Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A 65-year-old previously healthy man presented to the emergency department for several months of progressive upper extremity weakness and blurry vision. He reports that over the past 3 months, playing the violin and mowing the lawn have become more difficult because the longer he does these activities, the weaker his arms become. His hands and forearms still feel strong. His brother accompanies him and has noticed that in the evenings his eyelids seem to droop more. The drooping worsens the more he blinks. He also feels short of breath when lying flat. He was admitted to the neurology service for further workup. Respiratory parameters were monitored throughout his hospital course and remained stable. Neurologic exam was significant for asymmetric, right greater than left ptosis, significant eye closure and cheek puff weakness, and fatigable weakness of proximal upper and lower extremities. On electromyography, repetitive stimulation of the spinal accessory muscle demonstrated a reproducible, 30% decrement in compound muscle action potential amplitudes.
He was treated with intravenous immunoglobulins for presumed myasthenia gravis with improvement in his ptosis and proximal muscle weakness. Chest computerized tomography (CT) did not reveal a thymoma or thymic hyperplasia. He was started on prednisone and pyridostigmine. He presented to clinic 1 month later in follow-up at which point his acetylcholine receptor antibodies had returned to positive. His prednisone dose was increased due to continued symptoms and he was started on a steroid-sparing immunosuppressive therapy with mycophenolate mofetil.
Myasthenia gravis (MG) is caused by autoantibodies directed against components of the postsynaptic neuromuscular junction (NMJ). The loss of large numbers of functional acetylcholine receptors (AChRs) decreases the number of muscle fibers that can depolarize during motor nerve activation, resulting in reduced muscle fiber action potentials and muscle fiber contraction. Failure of neuromuscular transmission results in clinical weakness when it affects large numbers of muscle fibers ( Fig. 68.1 ). The most common cause of acquired MG (approximately 85%) results from the development of autoantibodies directed to the nicotinic AChR on the postsynaptic membrane. AChRs are composed of five protein chains (2 α, β, ε, and δ) that are arranged in a transmembrane ion channel that crosses the postsynaptic cell membrane ( Fig. 68.2 ). Anti-AChR autoantibodies target the α subunit, which has binding sites for acetylcholine. Another target for autoantibodies in MG is the muscle-specific tyrosine kinase (MuSK) postsynaptic protein. MuSK anchors the AChR to the postjunctional membrane. Anti-MuSK antibodies are found in approximately 5%–7% of all MG patients. Several more antibody targets have been recently discovered in MG patients who are seronegative to both AChR and MuSK. These include autoantibodies against low-density lipoprotein receptor-related protein 4 (LRP4), agrin, and cortactin. LRP4 is a receptor for agrin and MuSK. The binding of LRP4 to agrin increases agrin's affinity for MuSK. This protein complex in turn activates and clusters AChRs at the NMJ. Additionally, MuSK anchors acetylcholinesterase at the synaptic basal lamina. Cortactin acts downstream of the agrin/MuSK complex to promote AChR clustering. Antibodies to titin and ryanodine receptors have also been identified; their clinical significance is still under investigation ( Fig. 68.3 ).
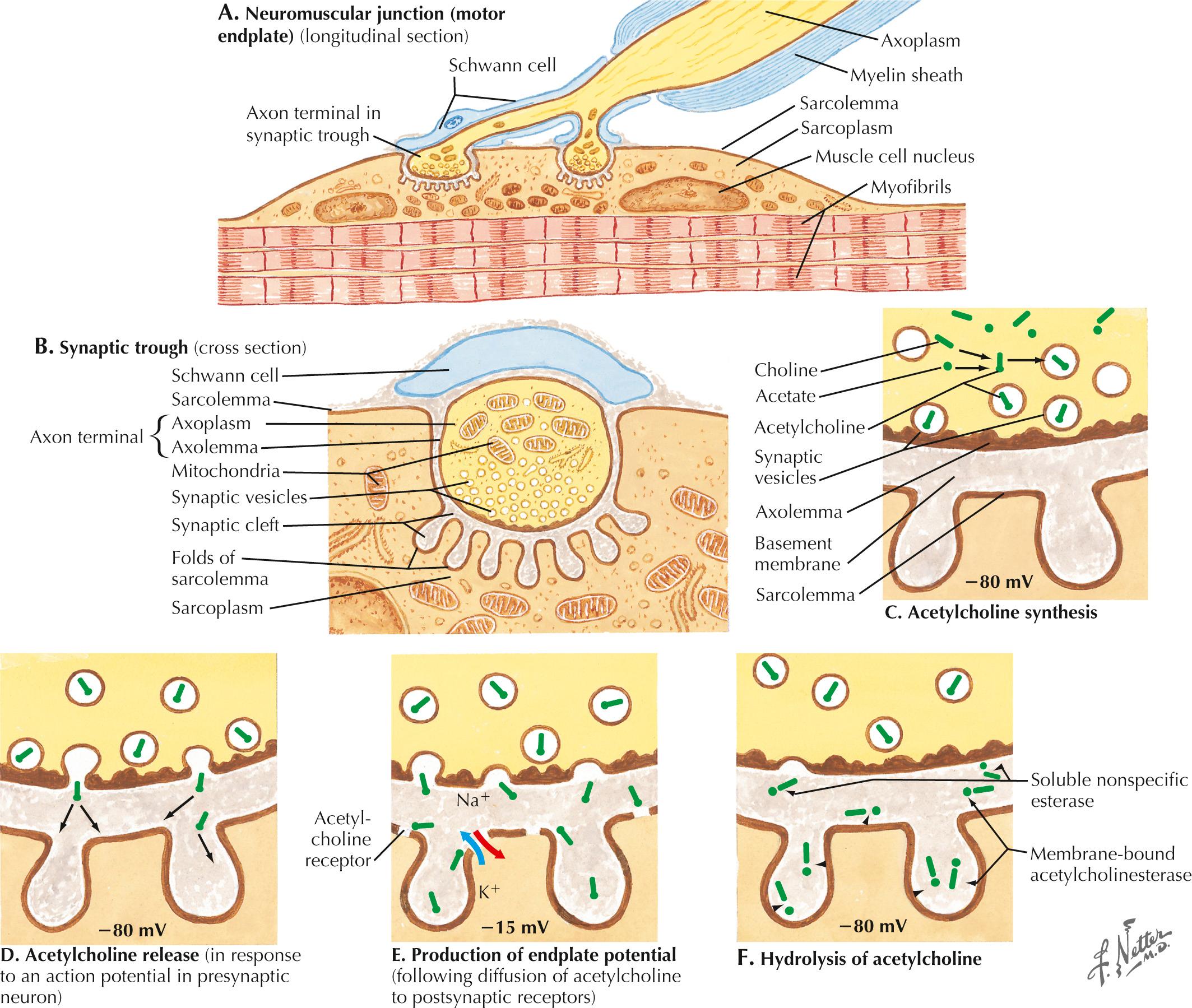
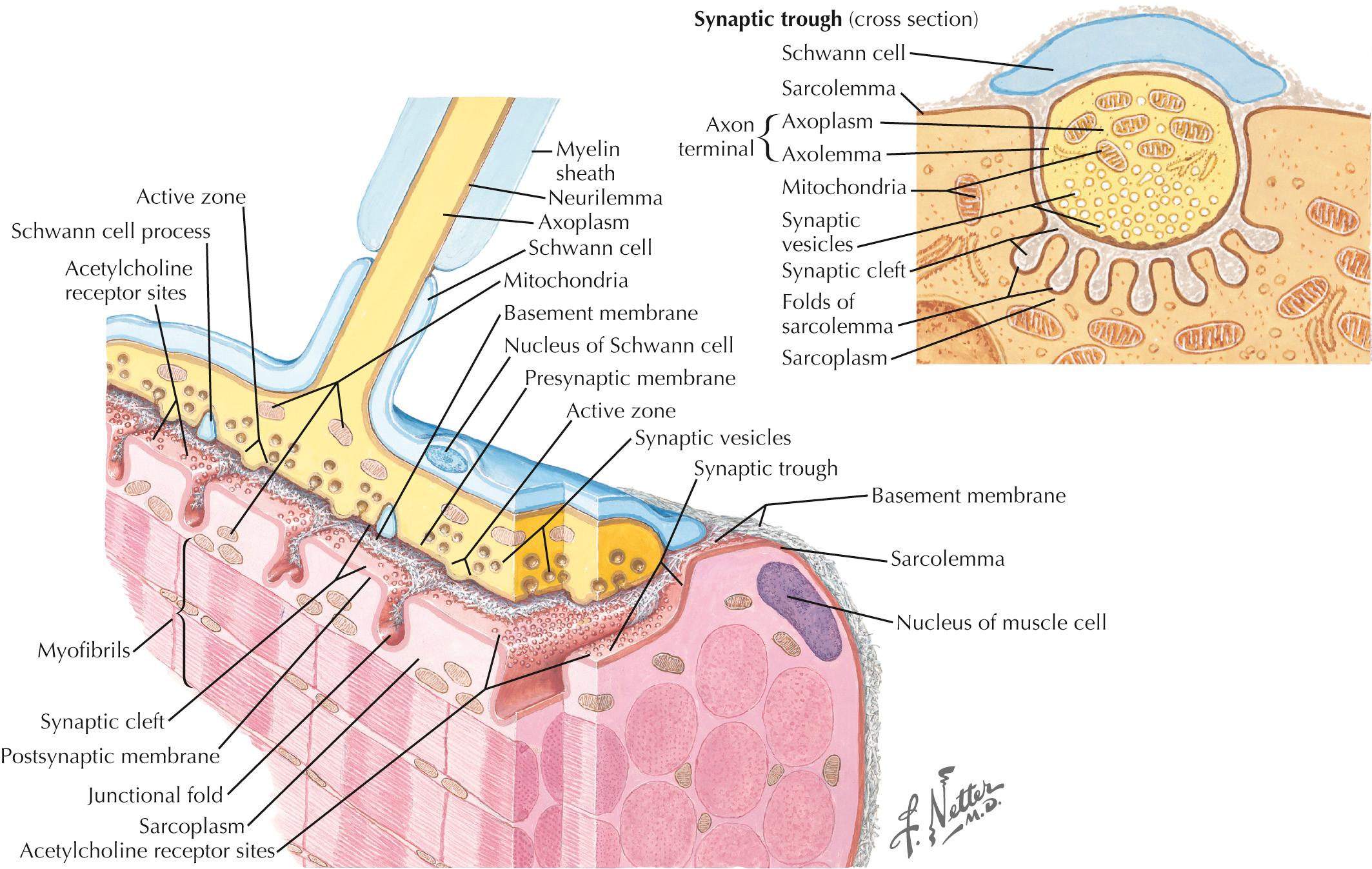
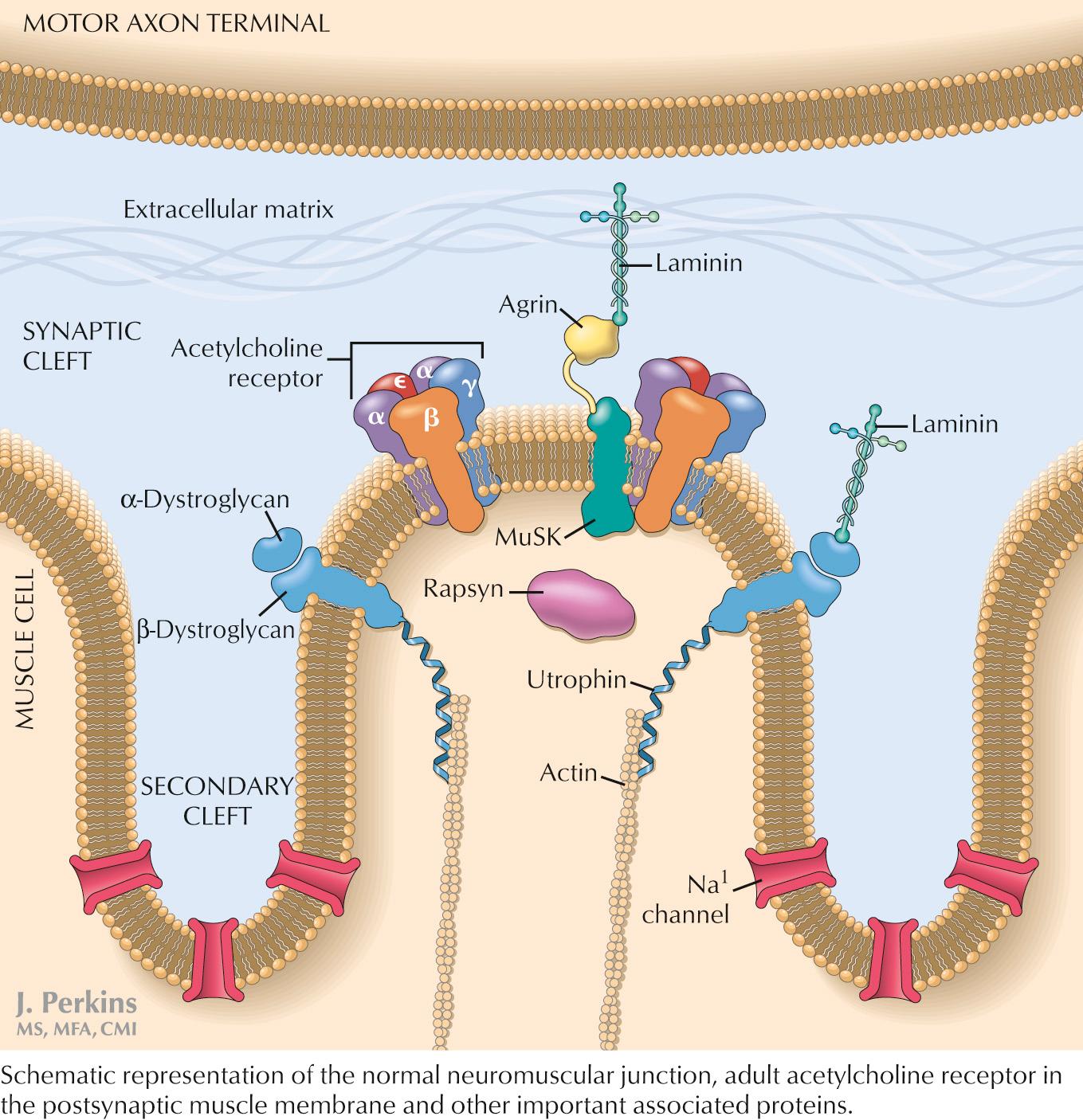
The AChR autoantibodies disrupt neuromuscular transmission in one of three ways: (1) complement-mediated activation that leads to destruction of the postsynaptic membrane, (2) endocytosis of the AChR, and (3) less commonly, direct blockage of the ACh binding site. The loss of functional AChRs in this way decreases the number of muscle fibers that can depolarize, resulting in decreased generation of muscle fiber action potentials and subsequent muscle contraction. This leads to functional muscle weakness.
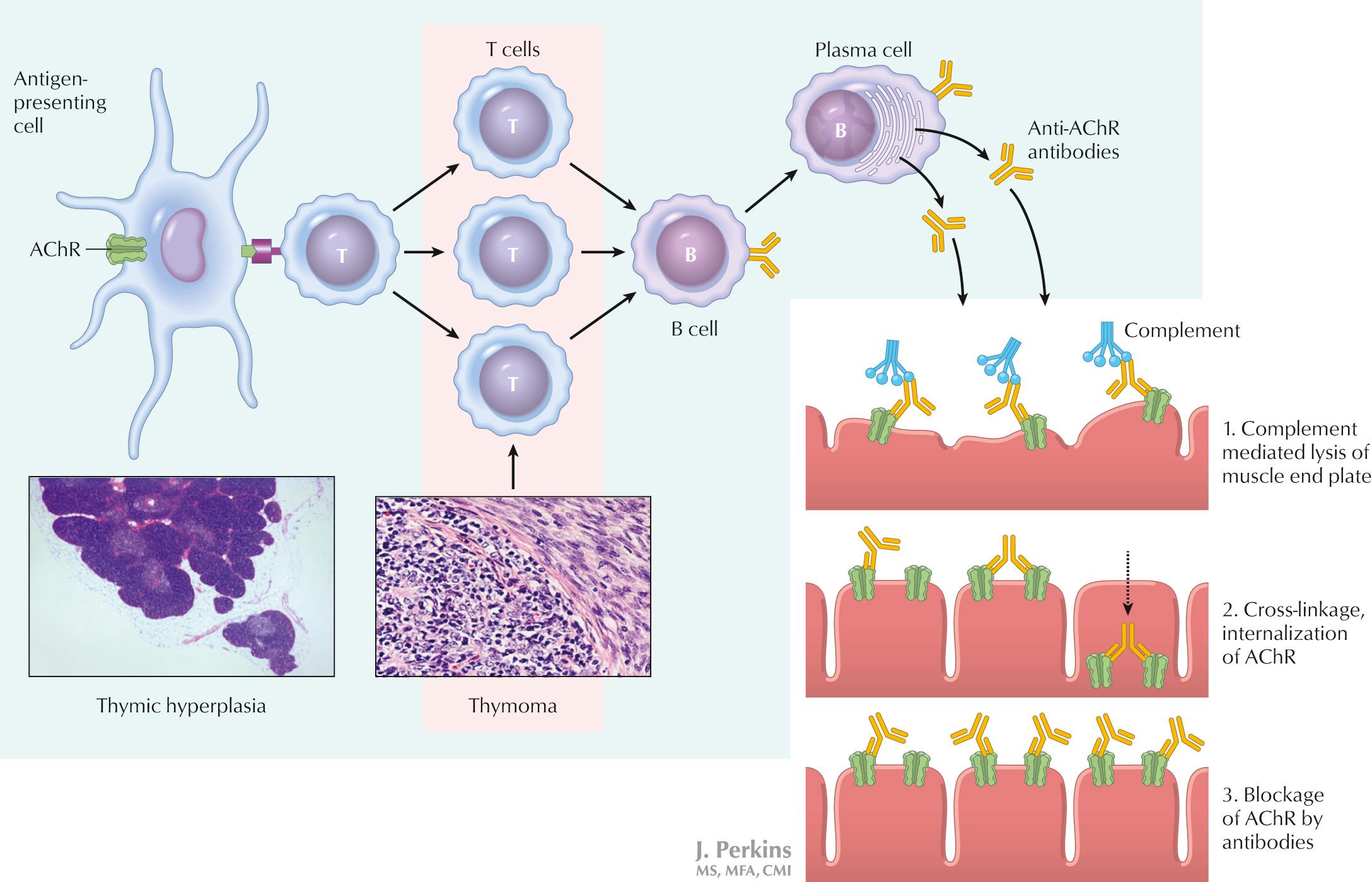
The thymus gland is an immune system organ that generates many naive T cells and clearly plays a role in the pathogenesis of MG. Patients can have follicular hyperplasia or thymomas, and the presence of either has implications for the progression and treatment of the disease. Thymomatous MG is typically more severe and requires thymectomy ( Fig. 68.4 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here