Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The trachea is a midline cartilaginous and fibromuscular tubular structure that extends from the inferior aspect of the cricoid cartilage to the carina. The intrathoracic length of the trachea normally ranges from 6 to 9 cm. The wall contains 16 to 22 horseshoe-shaped cartilage rings that are connected longitudinally by annular ligaments containing fibrous and connective tissue. The posterior wall of the trachea is membranous and contains transverse smooth muscle fibers of the trachealis muscle. Proximally, the trachea lies in close proximity to the skin surface but is posteriorly angulated as it descends inferiorly. The recurrent laryngeal and vagus nerves innervate the trachea, and sympathetic trunks provide sympathetic innervation. The left recurrent laryngeal nerve loops underneath the aortic arch and is located within or in close proximity to the tracheoesophageal groove. Arterial blood supply to the trachea derives from branches of the inferior thyroidal, intercostal, and bronchial arteries. The thoracic esophagus typically maintains a posterior location relative to the trachea; however, this varies, and the esophagus may be located laterally ( Fig. 2.1, A and B ).
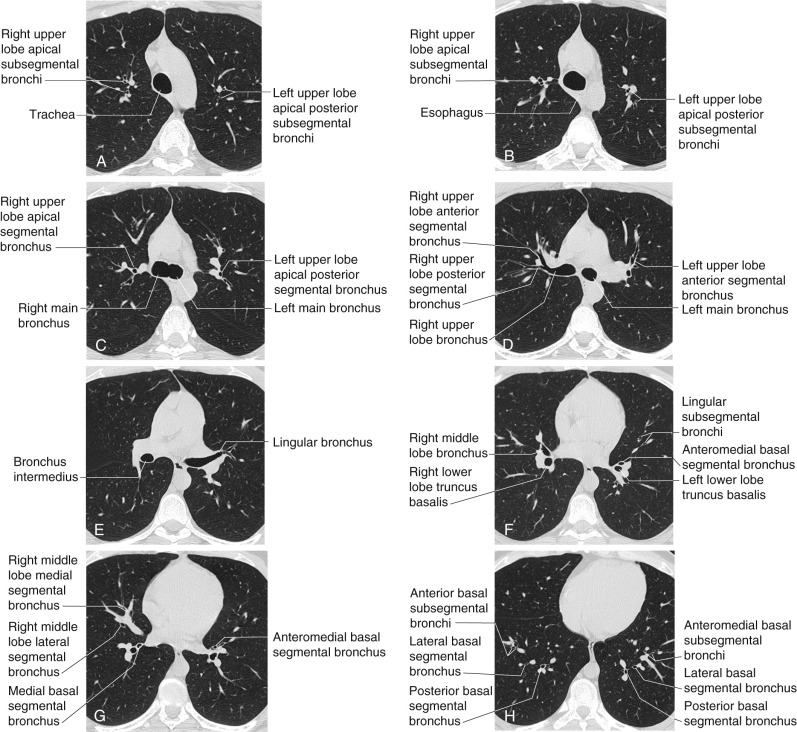
At the carina, the trachea divides into the right and left main bronchi ( Fig. 2.1, C ). The angle of bifurcation can either be measured as the interbronchial angle, which represents the angle between the central axis of each main bronchus, or the subcarinal angle, defined as the angle between the inferior aspect of both the right and left main bronchi. The normal carinal angle can range from 45 to 90 degrees but is usually approximately 60 degrees. A variety of pathologies may result in widening of the carinal angle, including left atrial enlargement, subcarinal masses or lymphadenopathy, lobar collapse, and presence of a pericardial effusion.
The right main bronchus has a more vertical course than the left and a shorter length (see Fig. 2.1, C ). The bronchial angle represents the angle created by the intersection of lines through the tracheal axis longitudinally and the origin of the bronchial axis. The steeper right bronchial angle and shorter length of the right main bronchus lead to a more accessible route for foreign bodies. However, in children up to 15 years of age, the right and left bronchial angles are relatively symmetric, with resultant near equal incidence of right- and left-sided aspiration in pediatric patients.
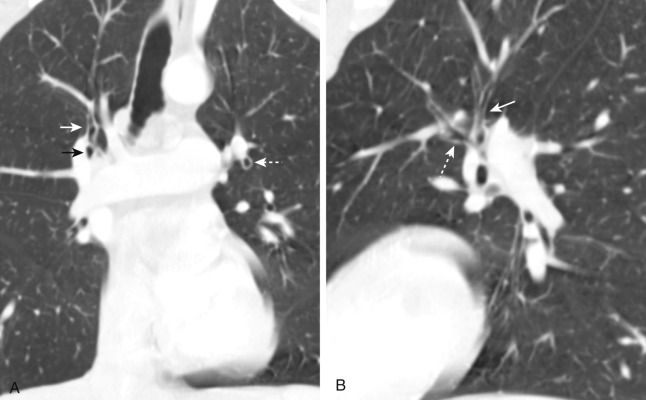
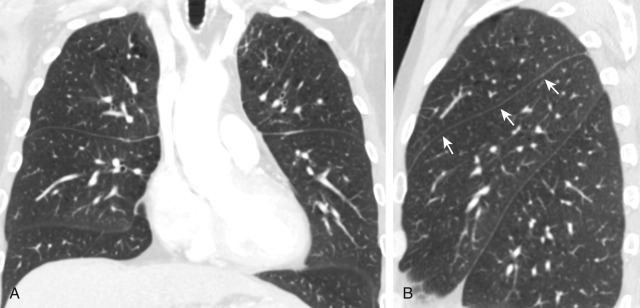
The right upper lobe bronchus arises from the lateral aspect of the right main bronchus, approximately 2 cm from the carina. The bronchus courses laterally and divides into three branches 1 to 2 cm from its origin, denoted anterior, posterior, and apical—each of which supplies a segment (see Fig. 2.1, C and D ). This normal trifurcation pattern has been shown to vary considerably, and many individuals have a variable bifurcation pattern of segmental bronchi in the right upper lobe. The anterior segmental bronchus is typically located in the axial scan plane on computed tomography (CT) (see Fig. 2.1, D ) and may appear as a rounded lucency on coronal CT images ( Fig. 2.2 ). The angle of the posterior segmental bronchus is directly slightly cephalad after its take-off and can be seen typically on CT as it ascends cranially (see Fig. 2.1, D ). The apical segmental bronchus can be identified on axial CT as a rounded lucency at the level of the carina (see Fig. 2.1, C ).
The bronchus intermedius continues distally for 3 to 4 cm following the origin of the right upper lobe bronchus and bifurcates into the right middle and right lower lobe bronchi ( Fig. 2.1, E and F ). The posterior wall of the bronchus intermedius approximates the superior segment of the right lower lobe and should be less than 3 mm in thickness. The right middle lobe bronchus originates from the anterolateral wall of the bronchus intermedius, nearly opposite from the origin of the lower lobe superior segmental bronchus origin (see Fig. 2.1, F ). It divides into the medial and lateral segmental bronchi approximately 1 to 2 cm beyond its origin, extending anteriorly and slightly inferiorly ( Fig. 2.1, G ).
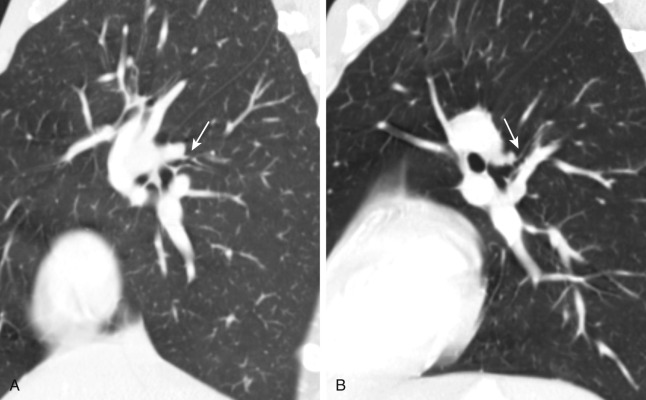
The nondivided segment of the right lower lobe bronchus is short. The superior segmental bronchus of the right lower lobe arises from the posterior wall of the right lower lobe bronchus near its origin. The superior segmental bronchus courses posteriorly and laterally for approximately 1 cm ( Fig. 2.3 ). After the superior segmental bronchus take-off, the right lower lobe bronchus continues caudally as the basal bronchial trunk or truncus basalis for 5 to 10 mm (see Fig. 2.1, F ). There are four basal segments in the right lower lobe: anterior, lateral, posterior, and medial, which is the order from the lateral to medial aspect of the hemithorax on the standard PA radiograph ( Fig. 2.1, H ). The first branch of the basal trunk is typically the medial basal segmental bronchus, which has an anterior relationship to the right inferior pulmonary vein ( Fig. 2.1, G ). The anterior and lateral basilar bronchi tend to have a somewhat oblique course, which can make it difficult to identify them on axial CT.
The left main bronchus is longer in length than the right and divides into the left upper and left lower lobe bronchi at a more caudal level than the right main bronchus (see Fig. 2.1, D ).
The left upper lobe bronchus arises from the anterolateral aspect of the left main bronchus and is 2 to 3 cm in length. In approximately 75% of cases, the left upper lobe bronchus bifurcates into superior and inferior divisions, the latter of which is the lingular bronchus. In the remainder of individuals, the left upper lobe bronchus trifurcates in anterior, apical posterior, and lingular bronchi. With the most common branching pattern, the superior division divides almost immediately into the apical posterior and anterior segmental branches (see Figs. 2.1, C and D , and 2.2 ). The anterior segmental bronchus can be seen at the level of the left upper lobe bronchus coursing anteriorly (see Fig. 2.2 ). The apical posterior segmental bronchus has a vertical course and therefore is imaged in cross-section at axial CT, appearing as a circular lucency above the anterior segmental bronchus origin (see Figs. 2.1, C , and 2.2 ).
The lingular bronchus originates from the inferior aspect of the distal left upper lobe bronchus, approximately 1 to 2 cm inferior to the right middle lobe bronchus take-off (see Fig. 2.1, E ). The lingular bronchus courses obliquely in the anterior inferior direction for 2 to 3 cm and then gives rise to the superior and inferior segmental branches (see Fig. 2.1, F ). Because of the oblique cephalocaudad course of the lingular bronchus and its segmental branches, it may be difficult to clearly visualize them on axial CT.
The superior segmental bronchus of the left lower lobe originates within 1 cm of the origin of the left lower lobe bronchus and courses posteriorly and laterally (see Fig. 2.3 ). It arises from the left lower lobe bronchus at approximately the level of the lingular and right middle lobe bronchi. The basal segmental bronchi in the left lower lobe arise from the truncus basalis, which is visible inferior to the superior segment origin for a length of 1 to 2 cm. There are three basal segments in the left lower lobe: anteromedial, lateral, and posterior, which are situated from lateral to medial on the posteroanterior (PA) radiograph (see Fig. 2.1, H ).
There are many variants of the normal tracheobronchial branching pattern, most frequently within the subsegmental airways but also among the lobar and segmental bronchi. Most variations have been found to occur in the upper lobes. Although bronchial segmental branching variations occur commonly, the bronchopulmonary segments maintain a relatively consistent location.
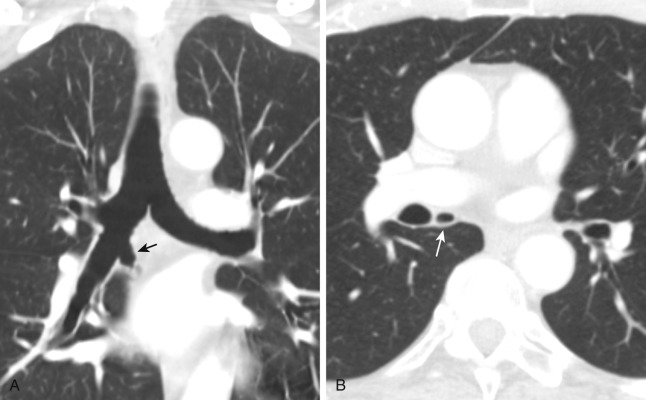
The tracheal bronchus was originally described as a bronchus to the right upper lobe arising from the trachea. More recently, the term tracheal bronchus has been used to refer to bronchial anomalies in which a bronchus supplying an upper lobe arises from either the trachea or a main bronchus. The majority of tracheal bronchi are located on the right and represent displaced rather than supernumerary bronchi. Tracheal bronchi to the right upper lobe typically arise from the right lateral tracheal wall within 2 cm of the carina and most frequently supply the apical segment ( Fig. 2.4 ).
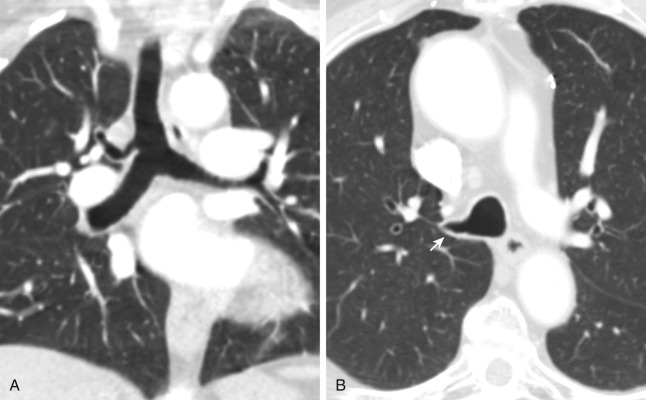
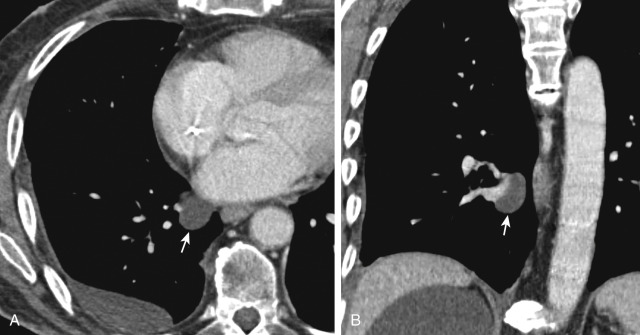
The accessory cardiac bronchus typically originates from the medial aspect of the bronchus intermedius or occasionally the right main bronchus and courses caudally, parallel to the bronchus intermedius, for 1 to 5 cm toward the heart or mediastinum ( Fig. 2.5 ). The incidence is about 0.1%. The majority of accessory cardiac bronchi are blind ending, although some terminate in small bronchioles, which may be associated with vestigial bronchiolar parenchymal tissue located in the azygoesophageal recess.
The main pulmonary artery arises from the pulmonic valve at the base of the right ventricle and passes superiorly, posteriorly, and to the left before bifurcating into the left and right pulmonary arteries ( Figs. 2.6 and 2.7, C ). The main, right, and left pulmonary arteries are located within the pericardium. The right pulmonary artery, which is longer than the left, courses to the right posterior to the ascending aorta before dividing in front of the right main bronchus into a right upper lobe branch, the truncus anterior , located anterior to the right upper lobe bronchus and the descending or interlobar pulmonary artery. The truncus anterior gives rise to segmental branches, which supply the right upper lobe. However, in many individuals, a separate branch originating from the interlobar artery supplies a portion of the right upper lobe posterior segment.
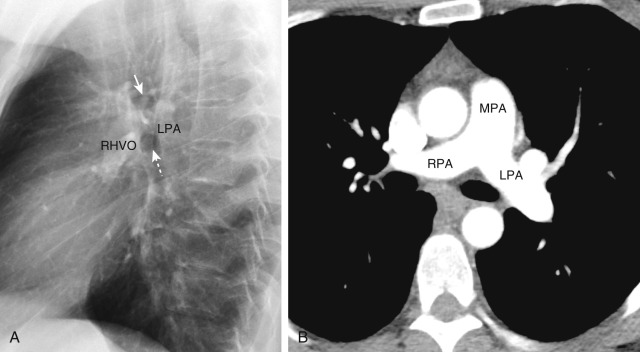
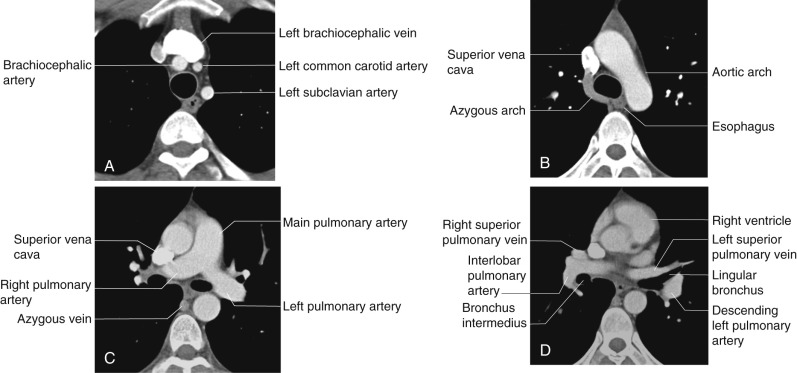
The right interlobar artery is located anterior and lateral to the bronchus intermedius and posterior to the right superior pulmonary vein ( Fig. 2.7, D ). The right middle lobe pulmonary artery arises from the interlobar artery and courses laterally, parallel to the right middle lobe bronchus. The right lower lobe pulmonary artery is directed perpendicular to the axial scan plane on CT at this level and can be seen as an ovoid structure at the level of the right middle lobe artery origin. The basilar segmental pulmonary arteries in the right lower lobe are located posterolateral to the associated basilar segmental bronchi.
The higher left pulmonary artery passes over the left main bronchus (see Fig. 2.6 ). It can give rise to a separate branch to the left upper lobe but more commonly continues directly into a vertical left interlobar or descending pulmonary artery, which directly gives to rise to segmental branches in the left upper and lower lobes. At the level of the lingular bronchus, the left interlobar artery is located lateral to the lower lobe bronchi and posterolateral to the lingular bronchus (see Fig. 2.7, D ). The basilar segmental arteries in the left lower lobe are located posterolateral to the basilar bronchi, as in the right lower lobe.
The pericardial recesses appear as fluid attenuation structures on CT, which exhibit minimal or no mass effect on adjacent structures. The transverse sinus and oblique sinus are the two major pericardial sinuses, each of which gives rise to several recesses.
The transverse sinus is situated superior to the left atrium and posterior to the ascending aorta and pulmonary trunk. There are four recesses within the transverse sinus: the superior and inferior aortic recesses and the right and left pulmonic recesses.
The superior aortic recess is the most superior component of the transverse sinus, and it can extend along the right aspect of the ascending aorta. The anterior aspect of the recess insinuates between the ascending aorta and pulmonary trunk. The posterior division of the superior aortic recess, also denoted the superior pericardial recess, is typically visible as a crescentic fluid collection approximating the posterior aspect of the ascending aorta, just above the right pulmonary artery ( Fig. 2.8 ). In some individuals, a “high-riding” superior pericardial recess may extend to the right paratracheal space and can be mistaken for lymphadenopathy or a cystic mediastinal lesion.
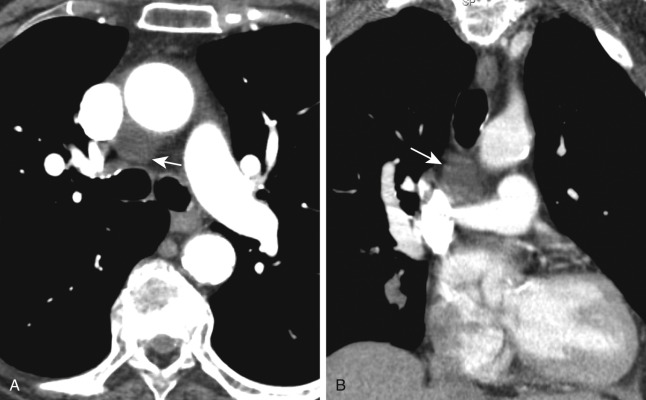
The left pulmonic recess is located inferior to the left pulmonary artery and is usually seen on CT as a crescentic or triangular fluid-attenuation structure paralleling the proximal right pulmonary artery (see Fig. 2.8 ). As with the superior aortic recess, the left pulmonic recess may have a round configuration and can be mistaken for lymphadenopathy.
The oblique pericardial sinus is posteriorly located within the pericardial space. It is situated anterior to the esophagus and posterior to the left atrium, approximating the subcarinal space. Fluid within the oblique sinus can mimic esophageal abnormalities or subcarinal lymphadenopathy.
The right and left pulmonary venous recesses and the postcaval recess originate from the pericardial cavity proper. The postcaval recess is located posterior to the superior vena cava (SVC). The right and left pulmonary venous recesses are situated between the superior and inferior pulmonary veins on their respective sides. Fluid distending the right pulmonary venous recess may have a lobulated appearance and can also mimic lymphadenopathy ( Fig. 2.9 ).
The lobes of the lungs are separated by fissures, bounded by the visceral pleura. The majority of fissures are incomplete. On the lateral projection, the major fissures course from superior to inferior, from the fifth thoracic vertebra to the diaphragm, roughly paralleling the sixth rib. The entire length of the major fissures is not usually visible. Above the hila, the medial portions of the major fissures lie more anteriorly than the lateral portions, and below the hila, the lateral portions of the major fissures lie more anteriorly. The major fissure is usually not visible on the frontal projection. However, the superolateral major fissure can occasionally be seen when extrapleural fat enters the edge of the fissure where it contacts the posterior chest wall. It forms a curved line on the frontal radiograph that starts medially above the hilum and curves downward and laterally.
The minor fissure extends anteriorly and laterally from the right hilum to the lateral chest wall and separates the anterior segment of the right upper lobe from the middle lobe. It is seen in at least half of patients on the frontal view. The fissure terminates medially at the right interlobar artery. On the lateral radiograph, the posterior extent of the minor fissure can occasionally project posterior to the hilum and major fissure.
Accessory fissures can be found in up to 30% of patients and may occur between any segments. Such fissures are frequently incomplete and vary with the degree of development. The common accessory fissures include the azygous fissure, inferior accessory fissure, superior accessory fissure, and left minor fissure.
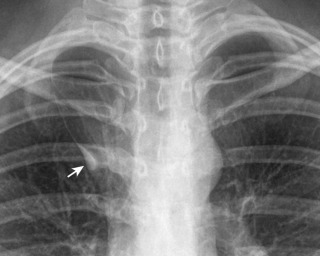
The azygous fissure is formed by the downward invagination of the azygous vein through the apical right upper lobe. It creates a curvilinear reflection composed of four pleural layers extending obliquely from the upper aspect of the right lung and terminating in a teardrop shadow, which is formed by the azygous vein above the right hilum ( Fig. 2.10 ). The azygous lobe is the portion of the right lung located medial to the fissure.
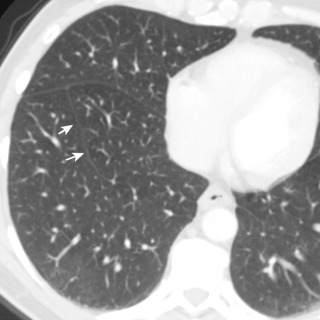
The inferior accessory fissure separates the medial basal segment from the remaining lower lobe segments and may occur on the right or left. The fissure extends from the inner third of the hemidiaphragm superiorly and slightly medially ( Fig. 2.11 ). It is visible in up to 16% of individuals on chest CT.
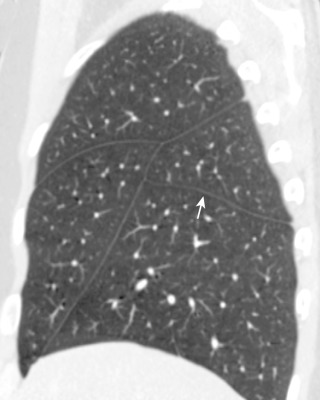
The superior accessory fissure divides the superior segment from the lower lobe basal segments. It is more frequent on the right and located in a horizontal plane similar to that of the right minor fissure ( Fig. 2.12 ).
The left minor fissure divides the lingua from the superior division of the left upper lobe ( Fig. 2.13 ). The left minor fissure is typically more superiorly located than the right.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here