Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Osteofibrous dysplasia (OFD) is a benign fibro-osseous lesion characteristically occurring in children younger than 10 years, with an age range from newborn to 39 years. Most cases (95%) arise in patients younger than 15 years. Males and females are equally affected. Characteristically, these lesions occur in the diaphysis of the tibia, with a small proportion exhibiting synchronous fibular involvement. Involvement of the fibula alone is rare, and involvement of other bones, including the ulna and radius, although documented, is extremely rare. The majority of patients have pain, swelling, and deformity. It may also present as congenital pseudoarthrosis.
| OFD | OFD-like Adamantinoma | Classic Adamantinoma | Dedifferentiated Adamantinoma | |
|---|---|---|---|---|
| Age | Mainly children younger than 10 years | Mainly in children, younger than classic adamantinoma | Mean age at presentation 30 years | Mean age at presentation 51 years |
| Radiologic features | Affects the cortex of the diaphysis of the tibia as an intracortical radiolucency, well marginated with surrounding sclerosis Periosteal reaction is rare No soft tissue extension |
Same as classic adamantinoma | Osteolytic, eccentric, expansile, and medullary in location with –characteristic soap-bubble appearance Extracortical extension into soft tissue in 15% of cases |
Similar to classic adamantinoma |
| Morphology | Osteofibrous lesion in which the woven bone shows prominent osteoblastic rimming | Osteofibrous lesion, small nests of epithelial cells | Obvious nests of epithelial cells arranged in various patterns within a fibrous or fibro-osseous stroma | Areas of classic adamantinoma, juxtaposed with high-grade sarcoma |
| Keratin staining | Single positive cells, no clusters | Small nests of keratin-positive cells | Positive in the epithelial component | Reduced to absent staining pattern for cytokeratins in areas of sarcomatous dedifferentiation |
| Molecular cytogenetic alterations | Trisomies in 7, 8, 12, and 21 | Trisomies in chromosomes 7, 8, 12, 19, and 21 | Trisomies in chromosomes 7, 8, 12, 19, and 21 KMT2D gene alterations multiple recurrent chromosomal gains and losses and CNVs, and EGFR |
Same as classic adamantinoma, some suggest additional p53 gene mutation |
| Local recurrence | None | ∼20% | Up to 90% | Aggressive clinical course |
| Metastasis | None | Rare | 12%–29% | Frequent |
Osteofibrous dysplasia affects the cortex of the diaphysis of the tibia as an intracortical radiolucency, which is well marginated with surrounding sclerosis ( Figs. 22.1 and 22.2 ). It may have a ground-glass texture. Multiple lucencies with intervening sclerosis are frequent. The lesions are elongated and can vary in size from several centimeters to involvement of most of the bone, some being circumferential. Although medullary involvement may occur, the medullary margin is sclerotic and well-defined with narrowing of the medullary canal. The cortex is usually thickened or expanded, or both. Periosteal reaction is rare, and is thick and solid when present. Soft tissue extension is not seen. Bowing is common and is usually anterior.


The lesion is confined to the cortex and is white to yellow-brown with a firm fibrous, sometimes gritty consistency ( Fig. 22.2D ).
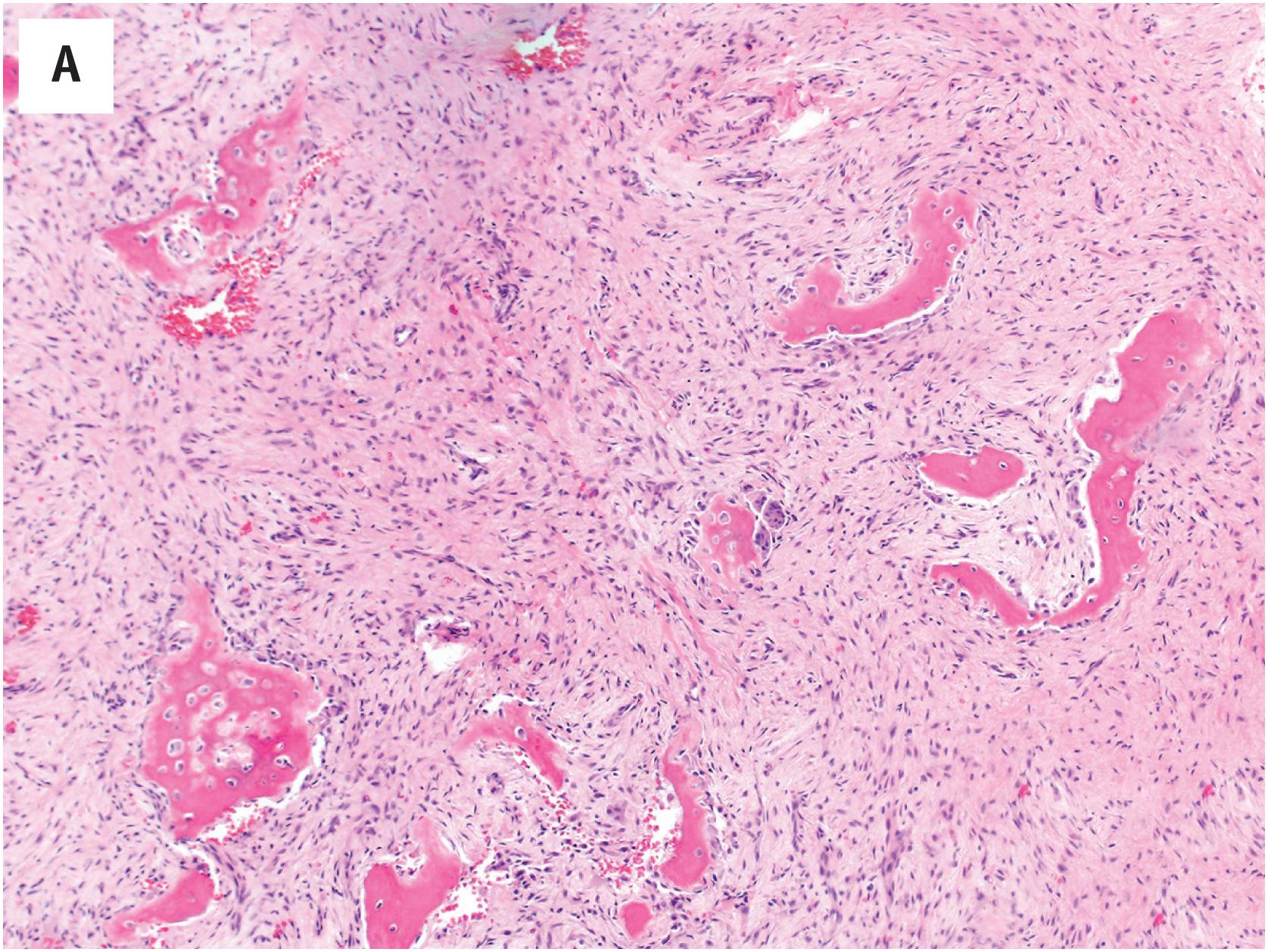
Histologically, OFD has a distinct zonal architecture. The central portion is composed predominantly of fibrous tissue which may have a loose, somewhat myxoid appearance, usually shows a storiform pattern ( Fig. 22.3A–C ) and may contain irregularly distributed woven bone ( Fig. 22.3B–C ). The bone formation gradually becomes more extensive, being composed of an admixture of woven and lamellar bone, the latter predominating at the periphery of the lesion, where it merges with either the cortical bone or the reactive sclerotic bone at the medullary aspect. Scattered osteoclasts are present, sometimes clustered. Foamy histiocytes are rare, and aneurysmal bone cyst formation is not seen. In areas the tumor may simulate fibrous dysplasia. Groups of epithelial cells are not present.
In approximately 80% of cases with characteristic hematoxylin and eosin histologic features of OFD and lacking recognizable epithelial cells, scattered, isolated, keratin-positive cells are present within the fibrous stroma ( Fig. 22.3D ). These keratin-positive cells show a “basal cell” immunophenotype, with strong expression of keratins 14 and 19, and a lesser degree of keratin 5 and 14 expression. Keratins 8 and 18 are absent. This pattern of expression is also seen in adamantinoma. Clusters of keratin positive epithelial cells are not seen.
In a small number of cases tested, clonal chromosomal abnormalities have been identified, including trisomy 7, 8, 12, and 21. Extra copies of one or more of these chromosomes have also been found in osteofibrous dysplasia-like (differentiated) adamantinoma and classic adamantinoma. Mutations for Gs α protein and NFI gene have not been detected. Expression of epidermal and fibroblastic growth factors and their receptors (EGF, EGFR, and FGF-2) has been identified in OFD.
OFD must be distinguished from fibrous dysplasia and both classic and osteofibrous dysplasia-like adamantinoma. Fibrous dysplasia is centered in the medulla, not the cortex, and consists almost entirely of woven bony trabeculae lacking osteoblastic rimming. In contrast, the bony trabeculae in osteofibrous dysplasia show prominent osteoblastic rimming. One should be cautioned, however, that areas of fracture may show bone with osteoblastic rimming (in addition to other reactive features such as hemorrhage, hemosiderin deposition, and xanthomatous change), and that osteoblasts may be present in the peripheral portions of long-standing examples of fibrous dysplasia. Keratin-positive cells are not seen in fibrous dysplasia.
A diagnosis of osteofibrous dysplasia-like adamantinoma (juvenile or differentiated adamantinoma) should be made when scattered small nests of epithelial cells are identified on the routinely stained slides (i.e., not by immunohistochemistry alone). Such cell clusters are usually found in the center of OFD-like adamantinoma lesions. In classic adamantinoma, the epithelial component predominates with only small osteofibrous dysplasia-like areas, located chiefly at the periphery of the lesion. Because the epithelial component is irregularly distributed and sparse in OFD-like adamantinoma, complete curettage of the lesions and complete sampling of the curetted material is paramount for accurate diagnosis
Based on the two largest series of cases, OFD appears to undergo spontaneous regression at puberty in most patients. The local recurrence rate after curettage or local resection is approximately 25%. It is therefore recommended that surgery be delayed until after puberty unless dictated by the presence of extensive disease with associated deformity and fracture. In these cases, stabilization procedures without actual excision may be indicated. The overwhelming majority of patients with a diagnosis of OFD-like adamantinoma follow a benign course. Rare cases exist where full-blown classic adamantinoma occurred even with a complete and adequate sampling of the original lesion. The rate of evolution has varied from 5 to 17 years. Excision of lesions after puberty is indicated if increasing growth of the lesion, deformity, or both occur.
Adamantinoma is a low-grade and slow-growing primary malignant bone tumor of uncertain histogenesis that typically arises in long bones, predominantly in the mid-portion of the tibia, with or without the involvement of the fibula. Synchronous involvement of tibia and fibula occurs in approximately 10% of all patients. Adamantinoma involving other bones has very rarely been reported, including the radius, ulna, femur, humerus, olecranon, ischium, spine, and rib. Adamantinoma constitute 0.1% to 0.5% of all malignant bone tumors. A wide age spectrum exists, but they usually affect male patients between the ages of 20 to 50 years with only approximately 3% of patients being younger than 10 years. The initial symptoms are often indolent and nonspecific; however, the majority of patients present with swelling. Symptoms may be present >30 years before diagnosis. The tumor is locally aggressive, and local recurrence or metastasis may develop years after the diagnosis of the primary lesion.
Benign fibro-osseous lesion of childhood occurring in an intracortical location predominantly in the midshaft of the tibia with or without involvement of the fibula
Rare, less than 1% of all primary bone tumors
Diaphysis of tibia, predominantly anterior cortex
Occasional involvement of fibula
Rare documented cases in radius and ulna
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here