Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
|
|
|
|
|
|
|
|
|
|
The causes of cervical deformity are diverse and may include systemic conditions, such as ankylosing spondylitis and rheumatoid arthritis, as well as neuromuscular, degenerative, posttraumatic, neoplastic, and iatrogenic conditions. Surgical intervention should be considered if the patient does not respond to a conservative treatment protocol or shows evidence of deteriorating myelopathy, radiculopathy, or functional impairment, such as inability to achieve horizontal gaze, swallowing dysfunction related to head position, tension- or kyphosis-induced myelopathy, or neck pain resulting from head imbalance. The spinal cord may be decompressed effectively by an anterior, posterior, or combined approach, but full decompression may require deformity correction, as in cases of kyphosis. Supplemental posterior fixation minimizes the risk of anterior dislodgment of the graft even in the presence of solid anterior fixation. Treatment of these complex cervical deformities is challenging and requires a clear understanding of the disease and the patient. Surgeons must be comfortable with remobilizing the spinal column anteriorly and posteriorly, with vertebral artery anatomy, and with methods of anterior and posterior correction.
Significant, irreducible deformity of the cervical spine may be sufficient to require corrective osteotomy. At the craniocervical junction, neurologic or functional impairment associated with the deformity may be best managed by osteotomy and fixation. Rigid deformities of the cervical spine below the craniocervical junction are more likely to require some type of osteotomy to correct the deformity and restore horizontal gaze.
This chapter details the preoperative considerations and surgical procedures of four cervical osteotomies: (1) craniocervical junction osteotomy using sequential anteroposterior approaches, (2) Smith-Petersen osteotomy (SPO), (3) cervicothoracic junction pedicle subtraction osteotomy (PSO), and (4) cervical circumferential osteotomy.
Patients may give a history of past trauma, sometimes associated with an intercurrent illness of ankylosing spondylitis or rheumatoid arthritis, as well as previous cervical spine surgery or degenerative and neoplastic disorders.
Symptoms may include suboccipital headache and neck stiffness, occipital neuralgia, symptoms of myelopathy, or progressive deformity leading to functional impairment, such as difficulty with looking forward or with eating and drinking. Patients may report low back pain and standing fatigue resulting from use of compensatory muscles to elevate pelvic tilt to alter gaze angle.
Assessment of the patient with cervical kyphotic deformity should include a comprehensive neurologic examination. Signs of myelopathy may be evident because of past injury, compression, or spinal cord tension secondary to stretch induced by kyphosis. In addition to a complete neurologic examination, the surgeon should assess the patient’s regional and overall global alignment. Assessment of the location of the kyphotic deformity should include evaluation of not only the craniocervical relationship, but also the thoracolumbar spine and lumbopelvic relationships. The angle from the brow to chin relation to the vertical line with the hips and knees extended and the neck in its fixed or neutral position (chin-brow to vertical angle) can be used to measure the degree of flexion deformity.
Clinical and radiographic assessments should be performed with the patient’s hips and knees in the extended position to obtain a better understanding of the sagittal alignment and the location of the deformity. This is important because occasionally the focus of the deformity lies within the thoracolumbar spine or lumbar pelvis. In addition, examination of the pelvis may reveal hip flexion contractures. Occasionally, lumbar sagittal deformities must be corrected first. Correction of lumbar imbalance alters head position substantially, especially in rigid deformities such as ankylosing spondylitis. However, all corrective lumbar osteotomies change the T1 slope angle to some extent and therefore change cervical alignment and often cervical C2 sagittal vertical axis.
The deformity should be evaluated by anteroposterior and lateral cervical radiographs along with dynamic lateral flexion and extension views. The deformity is then accurately measured (i.e., sagittal angle determination), and any other abnormalities are noted (e.g., subluxation and pseudarthrosis). The surgeon should obtain full-length posteroanterior and lateral 36-inch scoliosis radiographs to examine overall sagittal and coronal balance in these patients. The authors assess cervical, thoracic, and lumbar sagittal alignment individually and globally, define the effect of regional imbalance on cervical balance, and determine whether it is a primary, secondary, or compensatory cervical deformity. The degree of required correction depends on the angle of the cervical deformity (the chin-brow to vertical angle), the C2 plumb line, and the desired final lordosis.
The goals of treatment are to obtain balance, horizontal gaze, and spinal cord decompression and to normalize spinal cord tension. Dynamic (i.e., flexion and extension) radiographs permit assessment of the overall flexibility of the cervical spine that is paramount when designing a treatment strategy. Computed tomography (CT) scans of the cervical spine are also useful in determining the presence of fusion or ankylosis of the facet joints and disks and allow assessment of fixation points such as C2 and upper thoracic pedicles.
All patients should be evaluated with preoperative magnetic resonance imaging or CT myelography. These image modalities permit the evaluation of compressive disease. If significant ventral compressive disease (disk, osteophyte) is present, a ventral decompressive procedure may first be performed before correction of the deformity.
When planning surgical deformity correction for cervical kyphosis, the surgeon should consider whether the deformity is rigid or fixed and whether the patient has neurologic symptoms. Figure 37-1 demonstrates the surgical decision-making process in cervical deformity osteotomy. In the craniocervical junction, osteotomy is indicated when the deformity is irreducible and sufficient to result in severe pain or in functional or neurologic impairment that cannot be relieved with a surgical decompression or stabilization procedure alone. In flexible subaxial deformity, posterior stabilization (usually C2 to T2) is advocated; when deformity is semirigid Smith-Petersen osteotomy should be considered.
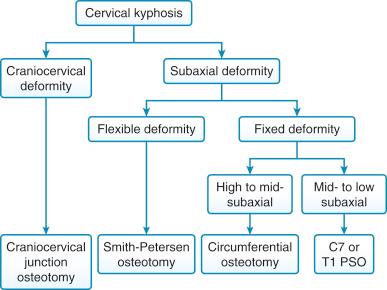
However, in the clinical setting of rigid cervical kyphosis (high cervical to midcervical kyphosis) with neurologic symptoms, the spinal cord is usually tethered over the subaxial kyphotic segment, thus leading to neurologic symptoms and myelopathy. Therefore, segmental kyphosis correction (circumferential osteotomy) is mandatory to untether and decompress the spinal cord. In the setting of rigid cervical kyphosis in the mid- to low cervical spine with cervical sagittal imbalance, C7 or T1 PSO may be sufficient.
At the craniocervical junction, it is unusual for osteotomy to be required, and little has been published on the subject in the surgical literature. However, cases exist, usually in the posttraumatic setting and in association with other conditions such as ankylosing spondylitis or end-stage rheumatoid arthritis with fixed atlantoaxial deformity, in which neurologic or functional impairment associated with the deformity may be best managed by osteotomy and fixation.
Osteotomy is indicated when the deformity is irreducible (possibly following a trial of traction) and sufficient to result in severe pain and functional or neurologic impairment that cannot be relieved with a surgical decompression or stabilization procedure alone. The procedure is contraindicated in the presence of significant osteoporosis or debilitating comorbidities.
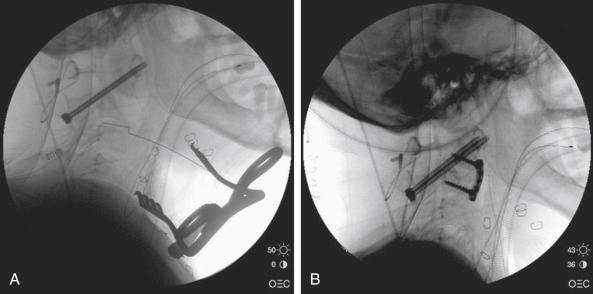
Figure 37-2 is a case example of craniocervical junction osteotomy. Plain radiographs at the atlantoaxial level reveal substantial kyphotic deformity, possibly in the presence of an old odontoid fracture, with subluxation or dislocation of the C1-C2 joints (see Fig. 37-2 , A to C ). The patient may have bony union across the subluxed joints or involving other elements of the atlantoaxial complex.
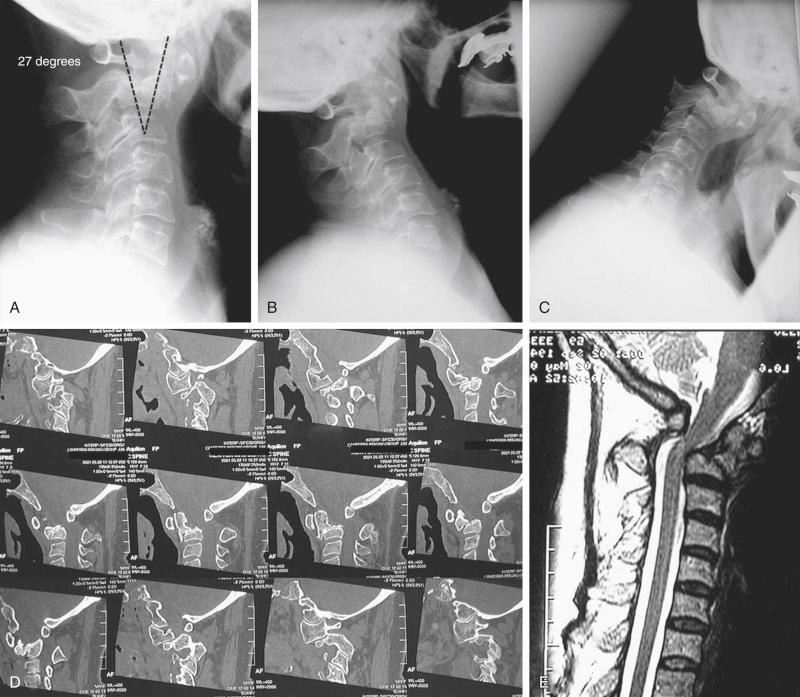
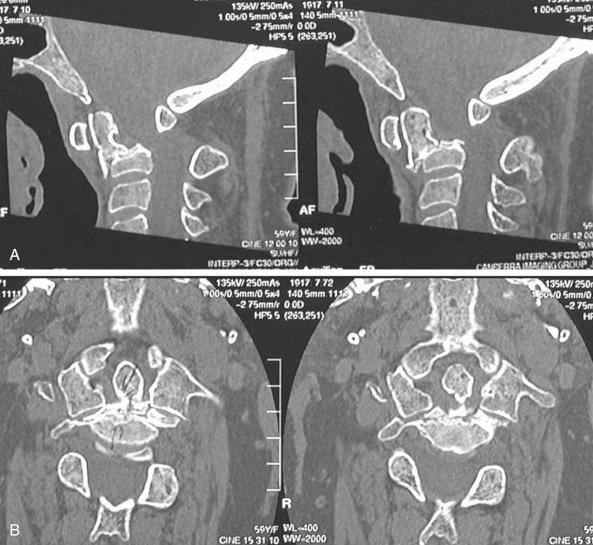
The ease of surgical access to the ventral aspect of C2 is an important consideration when choosing between an anterior-posterior approach and a posterior-only approach. Grundy and Gill described a posterior-only approach in cases in which the anticipated anterior access may be difficult. Preoperative planning of the intended osteotomy orientation is also important when considering the type of anterior approach. An osteotomy, which is oriented obliquely backward and upward from the base of C2 ( Fig. 37-3 , A ), enables satisfactory exposure through a high anterior retropharyngeal approach. This approach is described later.
Anesthesia and positioning: The patient usually requires awake endoscopic intubation and is positioned supine for the first (anterior) stage of the surgical procedure. It is preferable to use an operating table such as the Jackson table (Mizuho OSI, Union City, Calif.), which permits rotation of the patient to the prone position for the second surgical stage, and to secure the patient’s head in a Mayfield three-point head holder. Access for adjustment of the head and neck position should be maintained throughout the procedure. Intraoperative image-guided surgical navigation, such as with an O-Arm/Stealth (Medtronic, Dallas, Tex.), Iso-C (Siemens, Erlangen, Germany), or similar system may facilitate the surgeon’s orientation and placement of the osteotomy. Intraoperative neuromonitoring may be helpful during deformity reduction.
A high anterolateral skin incision is made for a retropharyngeal approach to the C2 vertebral body.
A retropharyngeal approach to the ventral aspect of the C2 vertebral body is used, with fluoroscopic confirmation of position.
The longus colli muscles are mobilized bilaterally.
The old fracture line is identified (when present). The bilateral extents of the fracture line are defined, and the surgeon endeavors to dissect upward to define the lateral aspects of the odontoid process bilaterally ( Fig. 37-3 , B ). This maneuver is important to mobilize the odontoid with the osteotomy completely and to avoid injury to the vertebral arteries.
The osteotomy is made through the old fracture line by using a high-speed drill with a small cutting burr. Frequent position and orientation checks are made with fluoroscopic or image guidance. The osteotomy is extended through to the back of the odontoid and bilaterally. The surgeon should take care not to venture too widely, to avoid injury to the vertebral arteries. If necessary, navigation may be used.
Depending on whether bony union of the posterior elements of the C1-C2 complex is present, an attempt may be made at this stage to open up the fracture line and correct the deformity by using intervertebral spreaders.
The anterior wound is then closed over a suction drain before the patient is turned to the prone position.
Through a midline suboccipital incision, subperiosteal dissection of the posterior elements of C1 to C3 is performed with identification of the C2 nerve roots.
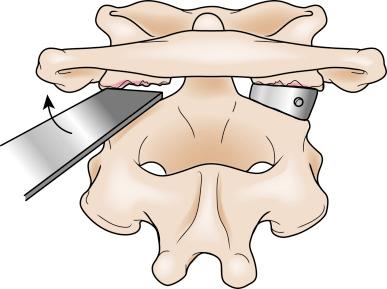
While controlling any hemorrhage from the venous plexus around the C2 nerve roots, the superior articular surfaces of C2 are exposed, and the posterior edges of the C1 lateral masses, adjacent to the inferior joint surfaces, are defined on each side. If any bony union has occurred between the C1 and C2 joints, this is divided with the high-speed drill or osteotome ( Fig. 37-4 ). Dissectors are then carefully inserted into the dislocated C1-C2 joints and are used to lever back the C1 lateral masses gently onto C2 while the surgical assistant and anesthesiologist adjust the patient’s head position in the Mayfield headholder.
It is helpful to remove the articular cartilage from the C2 joint surfaces before reducing the dislocation. Subsequently, the articular cartilage is removed with a small, angled curet from the inferior surface of the C1 lateral masses. Cancellous bone graft is then placed into the C1-C2 joint spaces.
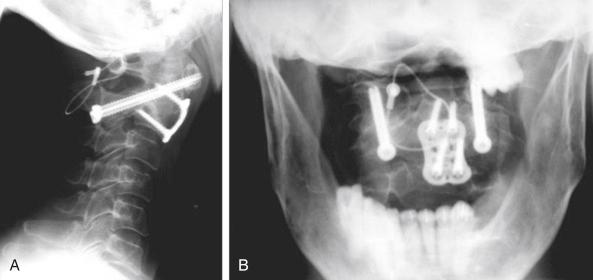
Depending on the surgeon’s preference and the vertebral artery anatomy, the C1-C2 segment is then stabilized using either transarticular screws (with additional posterior wiring) or a C1 lateral mass and C2 pars screw construct.
Further bone graft is placed over the decorticated posterolateral elements before posterior wound closure, in layers, over a vacuum drain.
Depending on how the patient is tolerating the procedure and the time available, the patient may be repositioned supine immediately or later, as a delayed procedure, for placement of bone graft into the anterior osteotomy site. This will have opened up into a wedge-shaped defect following the posterior deformity correction ( Fig. 37-5 , A ). Suitably fashioned allograft or iliac crest autograft is inserted into the wedge-shaped osteotomy site and secured with a small locking plate ( Fig. 37-5 , B ). Subsequent, standard postoperative care is given following segmental atlantoaxial stabilization and fusion ( Fig. 37-6 ).
The patient is then returned, ventilated, to the intensive care unit.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here