- or slightly overcorrected, a harmonious correction will read as “normal” to the outside world, and almost all patients will be happy. This is perhaps the single most important lesson from this chapter.
The last judgment is how close to the head the ear should be placed. The final position of the ear should be overcorrected minimally to allow for some relapse, but not enough to create an unsatisfactory result if no relapse should occur.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here