Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Biliary tract neoplasms include tumors in the bile ducts and gallbladder. Although they are infrequent, most neoplasms that arise from the gallbladder and bile ducts are malignant, resulting in poor prognosis. Gallbladder carcinoma is the seventh most common malignancy of the gastrointestinal tract and is the most common biliary malignancy; bile duct carcinoma occurs less often. Familiarity with the imaging characteristics of gallbladder and bile duct neoplasms is important to expedite diagnosis and appropriate treatment of patients who often present with nonspecific symptoms of right upper quadrant pain, jaundice, and weight loss.
Gallbladder cancer is the sixth most common cancer of the digestive system and accounts for 3%–4% of all gastrointestinal cancers. Carcinoma of the gallbladder accounts for 1.7% of all global cancer death. Carcinoma of the gallbladder is two to three times more common in women than in men, and its incidence steadily increases with age, although it varies greatly in different parts of the world. More than 90% of patients are older than 50 years; the peak incidence is 70–75 years. Some geographic areas have a high incidence of gallbladder cancer, including South America, India, and Eastern Asia. Incidence of gallbladder cancer was higher in certain groups including Americans natives, Alaskan natives, and Hispanics in the United States than other populations. ,
Several risk factors of developing gallbladder carcinoma have been reported. The presence of gallstones is considered to be an important risk factor for gallbladder carcinoma. Of patients with gallbladder carcinoma, 65%–90% have gallstones, an incidence considerably higher than that for age- and sex-matched control groups. , Gallbladder cancers are often incidentally found during surgery for gallstones or on final histologic analysis of the specimen. Hyalinizing cholecystitis, known as incomplete porcelain gallbladder, is another predisposing factor, ranging from 12% to 61%, whereas gallbladder with diffuse wall calcification is less related with carcinoma. Other risk factors include the presence of gallbladder adenomas, an anomalous pancreaticobiliary duct junction, primary sclerosing cholangitis (PSC), exposure to carcinogenic chemicals, and obesity.
Approximately 70% of carcinomas originate in the fundus, followed by body and neck. In some cases, the tumor may diffusely infiltrate the entire gallbladder, making its origin impossible to identify. Macroscopically, carcinomas of the gallbladder can appear as poorly defined areas of diffuse/focal gallbladder wall thickening (infiltrating) or a polypoid mass that grows into the gallbladder lumen. The infiltrating type invades and infiltrates the gallbladder wall and ultimately replaces the lumen with a mass of tumor. The papillary form grows into and eventually fills the lumen. Some tumors may show a combination of the infiltrating and fungating patterns. Histologically, most gallbladder cancers are adenocarcinoma (85%–90%), and the remaining tumors belong to other subtypes, including clear cell carcinoma, squamous or adenosquamous carcinoma, sarcomatoid carcinoma, or poorly cohesive carcinoma with or without signet ring cells.
The gallbladder has a unique anatomic feature: the wall consists of a mucosa, a lamina propria, a smooth muscle layer, perimuscular connective tissue, and serosa without a submucosa. Furthermore, no serosa exists at the attachment to the liver and along the hepatic surface. The connective tissue is continuous with the interlobular connective tissue of the liver. Gallbladder carcinoma is staged surgically by the depth of invasion, the extension of disease into adjacent structures, the involvement of lymph nodes, and the presence of metastases using the American Joint Committee on Cancer TNM staging system ( Table 50.1 ). Invasion of the muscularis mucosa distinguishes T1 from T2 cancers.
| Primary Tumor (T) | |
| Tis | Carcinoma in situ |
| T1a | Limited to the lamina propria |
| T1b | Invades the muscle layer |
| T2a | Invades the perimuscular connective tissue on the peritoneal side |
| T2b | Invades the perimuscular connective tissue on the hepatic side |
| T3 | Perforates the serosa and/or directly invades the liver and/or other adjacent organs or structures (stomach, duodenum, colon, pancreas, omentum, or extrahepatic bile ducts) |
| T4 | Invades the main portal vein or hepatic artery or two or more extrahepatic organs or structures |
| Regional Lymph Nodes (N) | |
| N0 | No regional metastasis |
| N1 | Metastasis in 1–3 regional lymph nodes |
| N2 | Metastasis in ≥ 4 regional lymph nodes |
| Distant Metastasis (M) | |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
| Stage Group | |
| 0 | TisN0M0 |
| I | T1N0M0 |
| IIA | T2aN0M0 |
| IIB | T2bN0M0 |
| IIIA | T1N1M0, T2N1 M0, T3N1M0 |
| IIIB | T4N0M0, T4N1M0 |
| IVA | Any T, N2M0 |
| IVB | Any T, Any N, M1 |
Early-stage gallbladder carcinomas do not have specific symptoms and cancer is often found incidentally. If patients with gallbladder cancer have symptoms, then there is a high probability to observe advanced stage of gallbladder cancer. Abdominal pain is the most common symptom of gallbladder cancer followed by nausea and vomiting, jaundice, anorexia, and weight loss. Patients may have long-standing symptoms of chronic cholecystitis with a recent change in the quality or frequency of the painful episodes. Other common presentations are similar to either acute cholecystitis or symptoms of biliary malignancy. Elevated serum levels of carbohydrate antigen 19-9 and carcinoembryonic antigen have been reported in association with gallbladder carcinoma.
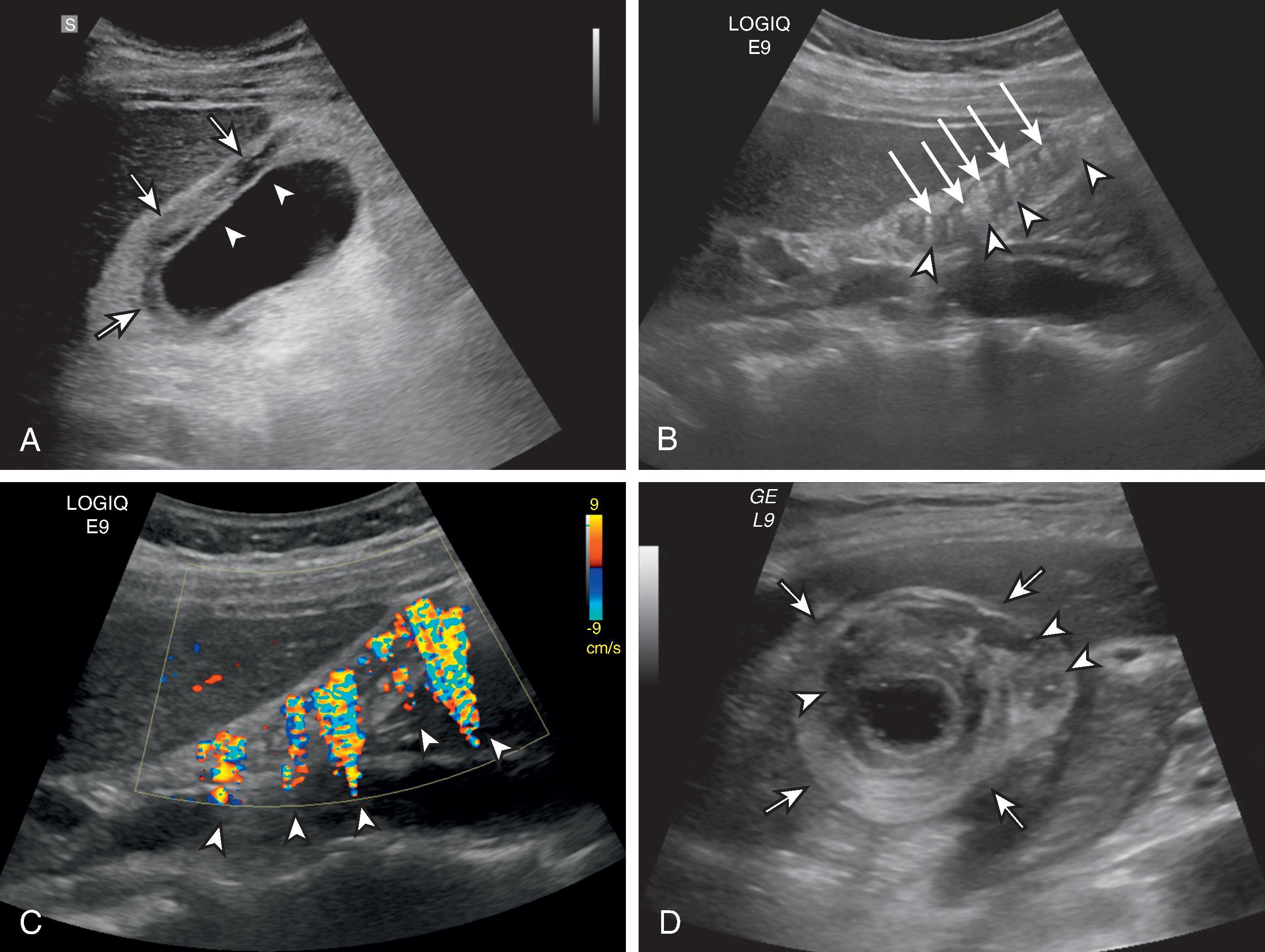
Ultrasound (US), computed tomography (CT), and magnetic resonance imaging (MRI) are valuable imaging modalities for evaluating patients with gallbladder carcinoma. US is recommended as an initial examination because it can detect suspicious lesions for gallbladder carcinoma such as a polyp with a wide base, irregular borders, vascular stalks, or wall thickening of more than 3 mm. The diagnostic accuracy of US in gallbladder cancer is over 80%. , US including Doppler is also useful for excluding benign lesions such as adenomyomatosis, non-neoplastic polyps, or tumefactive sludge by demonstrating intramural cystic spaces and/or echogenic foci within the wall, comet-tail artifact.
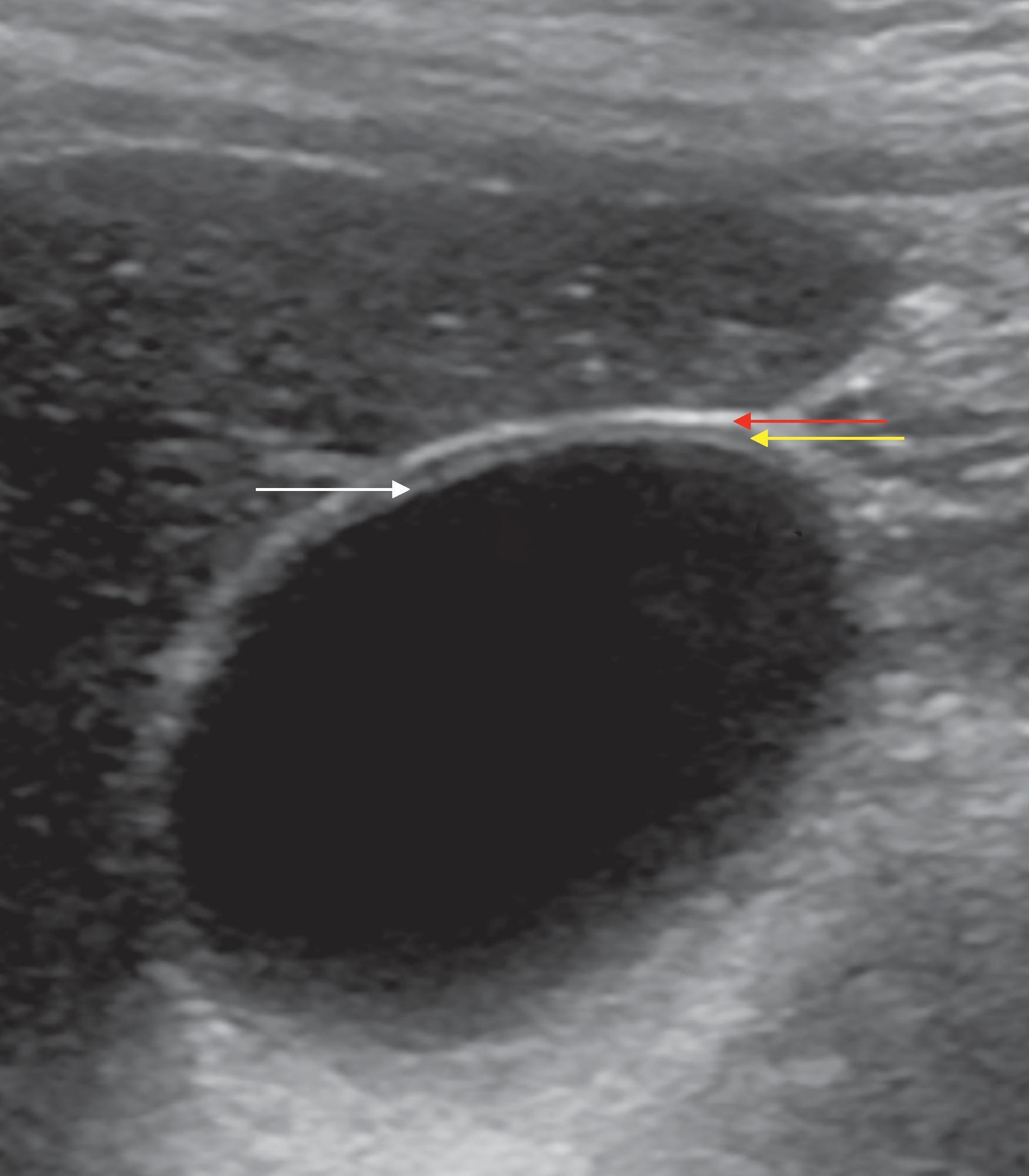
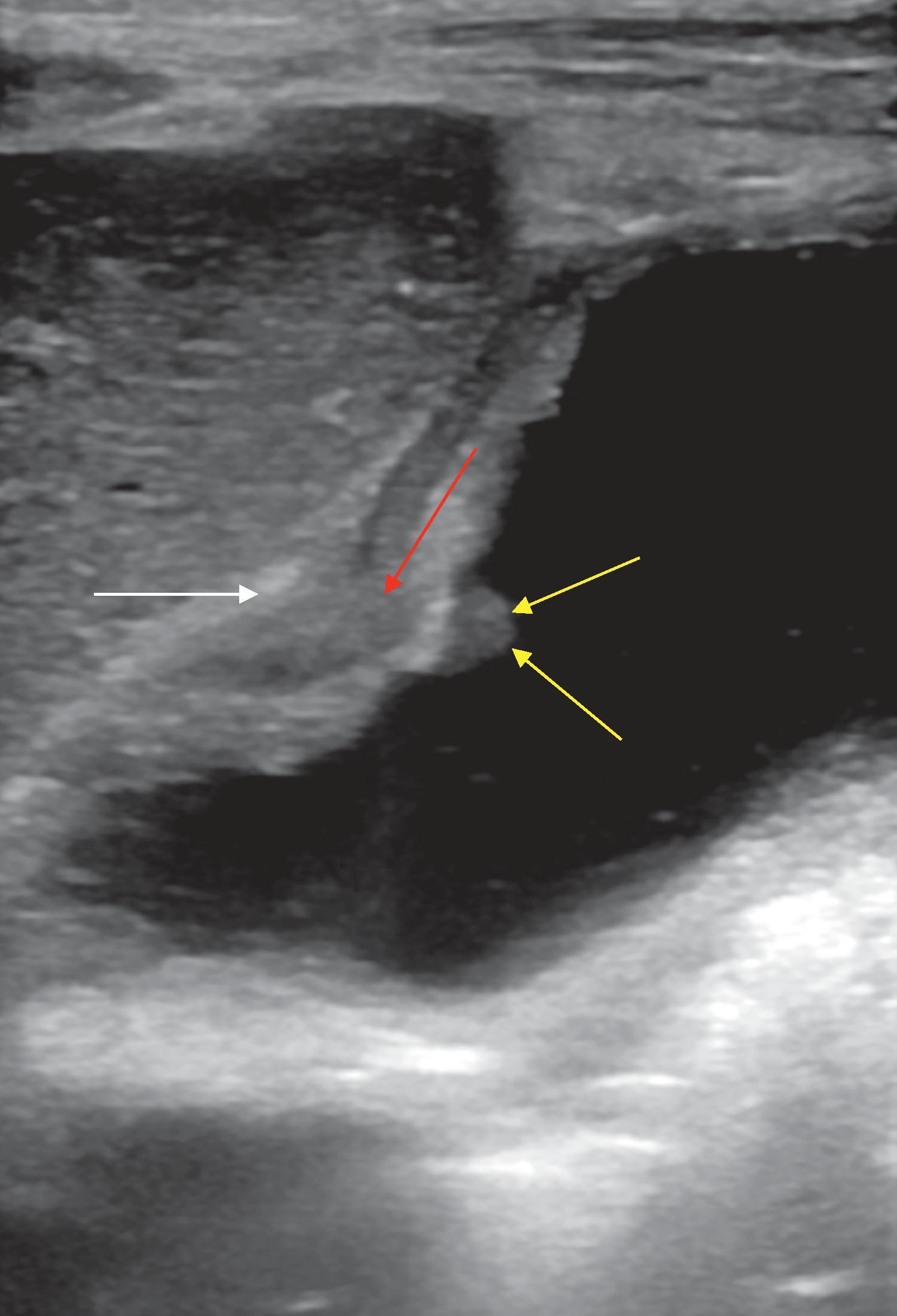
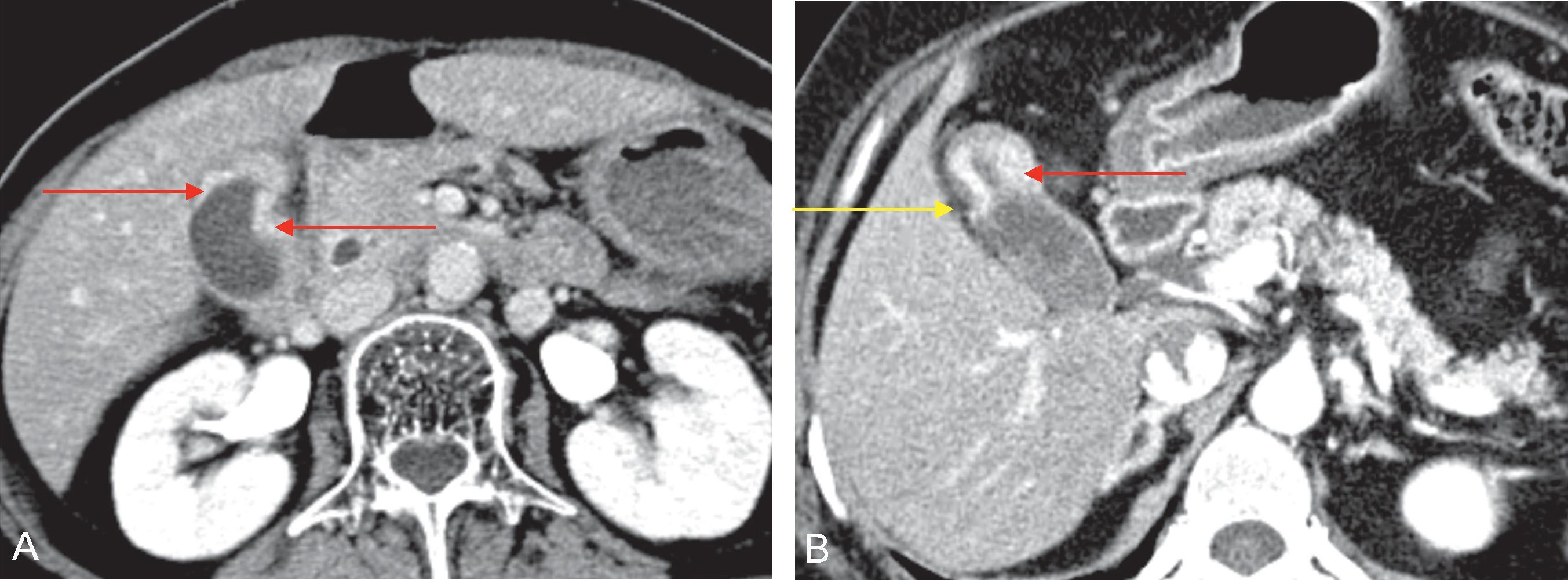
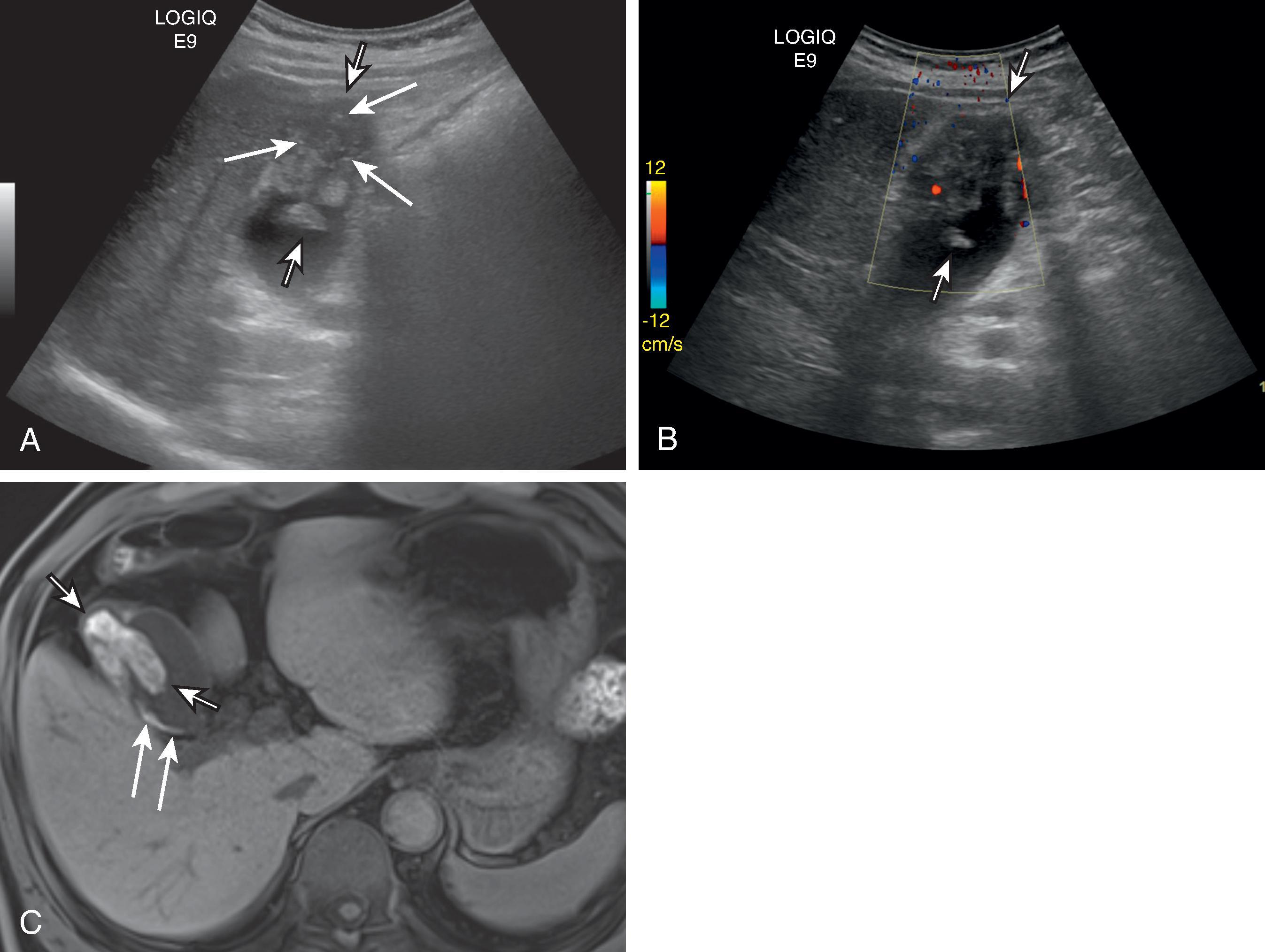
In patients with gallbladder carcinoma, endoscopic US and “high-resolution” US (HRUS) are useful in T-staging. HRUS uses both low- and high-frequency transducers (3–7 MHz) in order to better visualize gallbladder walls and intralesional echogenicity ( Fig. 50.1) . In patients with gallbladder carcinoma, perimuscular tissue involvement can be demonstrable in US, which determines surgical extent , ( Fig. 50.2 ). However, US has a limitation for evaluation of metastasis and is sometimes suffered from a limited sonic window. Instead, CT and MRI are able to assess lymphadenopathy and spread of the disease into the liver, porta hepatis, or adjacent structures. Furthermore, in patients with limited sonic window due to bowel gas or stones, or not eligible for endoscopic US due to previous surgery, CT and MRI can be used for local staging since large tumors (≥10 mm) can be easily demonstrated in CT or MRI. In patients with suspicion of metastasis, 2-deoxy-2-[F-18]fluoro-D-glucose-positron emission tomography (FDG-PET) will be helpful as well. These cross-sectional imaging tests are useful in predicting which patients will benefit from surgical resection. In addition, gallbladder carcinoma often spreads along the bile ducts in the lesser omentum. MRI with MR cholangiopancreatography (MRCP) provides more detailed information regarding biliary involvement of the tumor than US or CT and determines the surgical extent in advanced stage. Conventional radiography, traditional plain oral cholecystography, and barium studies of the gastrointestinal tract have a limited role in the imaging of gallbladder carcinoma in terms of detection, differential diagnosis, and cancer staging. Although direct cholangiographic techniques such as endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangiography are of little value in the diagnosis of gallbladder cancer, they are helpful in alleviating symptoms in patients with jaundice.
Gallbladder carcinomas have three major morphologic presentations: (1) focal or diffuse thickening and/or irregularity of the gallbladder wall; (2) polypoid masses originating in the gallbladder wall and projecting into the lumen; and (3) most commonly, a mass obscuring or replacing the gallbladder, often invading the adjacent liver.
Gallbladder carcinoma may cause mild to marked mural thickening in a focal or diffuse pattern. Although it is the least common presentation of gallbladder carcinoma, this is the most difficult to diagnose, particularly in the early stage. This mural thickening is best appreciated in US; the gallbladder wall usually is 3 mm or less in thickness. Pronounced wall thickening (>1.0 cm) with associated mucosal irregularity or marked asymmetry should raise concerns for malignancy or complicated cholecystitis. Carcinomas confined to the gallbladder mucosa may present as flat or slightly elevated lesions with a mucosal irregularity that are difficult to identify at imaging, which requires careful evaluation ( Fig. 50.3 ). In one sonographic series, half the patients with these early carcinomas had no protruding lesions and were identified preoperatively in less than one-third of patients. Advanced gallbladder carcinomas can cause marked mural thickening and wall deformity, often with heterogeneous echogenicity ( Fig. 50.4 ). The gallbladder may be contracted, normal sized, or distended, and gallstones are often present. When cancer occurs in the neck portion of the gallbladder, identification of cystic duct involvement by the tumor on imaging merits consideration of focal bile duct resection to achieve a negative resection margin.
Four factors interfere with the recognition of carcinoma as the cause of gallbladder wall thickening at US.
Minimal changes of early-stage carcinoma: changes of early gallbladder carcinoma may be subtle mucosal irregularity or mural thickening, which is frequently missed or not perceived in imaging.
Overlap with benign conditions: gallbladder wall thickening is a nonspecific finding that can also be caused by acute or chronic cholecystitis, adenomyomatosis, inadequate gallbladder distention, and other medical conditions such as portal hypertension, hepatitis, or renal failure.
Coexistence of benign condition: chronic cholecystitis is often present in patients with gallbladder carcinoma. Besides, acute cholecystitis can develop in patients with gallbladder carcinoma due to cystic duct obstruction.
Limited sonic window: shadowing stones or gallbladder wall calcification may obscure the carcinoma.
Early-stage carcinoma is still a challenge, but regular follow-up with HRUS in patients with suspicion may reduce the chance of misdiagnosis. Although there are some overlaps with benign condition, mucosal layer thickening rather muscular layer, mucosal discontinuity, and irregular border of lesion in US can be a clue for diagnosing gallbladder carcinoma early.
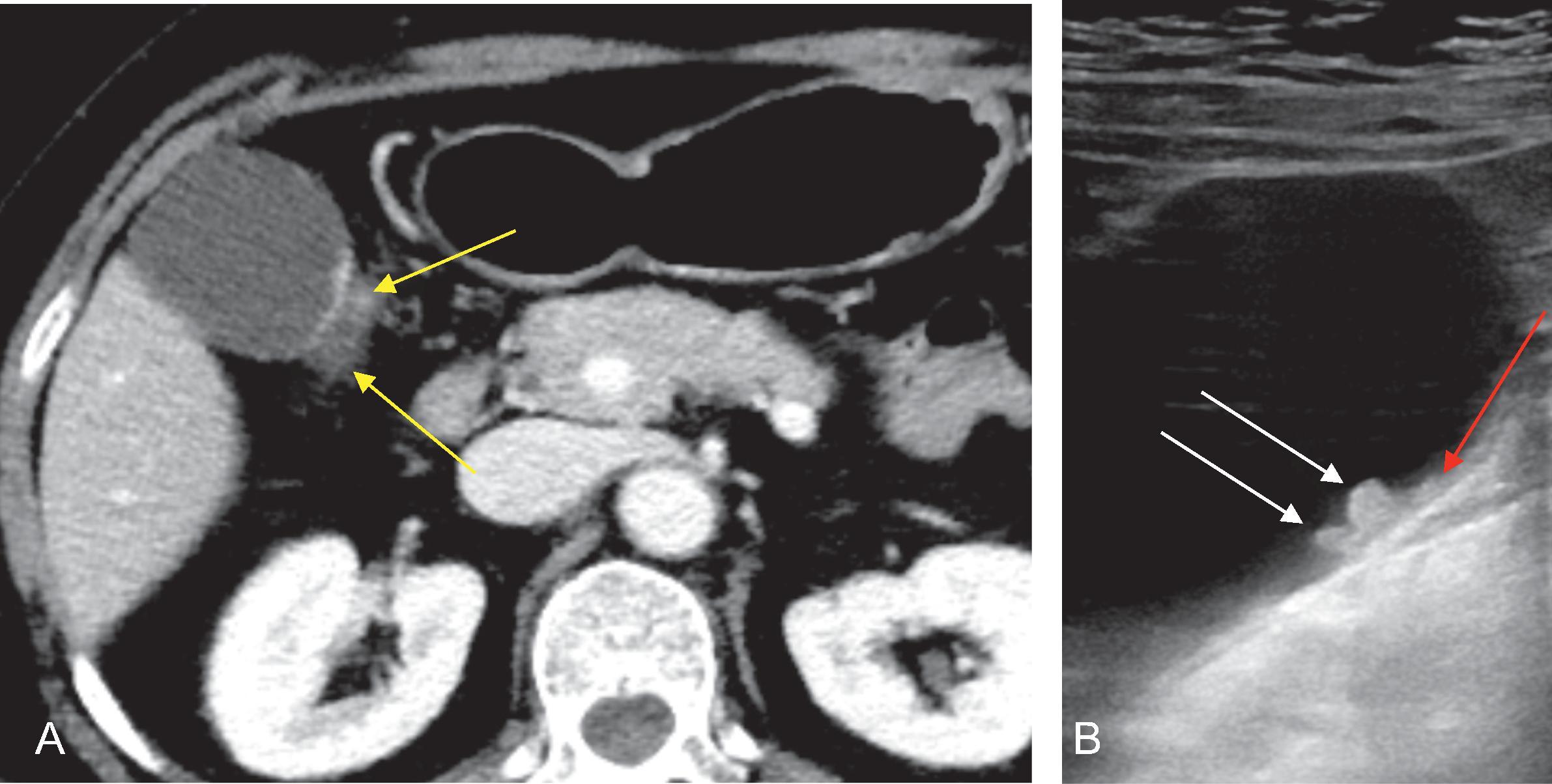
In patients with limited sonic window and those with indeterminate US findings, CT or MRI can be considered as a next step. CT and MRI can visualize thickened gallbladder wall, which is obscured by gallstones or mural calcifications in US. In CT and MRI, thick (>3 mm) and strong enhancement of the inner wall with hypoenhancing thin outer wall or diffuse transmural wall thickening with irregular contour are significant predictors for gallbladder carcinoma ( Figs. 50.4 and 50.5 ). , Intermediate high intensity on T2-weighted image and presence of diffusion restriction also suggest a high possibility of gallbladder carcinoma.
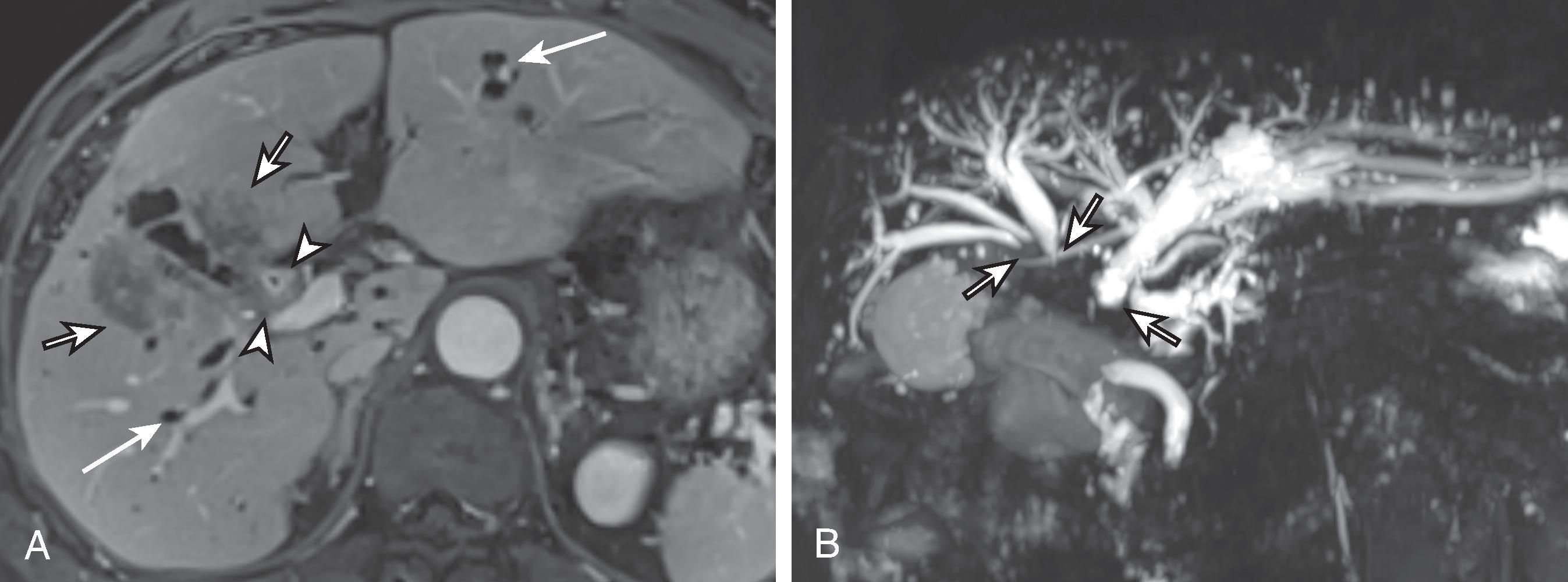
When focal or irregular thickening of the gallbladder wall is encountered in CT, the images should be carefully inspected for bile duct dilatation, liver invasion, lymphadenopathy, or metastasis. Multiplanar reformatted images of multidetector CT (MDCT) and MRI with MRCP are valuable for both local staging evaluation and distant metastasis detection ( Fig. 50.6 ). Recent studies reported better performance of MRI with MRCP for differentiating gallbladder carcinoma from benign wall thickening such as xanthogranulomatous cholecystitis (XGC) or adenomyomatosis than HRUS or in combination with HRUS. ,
Approximately one-fourth of gallbladder carcinomas manifest as a polypoid mass projecting into the gallbladder lumen. , Identification of these neoplasms is particularly crucial because they are well differentiated and are more likely to be confined to the gallbladder mucosa or muscularis when detected. ,
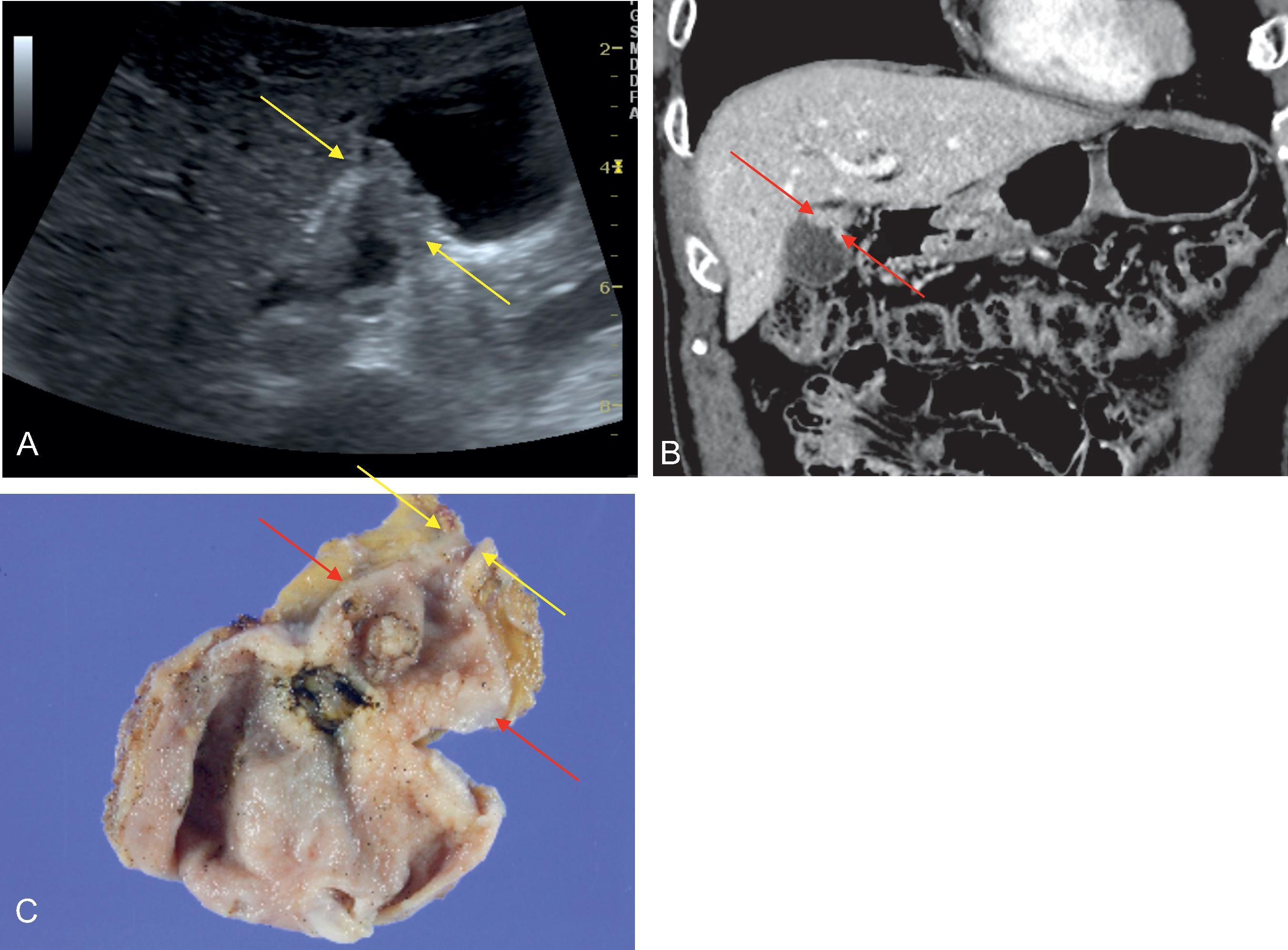
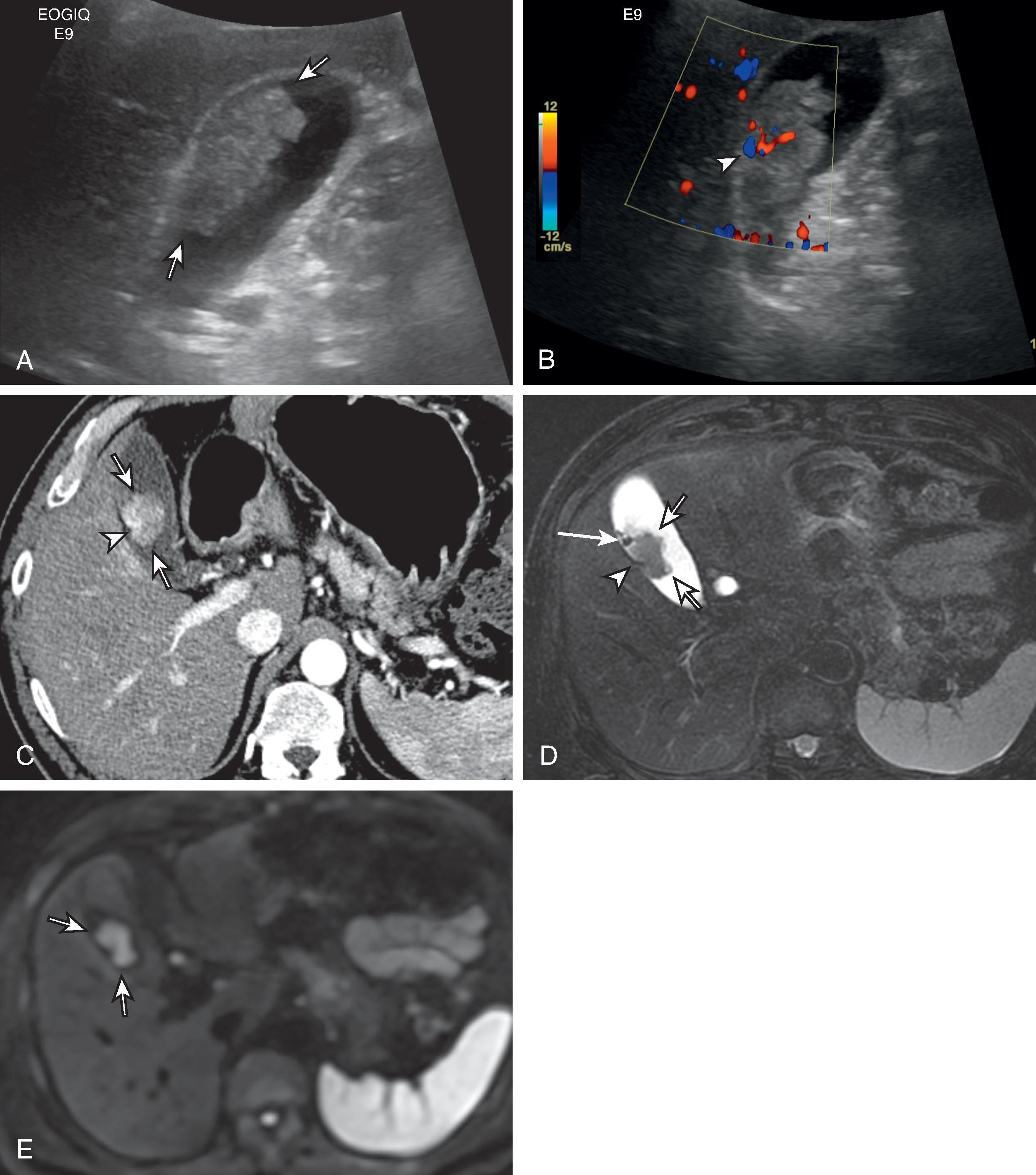
Polypoid carcinomas in US usually have a homogeneous tissue texture, are fixed to the gallbladder wall at their base, and do not cast an acoustic shadow ( Fig. 50.7 ). Although a small polypoid carcinoma can be indistinguishable from adenoma, cholesterol polyp, or tumefactive sludge, some US features are helpful to diagnose neoplastic polyps including carcinoma with polypoid appearance: large size (≥10 mm), broad base, vascular stalk/intratumoral vascularity, papillary growth, and sometimes internal hypoechogenicity ( Figs. 50.7 and 50.8 ). Adjacent gallbladder wall thickening and the presence of gallstone will be a clue of gallbladder carcinoma ( Figs. 50.9 ). When polypoid carcinomas are sufficiently large, they manifest as soft tissue masses that are denser than surrounding bile in CT or show a hypointensity than surrounding bile in the T2-weighted image (see Fig. 50.8 ). Polypoid cancer usually enhances homogeneously after administration of contrast medium, and occasionally vascular stalk is visible (see Figs. 50.7 and 50.8 ). Adjacent gallbladder wall may be thickened (see Figs. 50.7 and 50.8 ). Gallstones can be detected together.
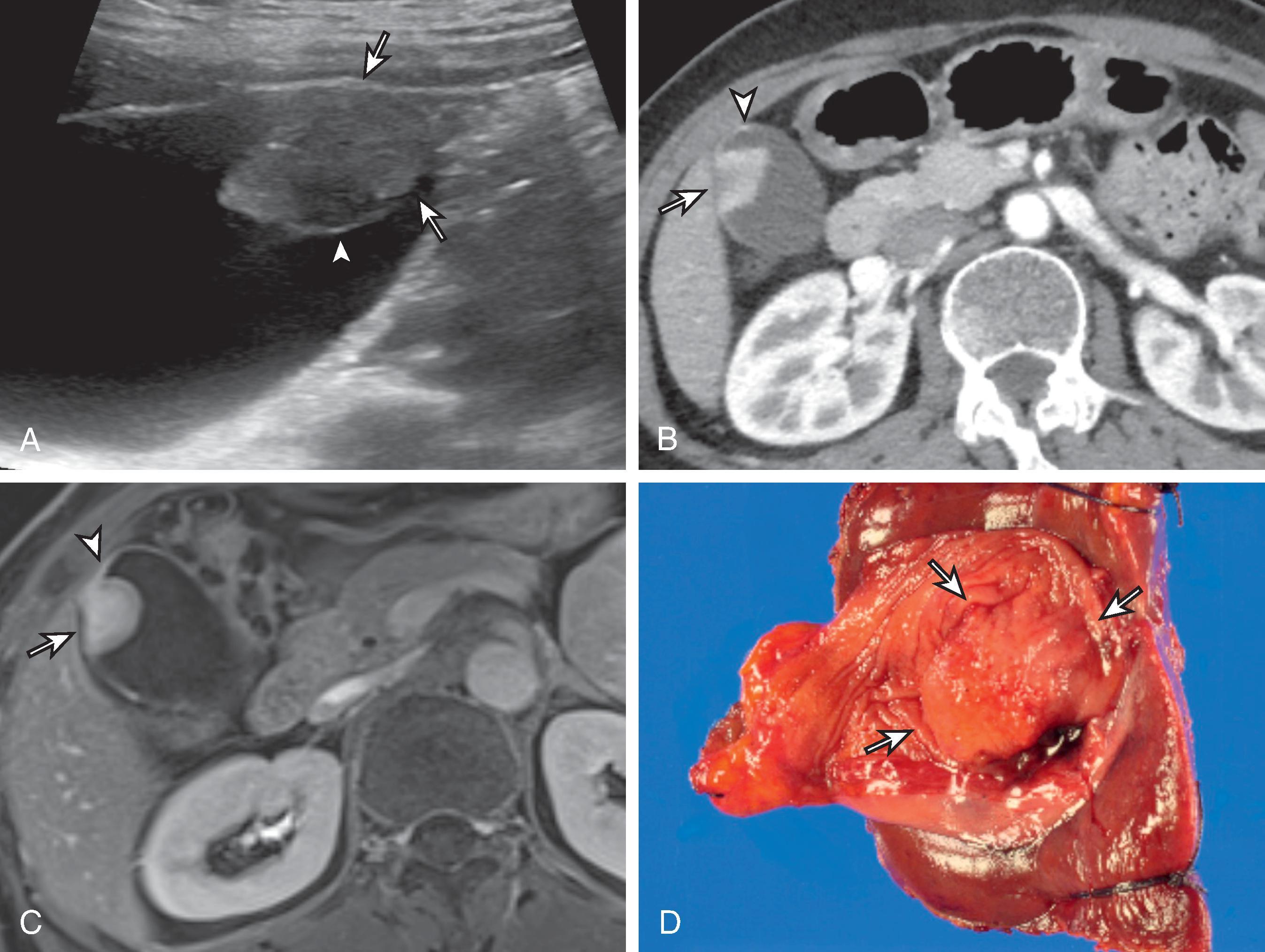
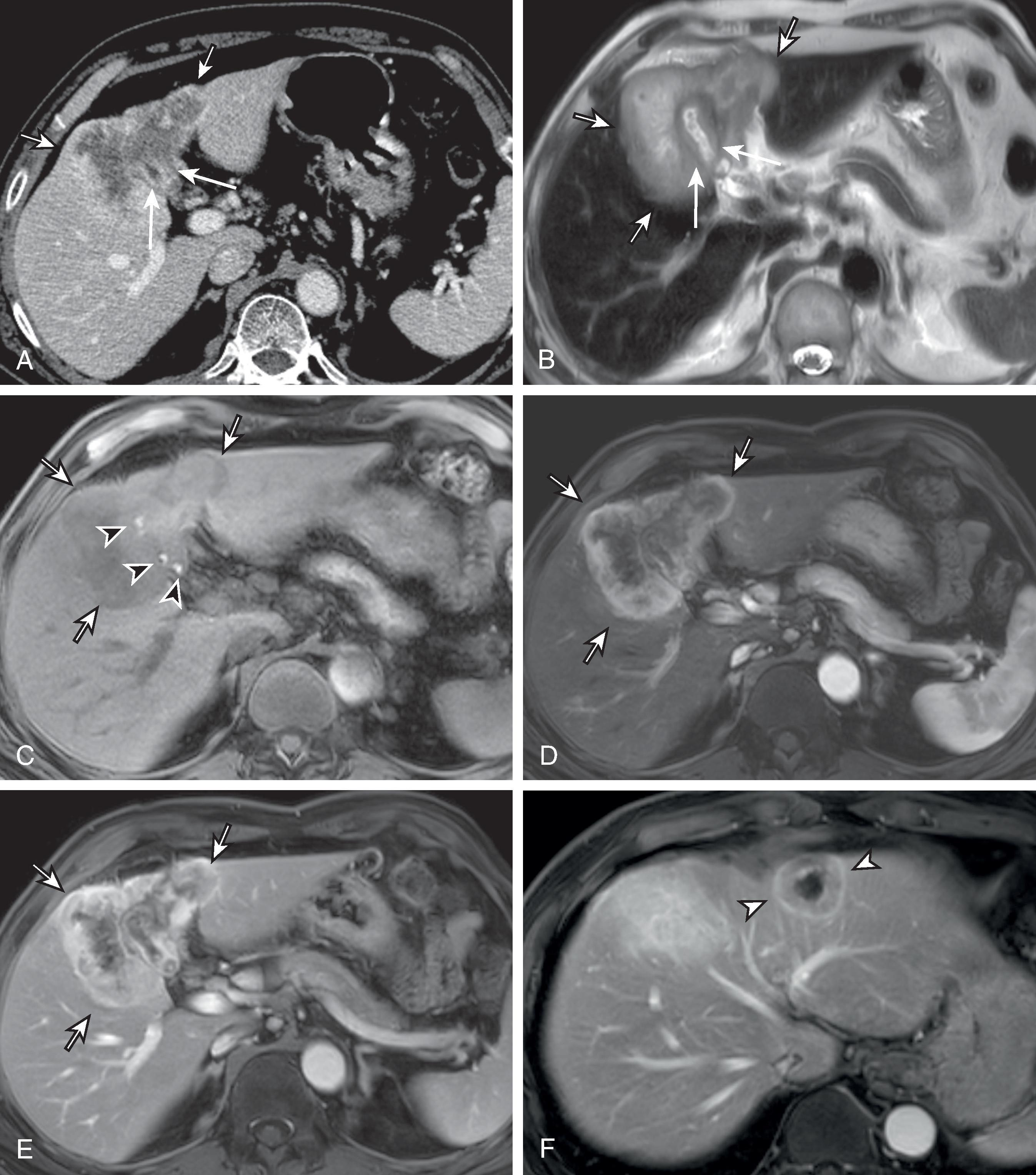
A large mass obscuring or replacing the gallbladder is the most common (40%–65%) presentation of gallbladder carcinoma. The mass often shows complex echogenicity in US due to tumor heterogeneity and internal necrosis. Gallstones are commonly seen within the ill-defined mass, which typically invades hepatic parenchyma. In CT, a large mass is in the liver parenchyma nearby the gallbladder fossa, or gallbladder wall thickening and the continuity with the mass are suggestive features of gallbladder carcinoma. Sometimes, the gallbladder is not seen, being replaced with the mass. This type of gallbladder carcinoma often shows lobulated contour, rim arterial phase hyperenhancement (APHE), and heterogeneous contrast enhancement with scattered regions of internal necrosis in CT (see Fig. 50.9 ). Invasion of the hepatoduodenal ligament, bile duct dilatation, intrahepatic satellite nodules, and distant metastasis, including the liver, are common.
MRI findings in gallbladder carcinoma are similar to those reported with CT. Masses are heterogeneously hyperintense on T2-weighted images and rim APHE with peripheral washout on dynamic phase, targetoid appearance in the diffusion-weighted image (see Fig. 50.9 ). Gallstones and tumoral calcifications may coexist. Owing to the advanced stage, metastasis is often found synchronously (see Fig. 50.9 ).
The differential diagnoses of wall thickening type gallbladder carcinomas include acute or chronic cholecystitis, XGC, adenomyomatosis, and wall thickening related to various medical conditions. For differential diagnosis, intramural echogenicity in US is helpful , ( Fig. 50.10 ). In acute cholecystitis, the wall often has irregular, discontinuous hypoechoic and echogenic bands. Chronic cholecystitis often results in uniformly thickened wall and collapsed lumen with stones. Wall thickening due to medical conditions generally shows wall edema of hypoechoic central band (see Fig. 50.10 ). Adenomyomatosis shows intramural echogenic spots and intramural cysts with intact mucosa, and comet-tail or twinkling artifact in US (see Fig. 50.10 ). XGC can show substantial mural thickening and multifocal intramural hypoechoic area or hypoechoic band with intact mucosa. Intramural hyperechoic spots can be observed (see Fig. 50.10 ). Adenomyomatosis and XGC can show typical appearance in CT or MRI, such as a pearl necklace sign or cotton ball sign of adenomyomatosis and intramural fat of XGC , , , ( Fig. 50.11 ). Complicated cholecystitis or adenomyomatosis may reveal low-attenuating intrahepatic halo surrounding the gallbladder wall in CT. , ,
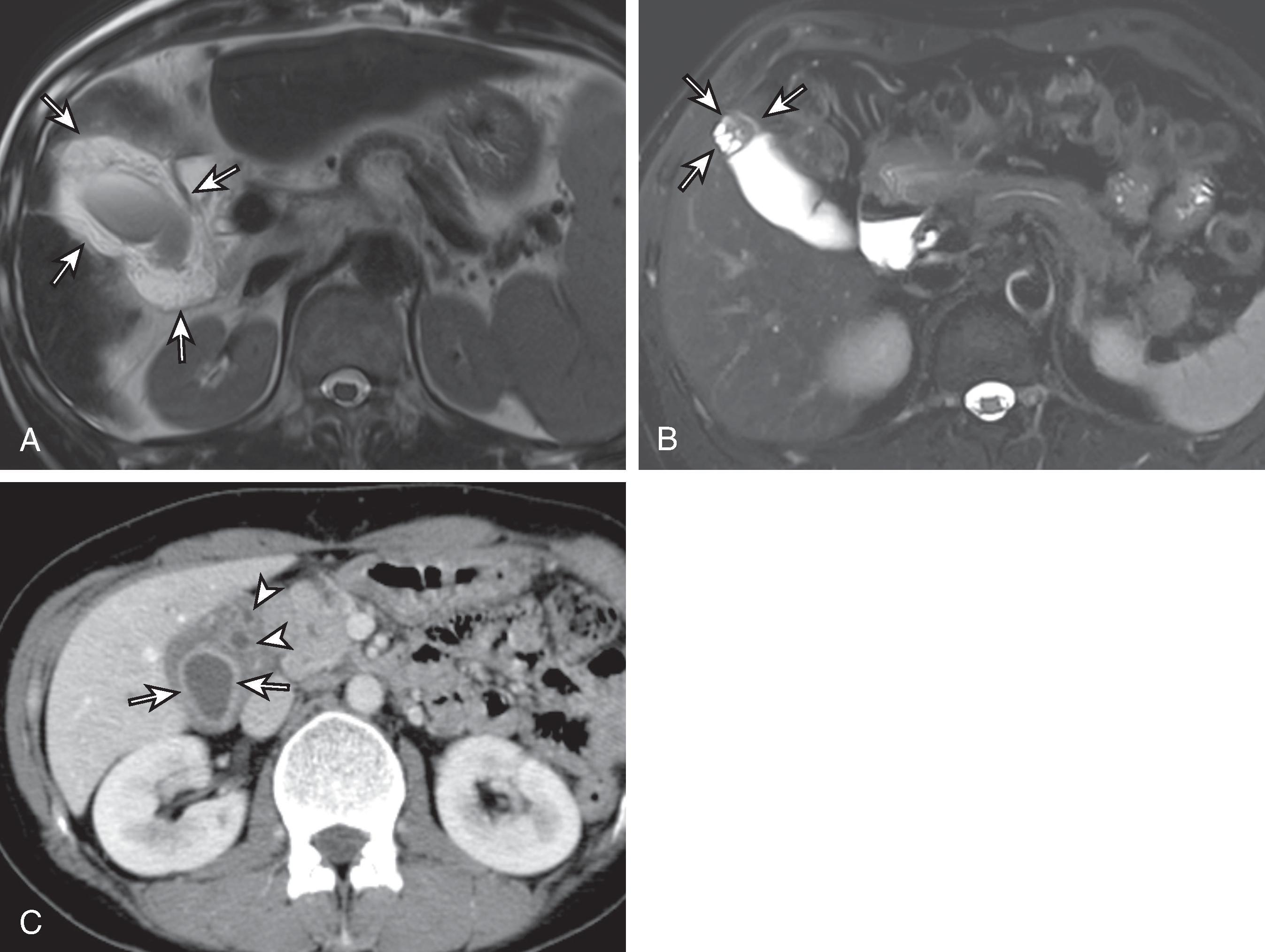
The differential diagnosis of tumors that present as an intraluminal polypoid mass includes tumefactive sludge, pseudotumoral polyps, adenoma, neuroendocrine tumor (NET) or metastasis. Tumefactive sludge presents as an intraluminal mass without posterior shadowing, fluid level, and movability unlike other biliary sludge. One differential point is that tumefactive sludge does not have internal vascularity, whereas gallbladder neoplastic polyps often show internal vascularity. And further, internal hyperechogenicity suggests the possibility of tumefactive sludge rather than accompanying malignancy. In addition, tumefactive sludge occasionally shows slow gravity dependence on follow-up US. CT and MRI help differentiate tumefactive sludge from carcinoma ( Fig. 50.12 ). The most common pseudotumor is cholesterol polyp that is usually small (<1 cm), multiple, and often shows posterior hyperechoic comet-tail artifact. Internal hyperechogenic spots with reverberation artifacts are observed in a large cholesterol polyp.
Furthermore, a mass replacing the gallbladder fossa includes hepatocellular carcinoma (HCC), cholangiocarcinoma (CCA), and metastatic disease to the gallbladder fossa. HCC occurring near the gallbladder fossa may be confused with gallbladder cancer radiographically, but they usually occur in cirrhotic livers, show non-rim APHE, and do not typically invade the gallbladder. Patients with liver metastases to the gallbladder fossa usually have a known primary neoplasm. Regardless of gross tumor type, gallbladder carcinoma should be suspected when there are features of a focal mass, lymphadenopathy, hepatic metastases, and biliary obstruction at the level of the porta hepatis, especially in old-age patients.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here