Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Significant injuries to the cerebral vessels can occur as a result of blunt or penetrating trauma to the neck.
Blunt trauma to the neck can lead to immediate or delayed ischemic strokes, and a low threshold for imaging vessels when neurologic findings or risk factors for cervical vessel injury exist is recommended.
A no-zone approach to penetrating neck trauma is becoming widely accepted as opposed to a zone-based selective management algorithm.
Multidetector CT angiogram is the initial imaging modality of choice in essentially all symptomatic cases of blunt or penetrating neck trauma.
Both penetrating and blunt neck injuries can present with minimal to no initial signs of injury; a high index of suspicion is therefore required.
Because of the paucity of neck trauma in children, many adult algorithms have been adopted for use in the pediatric population
Penetrating neck injuries (PNIs) comprise 5% to 10% of all traumatic injuries, but represent less than 1% of admissions to the emergency department (ED). Penetrating neck trauma carries a mortality rate of up to 10%. This is primarily a condition of adults; penetrating neck trauma in the pediatric patient is fortunately an uncommon entity. Of all children entered in the 2008 to 2012 national trauma data bank, only 0.3% sustained PNI with an average age just under 8 years and a predominance of male victims (70%). In this study, 44% of the injuries were caused by knives and 24% by firearms. Aerodigestive injury is most common followed by vascular injury in children below age 11 years. In the 11 to 14-year group, this ratio reverses with vascular injuries being most common. Mortality rates are reported at 5.6%.
Blunt neck trauma can injure the airway, pharyngoesophageal (PE) tract, nerves or glandular tissue, but the primary concern with blunt neck trauma involves blunt cerebrovascular injury (BCVI) to the carotid or vertebral artery. The incidence of BCVI in blunt trauma is 1%; however, 53-79% of patients are asymptomatic at presentation. Therefore, asymptomatic patients with high-risk injuries require screening.
The neck is defined as the area extending from the skull base to the T1 vertebral body and is separated by the superficial and deep (prevertebral) cervical fascia. The latter surrounds the perivertebral muscles and delineates the retropharyngeal space. The superficial fascia lies between the skin and platysma muscle. Immediately deep to the platysma is the deep cervical fascia , which comprises four separate layers: pretracheal, investing, and prevertebral layers as well the carotid sheath. The investing layer runs circumferentially around the entire neck just deep to the platysma. It splits to encase the trapezius and sternocleidomastoid muscles. The prevertebral fascia (deep to the investing layer) extends from the neck to the thorax, while encircling the cervical spine and prevertebral muscles. The pretracheal fascia completely surrounds the infrahyoid muscles, esophagus, trachea and thyroid gland. This layer inserts on the hyoid and thyroid cartilages above and the anterior pericardium below, while coursing deep to the sternum. It has clinical significance because it provides continuity from the neck to the mediastinum, meaning that spillage from neck wounds, in particular those involving the esophagus, can result in mediastinitis. The carotid sheath is comprised of all three layers of the deep cervical fascia. Within the sheath is found the internal or common carotid artery, the jugular vein, and vagus nerve.
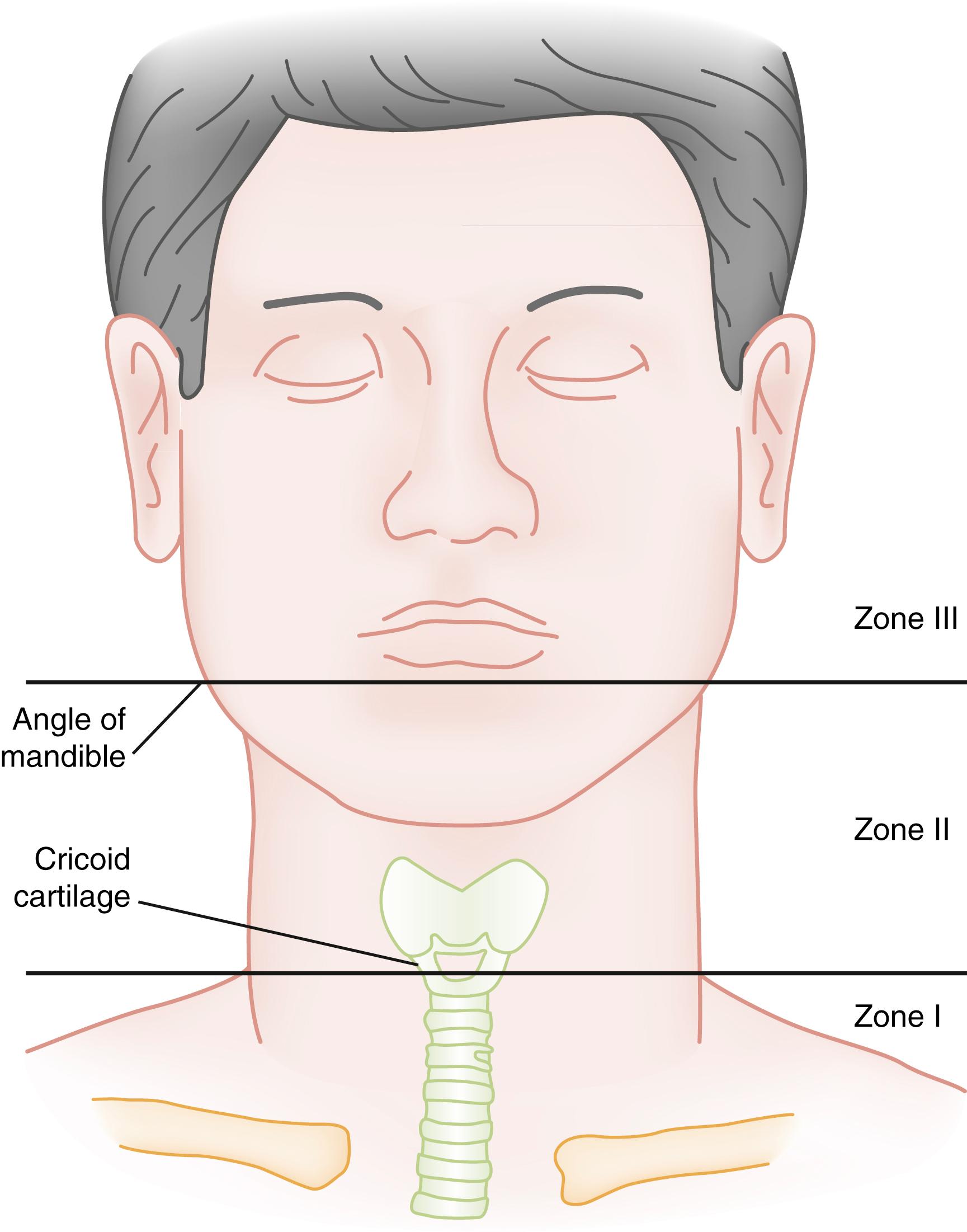
The neck has traditionally been divided into three zones. Zone 1 extends from the sternal notch to the cricoid cartilage, zone 2 from the cricoid cartilage to the angle of the mandible, and zone 3 from the angle of the mandible to the skull base ( Fig. 36.1 ). This distinction was largely predicated on the principal that zone 2 is the most commonly injured, has the highest mortality, and is most amenable to surgical exploration. However, widespread use of computed tomography angiogram (CTA) has made evaluation of this area possible without surgical exploration, rendering these distinctions less relevant, although important for communication among consultants. Furthermore, particularly in the setting of penetrating trauma, injuries often span multiple zones, and the most significant injury may lie in a different zone than the point of entry.
The neck is also divided into an anterior and posterior triangle. The anterior triangle is densely packed with vital structures including neurovascular and aerodigestive tracts. It is bordered anteriorly by the midline, posteriorly by the sternocleidomastoid muscle, and superiorly by the lower edge of the mandible. The posterior triangle is bound by the sternocleidomastoid muscle anteriorly, the clavicle inferiorly, and the anterior border of the trapezius muscle posteriorly. Excluding spinal trauma, injury to the posterior triangle often has a more favorable prognosis because of the relative paucity of vital structures.
The left common carotid branches off the aortic arch and the right off the brachiocephalic trunk. The common carotids branch into the internal and external carotids just superior to the thyroid cartilage. The internal carotid passes through the carotid canal in the temporal bone before splitting into the anterior and middle cerebral arteries. Blunt injuries to the carotids occur when hyperextension-rotation mechanisms stretch the carotid over the lateral processes of the upper spine, with hyperflexion, or with a direct blow to the vessel intraorally or externally. Damage to proximal structures such as the petrous portion of the temporal bone around the carotid canal can also cause damage. The vertebral arteries run cephalad through the transverse foramina starting at C6, and through the foremen magnum. Injury occurs during damage to the transverse foramina, fractures or facet dislocations of the upper cervical vertebrae (C1 through C3), or from stretch and compression around the atlantoaxial and atlantooccipital joints. Injuries to either vessel can predispose the patient to an ischemic stroke from obstruction of arterial flow.
The esophagus extends from the cricoid cartilage to the stomach (T11) and measures approximately 25 cm in the adult. It is anatomically divided into three sections: cervical, thoracic and abdominal. Physical examination alone is unreliable in diagnosing esophageal injury, and a normal examination does not exclude aerodigestive injury.
The larynx runs from the base of the tongue to the trachea, and contains the thyroid, cricoid, epiglottis and paired arytenoid, corniculate, and cuneiform cartilages. The low incidence of tracheal injury likely stems from its protected position sandwiched in-between the sternum, mandible and spine.
The type of damage to the cervical vasculature differs according to the mechanism of injury. More than 90% of carotid injuries are caused by penetrating trauma, which can result in partial or complete vascular transection, puncture wounds, AV fistula or pseudoaneurysm by direct transection or penetration injury. In addition, the concussive pressure effect resulting from the release of kinetic energy into small, contained deep neck spaces surrounding the carotid is seen with high velocity projectiles and tissue destruction remote to the projectile trajectory is expected. Vascular wounds sustained from penetrating objects comprise anywhere from 10% to 25% of PNIs. The ratio of carotid to vertebral artery involvement is approximately 2:1. Carotid artery mortality rates range from 5% to 6% and it is the leading cause of immediate death in the setting of PNI due to exsanguination. Extracranial vertebral artery injuries are less common with an overall incidence of 3%.
Blunt trauma typically leads to vascular occlusion, dissection, and intimal flaps. Up to 30% of BCVI can be bilateral. Carotid injuries portend a 17% to 38% risk of mortality and 32% to 67% rate of morbidity. For vertebral injuries, these numbers are lower but still significant at 8% to 18% and 14% to 24%, respectively . Two populations with distinct epidemiology are the pediatric and geriatric age groups. In one study looking at blunt injury, 23% of patients above 65 years of age with low energy falls who met screening criteria for vascular injury (detailed in the following) were diagnosed with BCVI. On the other hand, in pediatric patients, the rate of BCVI was lower than adults (0.2%), but the rates of neurological morbidity (80%) and mortality (40%) were high if stroke occurs. Most BCVI injury in the pediatric age group occur in teens, with only 9% impacting pre-school aged children.
Penetrating PE injuries are rare, and most often involve the cervical segment. Of all penetrating trauma, less than 1% results in injury to the pharynx or esophagus. Gunshot wounds comprise 54% and stab wounds 46%. Mortality rates for penetrating esophageal trauma have been reported from 4% to 8%. Mortality rates climb significantly (exceeding 44%) when esophageal injuries occur in a trauma patient with multi-organ system involvement. Diagnostic and/or therapeutic delays exceeding 24 hours are strongly associated with increased mortality.
PE injuries are less common following blunt trauma, but still associated with high mortality. They occur in less than 1% of all blunt trauma and 5% of blunt neck trauma with a median age of 18 years. Ten percent of laryngotracheal (LT) injuries are associated with a concurrent PE injury. Falls followed by motor vehicle collisions (MVCs) are the most common mechanisms of injury, although assault is responsible for 12% of cases. Mortality in patients who survive greater than 24 hours is similar regardless of whether the mechanism was penetrating or blunt.
Penetrating LT injuries most commonly result from bullets and knives. This type of injury is less common than blunt airway trauma. Penetrating LT occurs in 1% to 6% of all PNIs. These injuries can be subtle, and thus require a high index of suspicion.
In blunt neck trauma, the thyroid cartilage typically encounters forces to the neck first, and is the most commonly injured, often due to direct compression or manual strangulation. Laryngeal injury has been reported with sports-related neck trauma, mainly in young men. Bicycle and scooter accidents are associated with posterior membranous tracheal wall injuries. The cricoid cartilage is the only complete circumferential ring stenting the larynx open, leaving a patient with substantial damage to this structure at risk of airway collapse. Because the cricoid cartilage is a complete ring, there are often two fracture sites at the anterior and posterior aspects. When LT separation occurs, typically, this is at the level of the cricothyroid membrane.
Hanging is a specific type of blunt injury. Judicial hangings of the past resulted in death from cervical fractures and cord transection. Modern-day suicidal hangings rely on the external force of the ligature, which causes venous congestion and leads to unconsciousness with resultant tightening of the noose, arterial occlusion, and cerebral hypoxia. Vagal reflexes resulting from pressure on the carotid body may contribute to fatal dysrhythmias as well as increasing sympathetic tone from pericarotid sinus pressure. Compression of the airway does not play as significant a role.
Signs and symptoms suggesting penetrating vascular injury have been divided into two main categories: hard and soft signs of injury ( Table 36.1 ). Differentiating between soft and hard signs in the setting of penetrating neck trauma is imperative. Hard signs are commonly seen with serious or life-threatening injuries and should prompt an immediate surgical consultation and operative intervention. Hard signs have been shown to have an 89.7% positive predictive value for the presence of vascular or aerodigestive injury. Soft signs of injury are less specific but suggest the potential for a serious injury and warrant further workup. Soft signs are discovered during a thorough history and physical exam once airway stability is assured. The majority of vertebral artery injuries will present without acute neurological symptoms, however any transient ischemic attack (TIA) or stroke symptoms, are specific to the vertebrobasilar artery territory.
| Hard Signs | Soft Signs | |
|---|---|---|
| Vascular injury |
|
|
| Aerodigestive injury |
|
|
The most concerning complication of BCVI is stroke. Because the development of neurologic symptoms from BCVI is frequently delayed, clinicians have both a challenge and opportunity to identify lesions prior to the development of an ischemic stroke. The untreated stroke risk following BCVI is 10% to 40% and is highest within the first 7 days. When stroke occurs, it is seen on the first day following injury only one-quarter to half of the time. Forty-three percent of patients will have a focal neurological finding at the time of diagnosis. Strokes from blunt vertebral artery injuries occur less frequently (20% stroke risk) than those from carotid injuries, but tend to present in a slightly more delayed fashion. ,
Potential presenting signs include ipsilateral headache (58% to 92%), neck pain (18% to 46%), pulsatile tinnitus, transient blindness, bruit (12% to 39%) and partial Horner syndrome (9% to 75%). , Because many patients are asymptomatic, several authors have developed screening criteria to identify patients at higher risk for BCVI, ideally prior to the development of stroke symptoms (see Table 36.2 for the two most commonly used criteria). The modified Denver and modified Memphis criteria are both well studied and commonly used to screen for BCVI. The modified Denver screening criteria include signs, symptoms and risk factors. The Eastern Society of Trauma has developed guidelines based on the Denver screening criteria. In addition to the features included in these criteria, other authors have found Type 3 occipital condyle fractures or mandible fractures to increase the risk of BCVI. In fact, one retrospective study revealed that any facial fracture portends a three- to fourfold increased risk. Risk seems to increase with increasing injury severity score, with BCVI seen in less than 3% of blunt trauma patients with ISS ≥16. Some authors have found that substantial numbers of patients are missed using commonly accepted criteria. Using Denver, the probability of BCVI was 20% with no screening criteria met, 33% to 48% with one risk factor, 56% to 64% with two, 80% to 88% with three and 93% with four. Without any cervical spine fracture, there was a 3% risk of vertebral injury versus 33% with a fracture. Approximately 20% to 30% of patients with BCVI have no identifiable risk factors at all.
| Modified Denver Criteria | Modified Memphis Criteria | |
|---|---|---|
| Signs/Symptoms | Risk Factors a | |
|
|
|
These guidelines perform poorly in children, causing both over- and under-utilization of CTA. Criteria can miss as many as two-thirds of children with brain ischemia as seen in some studies. In children, injuries associated with BCVI are: basilar skull fracture (odds ratio; OR 2.21 to 3), cervical spine fracture (OR 3.6 to 3.85), jugular venous injury (OR 45.5), cranial nerve injury (OR 3.1), injury severity score ≥16 (OR 2.65), brain infarct (OR 3.85), hanging (OR 8.71), LeFort fracture, facial fracture, and clavicle fracture. Seatbelt sign in isolation has not been associated with BCVI, but it is used in some screening criteria for BCVI. A new score proposed for children (the McGovern score) was promising in an early trial, but still misclassified 19% of injured patients.
In penetrating trauma, air leaking from the wound site, odynophagia, dysphagia, and gas in the deep soft tissues are the most compelling indicators of an underlying esophageal injury. Otherwise, there are no pathognomonic signs of esophageal injury based on history or physical exam. Soft signs of injury include hematemesis, odynophagia, dysphagia, subcutaneous emphysema, and blood in the saliva or nasogastric tube aspirate. Other associated findings include dyspnea, hoarseness, stridor, cough, pain and tenderness in the neck, and resistance to passive neck movement. Recent studies provide strong evidence that a normal examination coupled with CTA lacking proximity wounds while confirming the absence of deep tissue emphysema can safely exclude any surgically significant esophageal lesions. ,
Blunt PE injuries are rare with little published data on clinical recognition. Signs and symptoms of penetrating PE injury may be useful in identifying patients with blunt PE injury. These injuries tend to be associated with facial fractures (16%) and traumatic brain injury (13%).
Signs and symptoms of penetrating and blunt LT injury overlap and one quarter of these patients ultimately requiring surgery will have no symptoms on arrival. Delays in symptom onset can exceed 24 hours with some remaining asymptomatic. ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here