Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
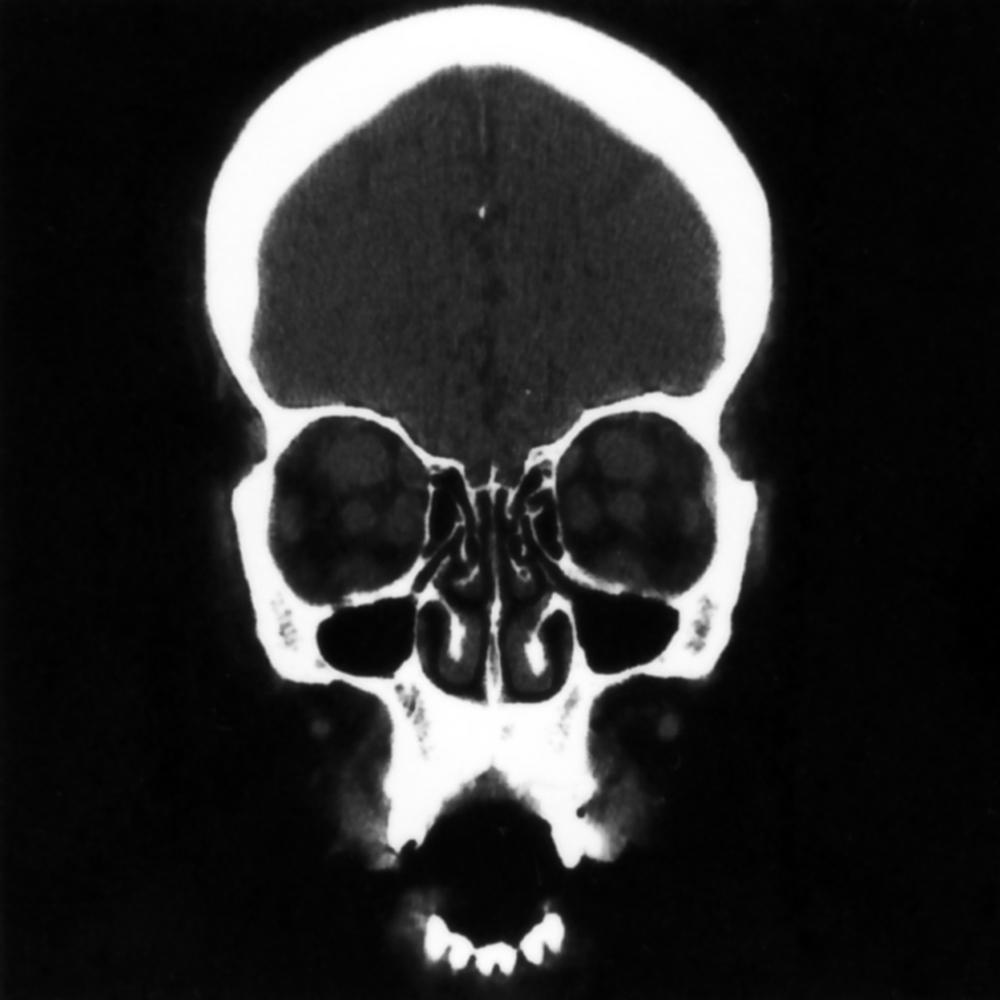
Decompression of the orbit may be considered for the treatment of space-occupying lesions causing compromise of function as a result of expansion of the orbital contents or a decrease in the rigid orbital confines. The volume of the orbit averages about 30 mL, and it is only anteriorly that it is not bound by bone. By far, the most common indication for decompression is Graves orbitopathy, but similar surgical techniques are applied to infectious, traumatic, neoplastic, and iatrogenic etiologies (e.g., orbital hematoma after sinus surgery) ( Figs. 151.1 and 151.2 ).

The incidence of Graves disease in the general population is about 1% to 3%. Females are affected about 5 times as often as men, but older men who experience orbitopathy often have a more fulminant course. About one-third of patients with Graves disease will have orbitopathy, often asymmetrical and usually mild or moderate. Approximately 85% of patients evaluated primarily for orbitopathy will be found to have a dysthyroid state. In adults, Graves disease is the most common cause of unilateral and bilateral proptosis. The first report of decompression for this condition occurred in 1911.
The pathogenesis of Graves orbitopathy remains only partially understood. Serum levels of antibodies to the thyroid-stimulating hormone (TSH) receptor and collagen XIII seem to correlate with orbital disease activity. TSH receptors are found on orbital fibroblasts, which may differentiate into adipocytes, and are more sensitive to TSH receptor antibodies than dermal fibrocytes. The proptosis is due to an increase in retrobulbar glycosaminoglycan deposition and edema and to a later increase in retrobulbar adipose tissue. Smoking is thought to affect this by creating increased oxygen-reactive species or by causing local tissue hypoxia, both of which lead to increased chemokines recruiting T cells from the bloodstream. TH2 cells are the predominant type involved in the orbital disease.
The acute phase of the disease, which consists of orbital congestion, inflammatory cell infiltrate, and forward movement of the globe, generally lasts between 6 and 24 months. After this phase, the disease is characterized pathologically by increased fibrosis of the tissues. A second acute phase may occasionally affect the patient later in life. Asymmetrical involvement of the orbits occurs frequently.
The only external factor proven to affect Graves orbitopathy is cigarette smoking. Current smoking outweighs previous smoking as a predictor of disease severity. Patients in whom orbital disease develops are 4 times as likely to smoke, and discontinuation of smoking appears to lessen the severity and protect patients from the development of further symptoms. Pretibial myxedema, thyroid acropachy (swelling of digits and toes), and female sex are also associated with more severe orbital disease.
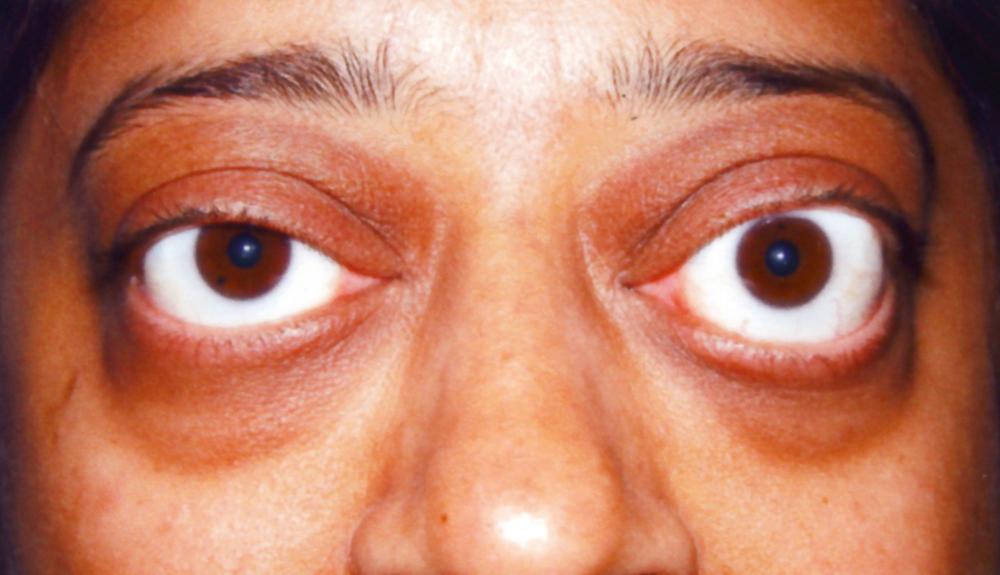
Symptoms of Graves orbitopathy include eyelid retraction, proptosis, diplopia, dryness of the eyes, a sensation of pressure behind one or both eyes, and swelling of the eyelids and conjunctiva (chemosis). Signs consist of eyelid retraction more than 1 mm from the limbus, eyelid lag on downward gaze (failure of the upper eyelid to descend properly when the patient looks down), unilateral or bilateral proptosis, restriction of extraocular movements (particularly upward gaze and abduction), hyperemia over the insertions of the horizontal rectus muscles, and corneal staining with fluorescein observed with a cobalt filter ( Figs. 151.3 and 151.4 ).

The courses of the orbital disease and any associated thyroid disease in Graves disease are independent. Euthyroid patients may have severe orbitopathy causing optic neuropathy or corneal perforation, whereas severely hyperthyroid patients may have no orbital signs or symptoms. Treating the thyroid abnormalities is essential to the patient’s general health, but it is unlikely to help the eye disease. Exceptions are removal of a large goiter, which may lessen the orbital symptoms, and treatment with radioactive iodine, which sometimes acutely worsens the condition of the orbits (ameliorated by concurrent treatment with oral steroids).
Orbital decompression is sometimes undertaken for other causes of proptosis: infection with abscess, tumor, trauma to the optic nerve, or hematoma (such as might occur after endoscopic sinus surgery). Abscesses located along the lamina papyracea in the orbit or medially along the roof or floor are most amenable to endoscopic drainage. Occasionally, an orbital apex tumor causing compressive optic neuropathy (CON) may be successfully treated by decompression when resection of the tumor is inadvisable.
Whenever possible, defer orbital decompression in Graves patients until the disease has been treated medically and is no longer active.
In cases of poorly responding optic neuropathy or impending corneal perforation, it may be necessary to operate during the active phase of the disease.
The number of walls decompressed correlates directly with the reduction in proptosis. The most reasonable approach appears to be the balanced decompression: removal of the medial and lateral walls of the orbit. A recent meta-analysis suggests that the average reduction in proptosis is 4.5 mm regardless of the method used. The roof is rarely decompressed, and decompressing the orbital floor gives a higher likelihood of new postoperative diplopia.
Smoking
Thyroid status (euthyroid; previous treatments to render the patient euthyroid)
Previous eye surgery
Diplopia
In primary gaze
In other positions of gaze
Previous sinus problems/surgeries
Complete eye examination by an Ophthalmologist
Best corrected visual acuity
Color vision
Extraocular movements
Pupillary responses
Intraocular pressure
Biomicroscopic examination of ocular surface and posterior segment
Hertel exophthalmometry (measures projection of each globe beyond the orbital rim)
Nasal endoscopy. Endoscopic examination of the nasal cavity is performed to identify structural abnormalities that may interfere with surgery (septal deviation), coexistent disease that needs to be addressed at the time of surgery (nasal polyposis), and conditions that need to be treated prior to surgery (acute or chronic rhinosinusitis).
Computed tomography (CT) (no contrast) of maxillofacial structures to determine whether there is sinus disease or septal deviation and assess the relative size of the extraocular muscles and orbital adipose tissue compartments. Other anatomic variations that may pose a problem during surgery include a low cribriform plate, Onodi cells, Haller cells, or non-pneumatization of sinuses.
Magnetic resonance imaging (MRI; particularly T2 sequence) of orbits if there is any question whether the disease is active (inflammatory phase)
Urgent decompression during active phase of inflammation (for Graves):
Compressive optic neuropathy
Corneal ulceration
Elective decompression after the disease is quiescent (for Graves):
Proptosis
Sensation of pressure or pain
Dryness of the eyes
Subluxation of the globe
Active sinus infection. Adequate medical or surgical management of sinus infection is necessary before orbital surgery due to the risk of infection spreading to the orbital tissues.
Coagulopathy
Unacceptable anesthesia risk
CT scan
Image-based navigation is optional and is not necessary unless there are anatomic variations or changes from prior surgery that obscure anatomic landmarks. If an optic nerve decompression is planned at the same time, navigation is helpful to identify the course of the optic canal and internal carotid artery.
Preoperative counseling is particularly important so that the patient understands that this procedure, when performed for Graves disease, is likely to be the first in a series of surgeries. Strabismus surgery may be performed for unresolved diplopia, and eyelid surgery (either correction of retraction or blepharoplasty) may be required after that.
Decide whether septoplasty or additional sinus surgery is necessary.
Bilateral orbital decompression
Only rarely does it makes sense to stage this operation in a case of bilateral disease; however, there are a few patients in whom the orbitopathy is very asymmetrical and one orbit only may be decompressed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here