Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On completion of this chapter, you should be able to:
Discuss gestational sac growth, take measurements, and assess gestational age
Describe how to perform a crown-rump measurement and evaluate growth
Measure, calculate the biparietal diameter, head circumference, three-dimensional cranium, abdominal circumference, and extremity measurements
Assess fetal parameter measurements, proportions, and fetal growth
Describe when other measurements should be used to provide additional clinical information
Evaluate the fetal growth time-series for intrauterine growth restriction and growth disturbances
Reliably assessing gestational age and the growth of the fetus has long posed a challenge to all who care for pregnant women. Although not without value, clinical parameters lack the necessary consistency for optimal perinatal care. With recent advances in diagnostic sonography, however, fetal age and growth can be assessed with high accuracy.
The difference between menstrual and fetal age is important to establish in clinical obstetrics. Fetal age begins at conception and is also known as conceptional age . Conceptional age is restricted to pregnancies in which the actual date of conception is known, as found in patients with in vitro fertilization or artificial insemination. If conceptual age is already known, the menstrual age may be found by adding 14 days to the conceptual age.
Obstetricians date pregnancies in menstrual weeks, calculated from the first day of the last [normal] menstrual period (LMP) . This method is called menstrual age or gestational age . The sonography student must understand that gestational ages are estimated from measurements of fetal parameters and are not the actual age of the parameters. The estimated ages are no more accurate than the measurements taken, and all parameters in a fetus will not result in the same fetal age because fetuses have different body size proportions.
It is clinically important to know the menstrual age of a patient because this information is used for the following reasons:
In early pregnancy to schedule invasive procedures (chorionic villus sampling and genetic amniocentesis)
To interpret maternal serum alpha-fetoprotein screening
To plan date of delivery
To evaluate fetal growth
Before the use of sonographic determination of fetal growth, menstrual age was calculated by three factors: (1) the menstrual history, (2) physical examination of the fundal height of the uterus, and (3) postnatal physical examination of the neonate. This process was not always reliable if the patient could not recall the date of her last period or if other factors—such as oligomenorrhea, implantation bleeding, use of oral contraceptives, or irregular menstrual cycle—were present.
Because all gestations do not deliver exactly at 40 weeks after LMP, specific terminology has been defined for the relative gestational age at term ( Box 52.1 ).
Early term: 37w0d to 38w6d
Full term: 39w0d to 40w6d
Late term: 41w0d to 41w6d
Post-term: 42w0d to delivery
Transvaginal sonography enables visualization and evaluation of intrauterine pregnancies earlier than was previously thought possible. The earliest sonographic finding of an intrauterine pregnancy is thickening of the decidua. Sonographically, this appears as an echogenic, thick filling of the fundal region of the endometrial cavity occurring at approximately 3 to 4 weeks after the normal LMP ( Box 52.2 , Fig. 52.1 ).
A distended urinary bladder affects the gestational sac measurement; it changes its shape from round to ovoid or teardrop.
If the sac is round, measure one GSD diameter inner to inner (all three diameters equal).
If the sac is ovoid, make two measurements inner to inner, one transverse and the other perpendicular to the length. Take the third GSD inner to inner.
The three GSD diameters are averaged for the diameter of record.
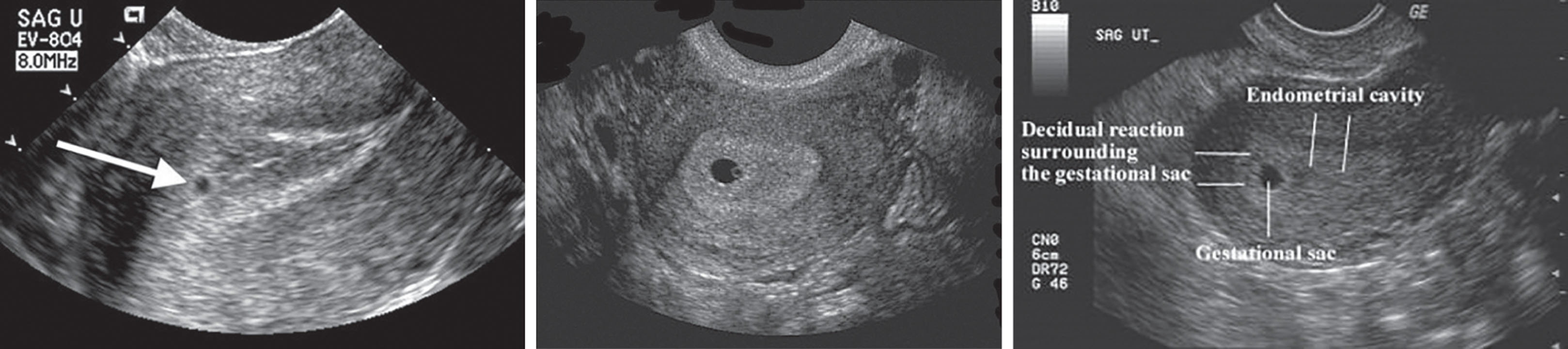
At approximately 4 weeks of menstrual age, a small hypoechoic area appears in the fundus or midportion of the uterus, known as the double decidual sac sign . As the sac embeds further into the uterus, it is surrounded by an echogenic rim and is seen within the choriodecidual tissue. This is known as the chorionic or gestational sac ( Fig. 52.2 ).

At 5 weeks after the LMP, the average of the three perpendicular internal diameters of the GSD—calculated as the mean of the anteroposterior diameter, the transverse diameter, and the longitudinal diameter—can provide an adequate estimation of menstrual age ( Fig. 52.3 ). A gestational sac should be seen within the uterine cavity when the β-human chorionic gonadotropin (β-hCG) is above 500 mIU/mL (second international standard). This becomes especially important when evaluating a pregnancy for ectopic implantation.
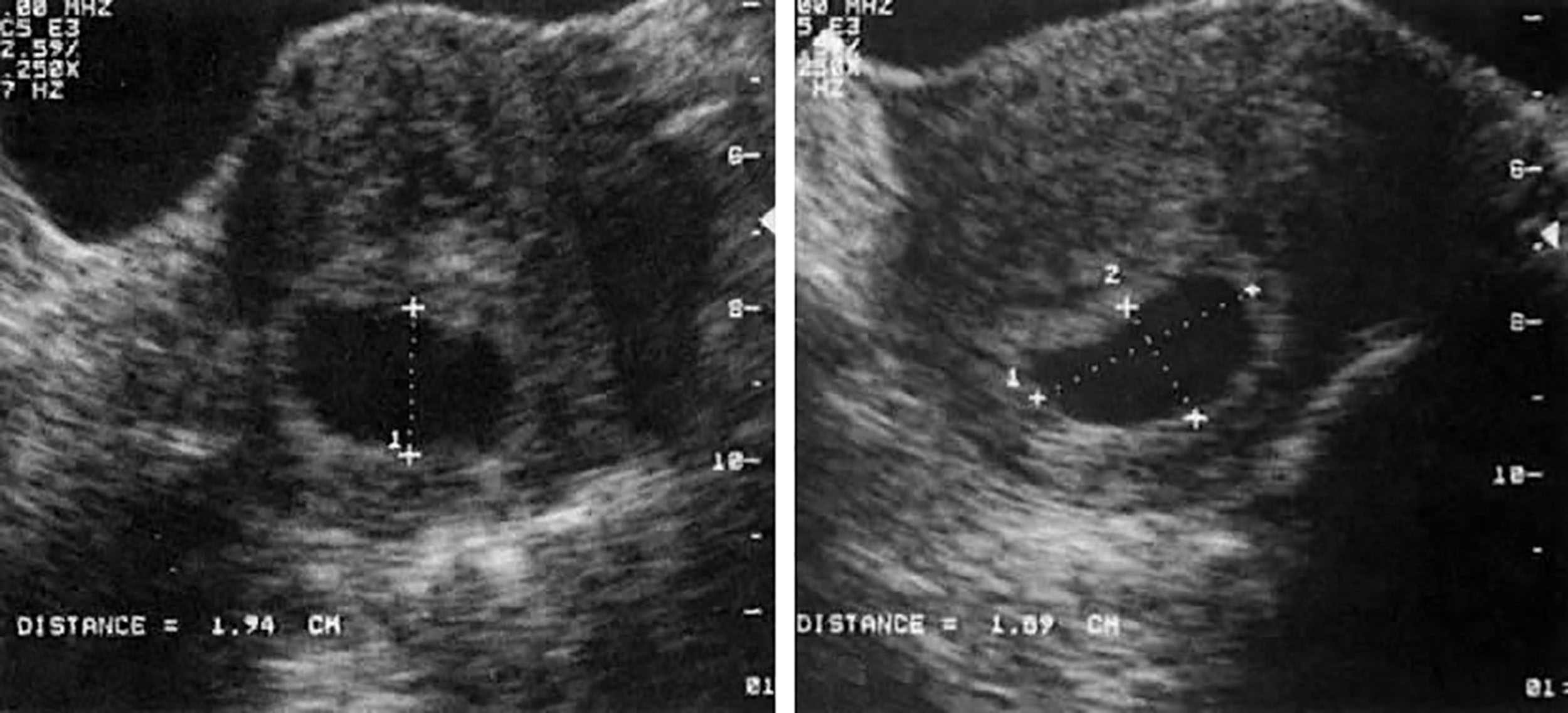
The sac grows rapidly in the first 10 weeks, with an average increase of 1 mm/day (see Table 52.1 ). According to one report, a gestational sac growing less than 0.7 mm/day is associated with impending early pregnancy loss. Even the most experienced sonographer may incorporate a measuring error; therefore, the β-hCG test in conjunction with a sonographic evaluation is suggested in a sequential time frame.
| Gestational Age (Weeks) a | MSD |
|---|---|
| 5.0 | 2 |
| 5.1 | 3 |
| 5.2 | 4 |
| 5.4 | 5 |
| 5.5 | 6 |
| 5.6 | 7 |
| 5.7 | 8 |
| 5.9 | 9 |
| 6.0 | 10 |
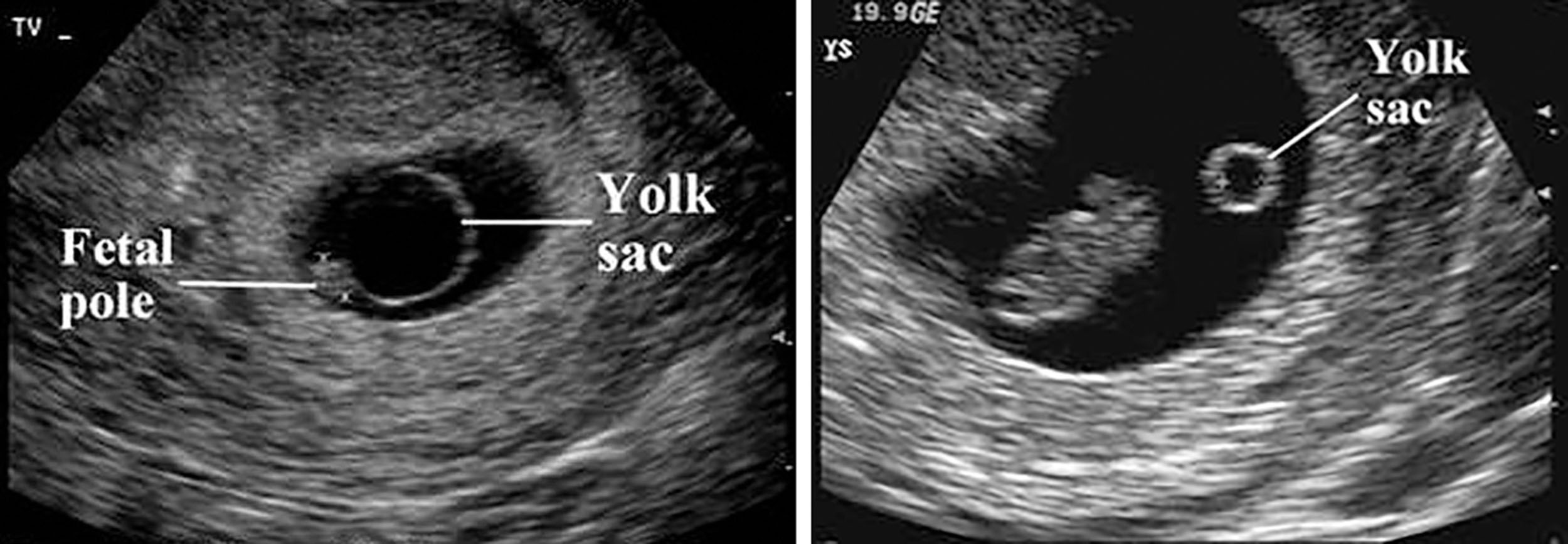
A yolk sac should be seen when the gestational sac exceeds 8 mm in mean internal diameter ( Fig. 52.4 ). The yolk sac is a small, spherical structure with an anechoic center within the gestational sac. It provides early transfer of nutrients from the trophoblast to the embryo. It also aids in the early formation of the primitive gut and vitelline arteries and veins and in producing the primordial germ cells. Yolk sac size has not been correlated with gestational age determination. Normal yolk sac size should be less than 6 mm. Yolk sacs greater than 8 mm have been associated with poor pregnancy outcomes and solid, echogenic yolk sacs. Box 52.3 lists sonographic landmarks for early pregnancy.
500 mIU/mL β-hCG = gestational sac seen
>8 mm gestational sac = yolk sac seen
>16 mm gestational sac = embryo seen
<6 mm yolk sac = normal
>8 mm yolk sac = abnormal
>7 mm fetal pole = positive cardiac activity
When the mean gestational sac diameter (GSD) exceeds 16 mm, an embryo with definite cardiac activity should be well visualized with transvaginal scanning. This usually occurs by the 6th menstrual week ( Fig. 52.5 ) but may be as early as the fifth LMP week with transvaginal sonography. The maternal urinary bladder must be filled to create an acoustic window for the transabdominal scanning approach. With this technique, the sac shape can vary secondary to bladder compression, maternal bowel gas, or myomas and should not be misinterpreted as abnormal.
Assessing gestational age using a single gestational sac diameter or even up to three averaged diameters yields an accuracy of only ±2 to 3 weeks in 90% of cases. Accordingly, gestational sac diameter has not been widely used as a determinant of gestational age after more accurate embryonic parameters can be measured (see Chapters 49 and 53 ).
With transvaginal sonography, embryonic echoes can be identified as early as 38 to 39 days of menstrual age ( Box 52.4 ). The crown-rump length (CRL) is usually 1 to 2 mm at this stage. The embryo is usually located adjacent to the yolk sac. The CRL is the most accurate sonographic technique for establishing gestational age in the first trimester ( Fig. 52.6 ). The reason for this high accuracy is the excellent correlation between fetal length and age in early pregnancy because pathologic disorders minimally affect the growth of the embryo during this time.
CRL can be measured from 6 to 12 gestational weeks by transvaginal sonography.
Measurements should be made along the long axis of the embryo from the top of the head (crown) to the bottom of the trunk (rump).
CRL is the most accurate fetal age measurement.
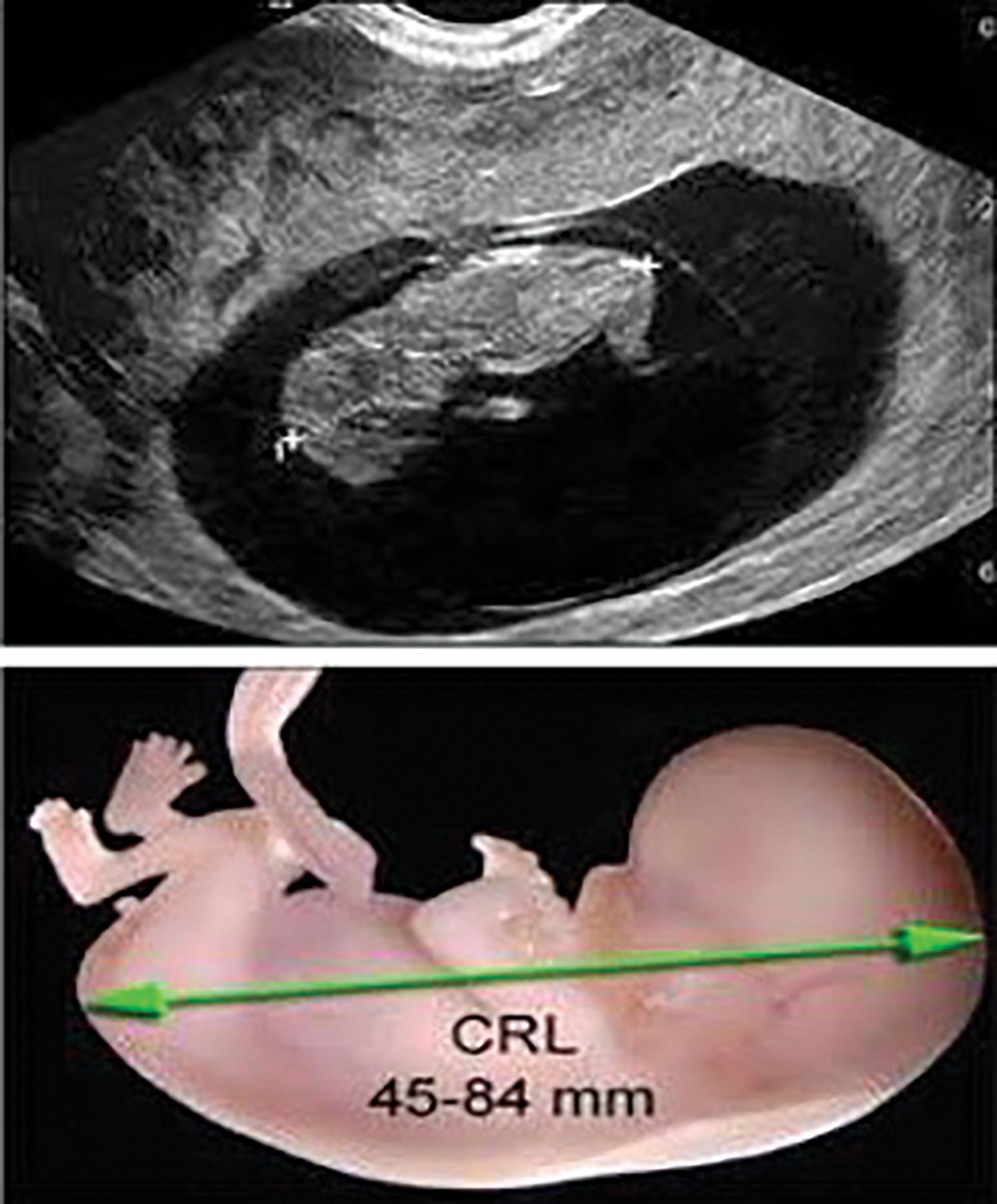
The embryo can be measured easily with real-time dynamic imaging. For transabdominal imaging, the mother’s bladder should be full to create an acoustic window. The measurement should be taken from the top of the fetal head to the outer fetal rump, excluding the fetal limbs or yolk sac ( Table 52.2 and Fig. 52.7 ). The accuracy is ±5 days with a 95% confidence level. The average of three separate measurements of the CRL may be obtained to determine gestational age.
| GA | CRL | GA | CRL | GA | CRL | GA | CRL | GA | CRL | GA | CRL | GA | CRL | GA | CRL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6.0 | 5 | 7.0 | 10 | 8.0 | 16 | 9.0 | 24 | 10.0 | 33 | 11.0 | 44 | 12.0 | 56 | 13.0 | 70 |
| 6.2 | 6 | 7.2 | 11 | 8.3 | 18 | 9.3 | 26 | 10.2 | 35 | 11.2 | 46 | 12.2 | 58 | 13.2 | 72 |
| 6.4 | 7 | 7.4 | 12 | 8.4 | 19 | 9.5 | 28 | 10.4 | 37 | 11.4 | 49 | 12.4 | 62 | 13.4 | 76 |
| 6.6 | 8 | 7.7 | 14 | 8.7 | 21 | 9.7 | 30 | 10.6 | 39 | 11.6 | 51 | 12.6 | 64 | 13.6 | 79 |
| 6.8 | 9 | 7.8 | 15 | 8.8 | 22 | 9.8 | 31 | 10.8 | 41 | 11.8 | 53 | 12.8 | 67 | 13.7 | 80 |

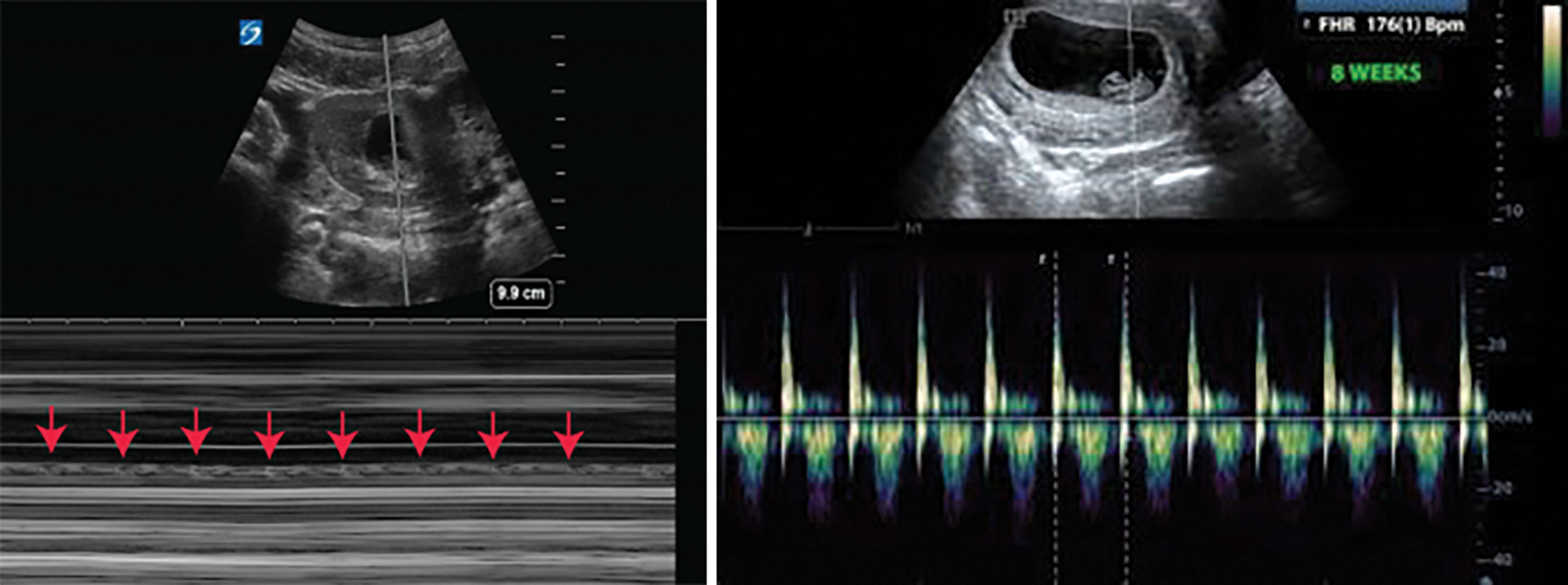
Cardiac activity should be seen when the CRL exceeds 7 mm, but it may be seen by transvaginal sonography once the CRL reaches 2 mm. It is generally accepted that it is good to follow patients with small CRL and no fetal heartbeat over a few days. In general, the CRL should increase at a rate of 8 mm/day. Occasionally an embryo is seen with no visible cardiac activity and a small CRL for menstrual age. It is advisable to wait a week and rescan to see if the patient spontaneously aborts the products of conception or needs medical intervention, such as a dilation and curettage procedure. Infrequently an appropriate fetal CRL and positive cardiac activity are seen after the week’s wait. Why this happens is not known, but experienced sonographers have observed it.
Absence of an embryo by 7 to 8 weeks of gestation is consistent with an embryonic demise or an anembryonic pregnancy. If a nomogram is not readily available to identify gestational age, a convenient formula is: Gestational age (weeks) = CRL (cm)+6. After the twelfth week, CRL is no longer considered accurate because of flexion and extension of the active fetus; therefore, other biometric parameters should be used.
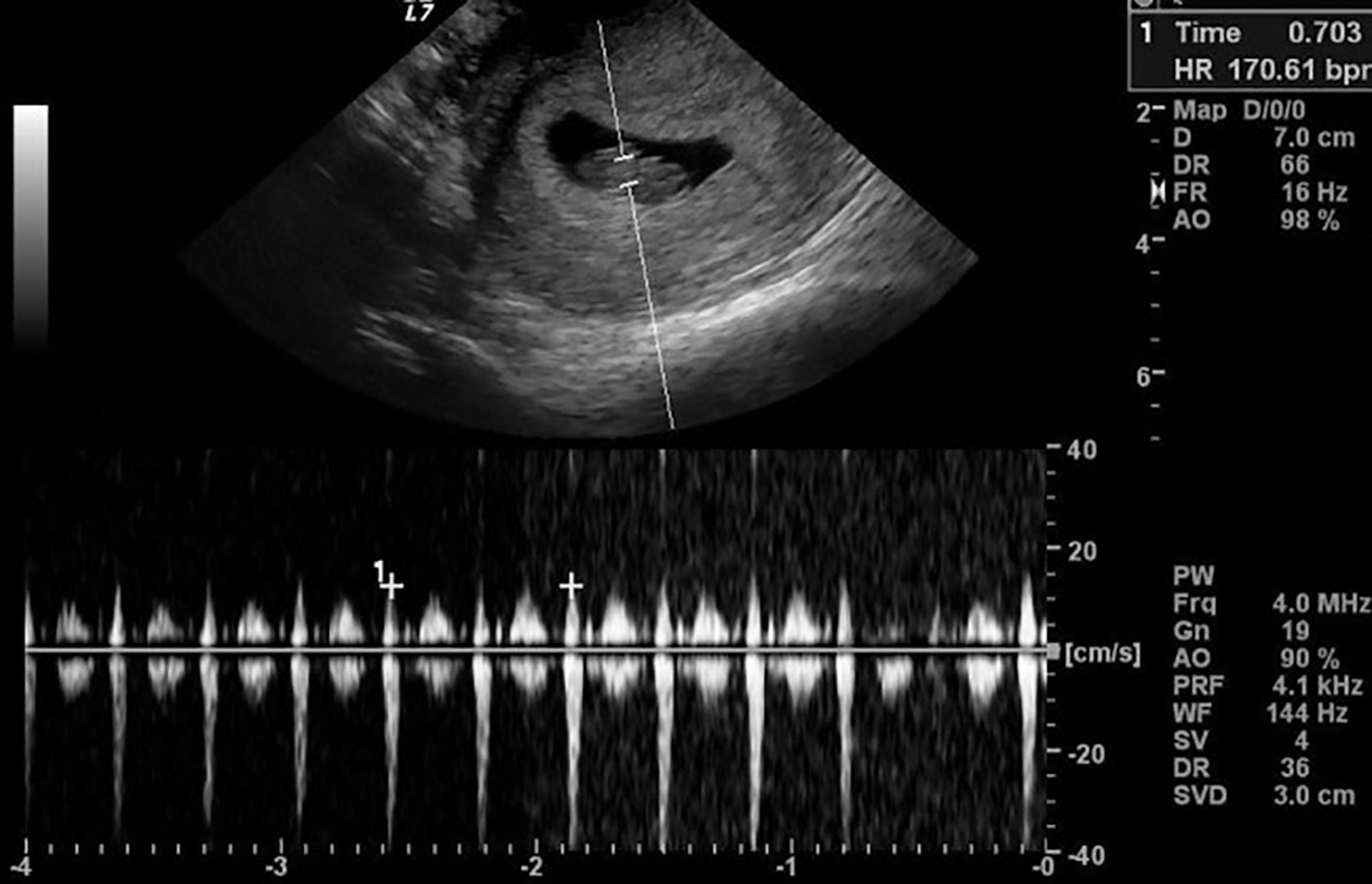
The embryonic heart rate (EHR) accelerates linearly during the first month of beating between the 5th and 9th gestational weeks ( Fig. 52.8 ). This linear acceleration correlates well with the embryonic age before the CRL reaches 2.5 cm or before approximately 9.2 LMP weeks. The mean rate of acceleration is 3.3 beats/min per day, 10 beats/min every 3 days, or approximately 100 beats/min between the start of beating until the early ninth week ( Box 52.5 ). The embryonic age in days can be estimated with the following formula:
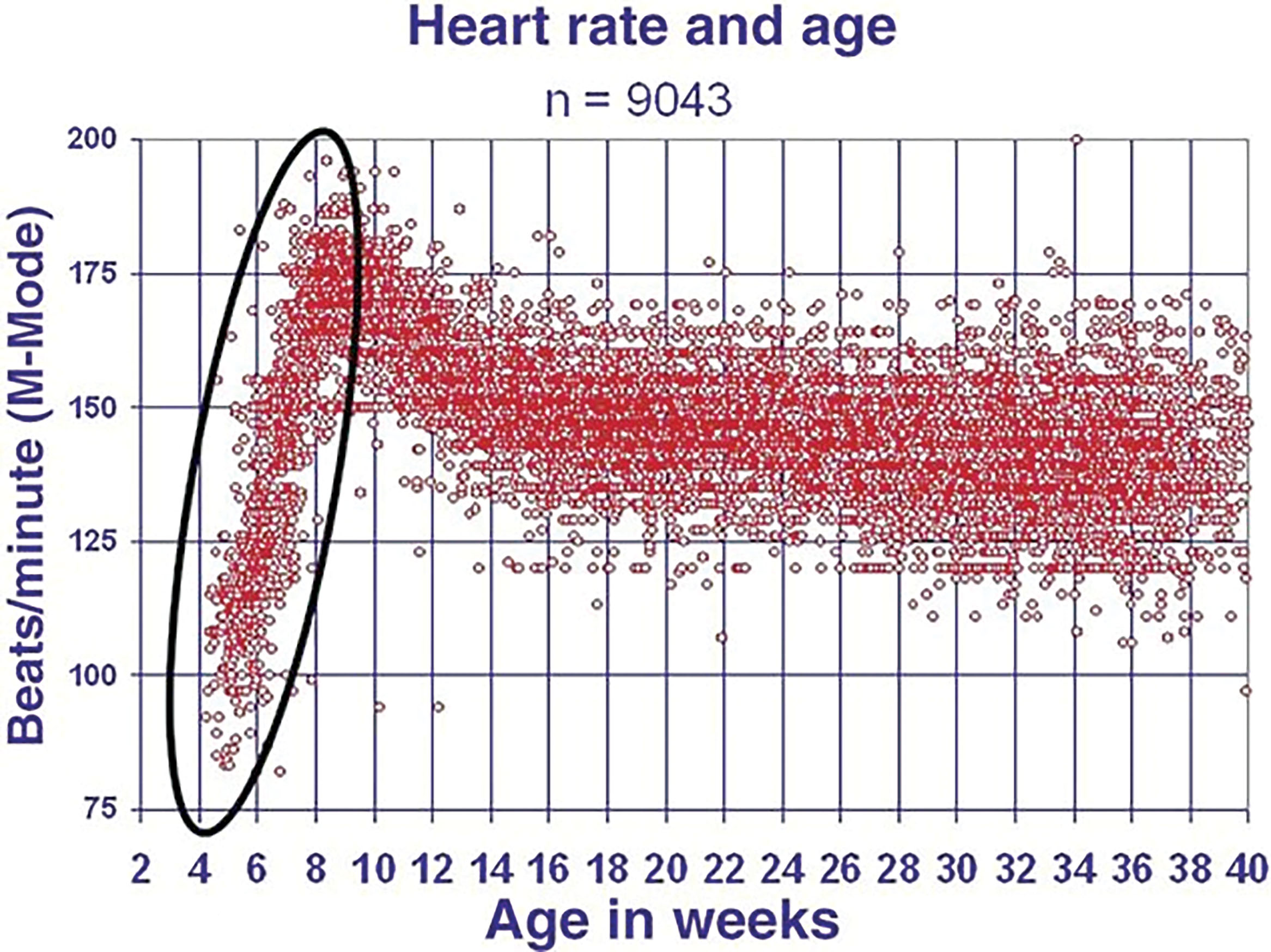
EHR can be measured by M-mode transvaginal sonography to estimate age from the early fifth to early ninth gestational weeks when the CRL is <25 mm.
The most accurate EHR measurements can be obtained by enlarging the two-dimensional image and using a fast sweep speed for the M-mode tracing. Measure from repeating distinct points on M-mode.
The EHR age will be accurate to within ±6 days. An EHR age that trails the CRL age by >6 days may be associated with impending first-trimester failure and warrants follow-up.
The normal EHR accelerates linearly at 3.3 beats/min/ per day, which is approximately 10 beats every 3 days, or 100 beats in the first month of beating.
The result of this estimation will be within ±6 days in 95% of normal pregnancies. If the age estimated by the CRL leads the age by EHR by more than 1 week, it may be prognostic for first-trimester failure and warrants follow-up. Because the heart rate is accelerating so rapidly during the embryonic period, accurate M-mode measurements are desirable. The greatest accuracy can be achieved by magnifying the embryo as much as possible and using a fast M-mode tracing to stretch out the heartbeats for more precise cursor placement. The cursors should be carefully placed on identifiable, repeating locations of the M-mode tracing ( Fig. 52.9 ).
In the second trimester, the gestational age parameters extend to the biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), femur length (FL), and other parameters that may be used. It is critical for the sonographer to know precisely which landmarks are necessary to determine these measurements. Proper gain settings, instrumentation, and fetal lie all influence the accuracy of measurements used to estimate the gestational age.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here