Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Microscopes have always been the essential tool for pathologists and will likely remain so. Although this relationship is now being questioned due to increasing reliance on digital imaging, it is important to remember that a tissue section is a three-dimensional object with optical properties that cannot be fully captured by a photograph—no matter how detailed. The microscope will continue to play an important role in that it does not just magnify tissues, but is also an analytical tool that detects optical properties such as refraction and polarization.
Although it is not necessary to have an advanced degree in optics, it is important to understand the basics of microscope use, special techniques useful to the pathologist, and optical properties of biologic and synthetic materials present in clinical specimens. These topics are covered in the sections below.
Optimal image formation occurs when the image is in focus and the illumination is appropriately adjusted. First, the eyepieces should be adjusted for width (by sliding them back and forth) in order to form a single image. Second, each eye is closed in turn individually to adjust the focus of each eyepiece. Many people have subtle differences between their two eyes. Finally, the illumination is adjusted to ensure that the light is bright, evenly dispersed, glare free, and that good image contrast is achieved. This procedure is termed “Koehler illumination” after August Karl Johann Valentin Kohler (1866–1948) who first determined the optimal settings for his Ph.D. thesis in 1893.
Parts of the microscope used for Kohler illumination:
Field diaphragm: This is an iris diaphragm at the base of the microscope that is adjusted by moving the surrounding circular ring. Closing the diaphragm limits the size of the illuminated field on the stage of the microscope.
Substage condenser: This is located just below the stage. It can be moved up and down. It is centered using two screws.
Aperture iris diaphragm: This iris diaphragm is located in the substage condenser. It is adjusted using a rotating ring on the front of the condenser.
Adjusting a microscope for Koehler illumination:
Open the aperture diaphragm and the field diaphragm completely. Using a 20× objective, focus on a slide on the stage.
Close the field diaphragm almost completely. Raise the condenser until the edges of the diaphragm are sharply focused (the condenser is usually at about its highest position).
Use the centering screws on the substage condenser to center the image of the field diaphragm. Slowly open the field diaphragm until it just disappears from view.
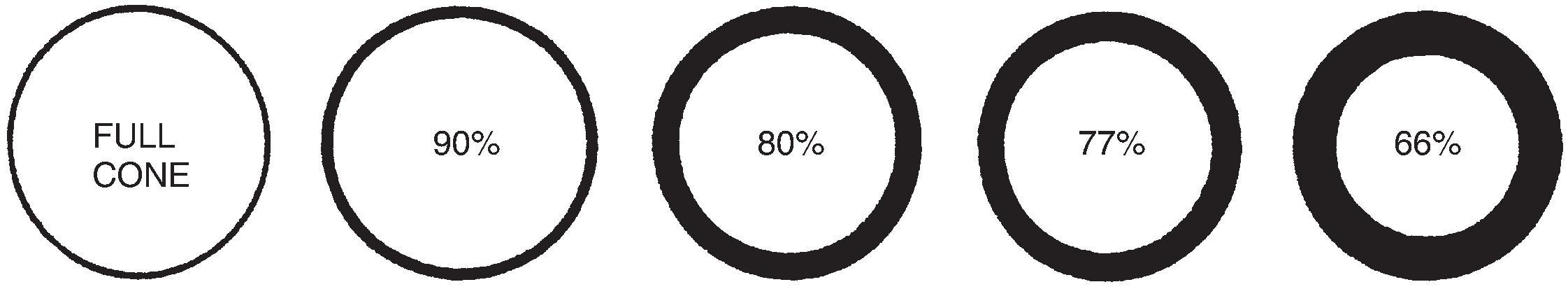
Remove one eyepiece objective and look into the tube. Open and close the aperture diaphragm until only 66–77% of the back lens is illuminated ( Fig. 7.1 ). This prevents unnecessary light from entering that creates glare.
The microscope is now optimally adjusted for the objective. Other objectives will require readjustment and in practical terms usually a compromise position is used that is adequate for all of the objectives. A reasonable solution is to center the field diaphragm for a 40× objective and maintain its opening for a 10× field. The substage condenser should be slightly below the level where dust is brought into focus using a 10× objective. As objectives are changed, only the aperture diaphragm need be changed to optimize contrast.
If the light intensity needs to be adjusted, it is accomplished by using the transformer, not by changing the position of the condenser or diaphragm.
Contrast can be increased by closing the aperture diaphragm below 60% or by lowering the substage condenser. However, resolution and sharpness are reduced. This maneuver may be useful if looking for refractile material (see section below).
Oil immersion lenses (usually 100×) can achieve higher magnifications than dry lenses. Because the refractive index of oil is higher than that of air, light rays coming from the slide are bent to a greater degree and thus an oil objective can capture more of these light rays which results in greater resolution.
There are two major uses in surgical pathology for oil immersion magnification:
Hematologic specimens: Due to the generally small size of the cells and the importance of subtle nuclear and cytoplasmic features for characterization, higher magnifications are helpful.
Small microorganisms: Some organisms such as acid-fast bacilli or microsporidia are best seen at high magnification.
There is virtually no other use for oil immersion lenses. This has led to the old saying in pathology that “low power pathologists make high power diagnoses.” The use of oil should be avoided outside of the applications cited above due to the frequent contamination of the microscope and other objectives with oil if great care is not used.
Only immersion oil designed for microscopic use should be employed. Lint-free tissues or lens paper should always be available to wipe away any excess oil before it drips into the microscope or onto other surfaces.
Using an oil immersion lens:
Focus the microscope using the highest magnification available with a dry objective. It is helpful to identify and mark the area(s) of the slide to be examined under oil with ink to avoid the need to scan the slide after oil is applied.
Swing this objective away (in the direction to bring the oil objective into place) and place a small amount of oil on the slide.
Swing the oil objective into place, making sure that the space between the objective and the slide is filled with oil. The slide may now be observed.
After viewing, again swing the oil objective partially away from the slide.
Immediately wipe the objective with lens paper to prevent oil from dripping onto the microscope. If the oil is allowed to dry, it can be difficult to remove and efforts to do so can damage the lens.
Remove the slide and wipe off excess oil with lens paper. The slide may then be cleaned with a small amount of xylene. Peripheral blood smears are often viewed under oil without using a coverslip. The oil can be wiped directly off the slide.
Do not attempt to view a slide with a high power dry objective while there is oil on the slide! If it is necessary to scan a slide, place a 4× objective adjacent to the oil objective. One can safely alternate between these two objectives without contaminating the 4× objective with oil. It is very difficult to clean oil off an objective not designed to be used with oil (see the section on cleaning objectives below).
The optical properties of microscopic objects reveal clues about their structure and identity ( Table 7.1 ).
| TYPE | POLARIZABLE | REFRACTILE | LOCATIONS USUALLY SEEN | APPEARANCE/STAINS | COMMENTS | HISTOLOGIC APPEARANCE |
| ENDOGENOUS Material | ||||||
| Amyloid | Yes | Yes/no | Bone marrow (multiple myeloma), medullary carcinoma of the thyroid, periarticular tissue in dialysis patients, many other sites | Acellular homogeneous pink material, sometimes with giant cells. Congo red +: orange/red without polarization and green, orange or yellow with polarization | Immunoperoxidase studies can be used to identify specific types of amyloid: Multiple myeloma—lambda and kappa chains Medullary carcinoma of the thyroid—calcitonin Dialysis related amyloidosis - ß 2 microglobulin EM can also be used to recognize amyloid |
 |
| Bile | No | No | Liver—hepatocytes or intracanicular | Dark green–brown globules (intra or extracellular). PAS + | May be helpful for recognition of hepatocellular carcinoma | |
| Bone and collagen | Yes | No | Joints and connective tissue | Normal bone—polarization shows regular osteoid seams (not seen in woven bone) Type I collagen is polarizable. Type III collagen (reticulin) is not polarizable |
Bone and collagen overstained with Congo red will show green birefringence after polarization. A properly stained slide should not show background staining Trichrome stains and reticulin stains can be used to identify collagen Nodular sclerosing Hodgkin's disease is associated with polarizable collagen |
|
| Calcium oxalate | Yes | Yes | Apocrine cysts of the breast, benign thyroid follicles, giant cells in sarcoidosis | Flat rhomboid (sometimes needle shaped) colorless or pale yellow crystals. Can be difficult to see without polarization | Can be the source of mammographic calcifications in breast biopsies Also present in congenital hyperoxaluria |
 |
| Calcium phosphate | No | No | Benign and malignant breast lesions, areas of chronic inflammation or necrosis, deposition on collagen (e.g. heart valves), pulmonary blue bodies | Purple granular material Calcium stain + |
Most common source of mammographic calcifications |  |
| Calcium pyrophosphate dihydrate crystals | Yes | Yes | Large joints in periarticular tissues (uncommon in small joints of foot or hand) | Blue to purple short rhomboid crystals (but may be needle shaped) | “Pseudogout” or chondrocalcinosis The crystals are water soluble and require anaqueous processing for best demonstration. They can sometimes be demonstrated with polarization of an unstained tissue section |
 |
| Charcot–Leyden crystals | No | Yes | Sites of eosinophil accumulation (e.g. chronic sinusitis, parasitic infections, asthma) | Bright-red, needle-like crystals | Formed from galectin-10 released when eosinophils undergo cytolysis |  |
| Corpora amylacea | No | No | Prostate, brain, lung | Extracellular laminated light pink spherical structures | Incidence increases with age |  |
| Gamna–Gandy nodules | No | Yes/no | Spleen, lymph nodes, thymus gland, thyroid, cardiac myxomas | Granulomas consisting of hemosiderin, calcium, foreign body giant cells, and ovoid or bamboo shaped structures | “Siderotic granulomas” found in sites of prior hemorrhage , Can mimic fungal mycelia or parasite eggs |
 |
| Hamazaki–Wesenberg bodies | No | Yes | Areas of prior hemorrhage, lymph nodes (sinusoids) | Small round to ovoid brown bodies that may appear to be budding | Can mimic pigmented fungal forms or bacteria |  |
| Hemosiderin | No | Yes | Any area of hemorrhage Liver in hemochromatosis and hemosiderosis |
Coarse granular brown intra and extracellular granules. Iron stain + | A complex of iron and ferritin Useful in distinguishing prior bleeding from intraoperative bleeding |
|
| Liesegang rings | No | No | Any area of old hemorrhage | Round extracellular concentric laminated or fibrillated concretions of precipitated proteins | May be mistaken for the Giant Kidney Worm or fungal organisms. , , Similar pattern to psammoma bodies |  |
| Lipids | No/yes | No | Polarizable lipids may be present in xanthomas, histiocytosis X, and other dermatopathologic entities, and fat necrosis secondary to pancreatitis Cholesterol crystals are often seen as empty clefts in areas of cell injury | Needle-shaped clear crystals of varying size, plate-like structures, or intracellular rounded structures. Oil red O +. Sudan black + | Must have special processing or frozen sections to avoid loss during processing Also present in metabolic storage diseases such as Gaucher, Neimann-Pick, and Wolman disease Polarized crystals in fat necrosis may be due to pancreatitis |
 |
| Lipofuscin (oxidized lipid precursors) |
No | No | Sites of atrophy or chronic injury | Fine yellow–brown granules to coarse granules resembling hemosiderin. PAS + | Ochrocytes are histiocytes containing lipofuscin | |
| Malaria pigment (haemozoin, hematin) | Yes | No | Macrophages and erythrocytes | Brown to black granules inside macrophages | Present in malaria and schistosomal infections or severe hemolytic anemia Formalin pigment can resemble malaria pigment |
|
| Melanin | No | No | Normal melanocytes in basal epithelium, pigmented malignant melanomas | Fine brown or black granules but can sometimes resemble hemosiderin. Fontana Masson + | ||
| Michaelis–Gutmann body | No | No | Malakoplakia | Concentric targetoid bodies (“owl-eye”), intra and extracellular. Iron stain +, Von Kossa +, PAS + | These bodies form due to defective phagocytosis of bacteria—most patients have a chronic coliform infection. Forms masses that can mimic tumors |  |
| Prostatic crystalloids | No | Yes | Prostate carcinomas | Bright eosinophilic angulated crystals in lumens of adenocarcinomas | When present in the prostate, these crystals are always associated with cancer—if present on a core needle biopsy in the absence of cancer, additional levels should be examined Similar crystals are rarely seen in DCIS of the breast |
 |
| Psammoma body | No | No | Papillary carcinoma of the thyroid, ovarian carcinoma, lactational-like changes in the breast, others | Laminated concentric rings of calcium phosphate | Very specific in the thyroid for papillary carcinoma Similar structure to Liesegang rings |
 |
| Reinke crystals | No | Yes | Leydig cells of the testis, hilus cells of ovary, and their tumors | Rod-shaped eosinophilic crystals. Masson's trichrome + (magenta) | The crystals dissolve in formalin They are better preserved in frozen sections, touch imprints, and tissue fixed in alcohol |  |
| Schaumann bodies | No | No | Intracytoplasmic inclusions seen in the granulomas of sarcoid, tuberculosis, and chronic beryllium diseases | Concentric basophilic rings | These bodies are most commonly seen in sarcoidosis. Other types of inclusions in sarcoidosis are calcium oxalate crystals and asteroid bodies (spider-shaped inclusions). These inclusions are not specific for sarcoid |  |
| Spironolactone bodies | No | No | Adrenal adenomas associated with Conn syndrome | Concentric laminated eosinophilic inclusions (2–12 microns) in cytoplasm. PAS + | Found in tumors in patients with Conn syndrome, treated with spironolactone IHC can identify aldosterone in the bodies |
 |
| Uric acid crystals (gout) | Yes | Yes | Periarticular tissues around joints, other areas of connective tissue | Long needle shaped crystals (sheaves of wheat) are characteristic but may be fractured and appear to be smaller crystals | Requires anaqueous processing for preservation In routine H&E sections only needle shaped holes may be seen where the crystals are dissolved. The crystals may be seen in routinely fixed tissue if the tissue is unstained |
 |
| Iatrogenic Material | ||||||
| Barium sulfate | No/yes | Yes | In GI tract after radiologic examination, in peritoneum after perforation, within bone cement | Golden refractile granular material. May be intra- or extracellular | Rarely incites an inflammatory reaction | |
| Bile acid sequestrants | In GI tract | Bright orange (but also black or red), rectangular shape (but may be rounded), smooth texture (fish scale texture uncommon); may have small dot-like inclusions. AFB dull yellow | These agents are usually used to treat diarrhea and do not cause bowel damage. Also see kayexalate and sevelamer as these agents are also seen in the GI tract | |||
| Cotton fibers | Yes | Yes | Around surgical sites | Hollow discoid fibers, present intra or extracellularly | ||
| Cornstarch | Yes | No | In surgical sites | 3–20 micron spheres. Maltese cross appearance after polarization. PAS+, MSS+ | Used to lubricate surgical gloves. However cornstarch should be avoided as it can incite a granulomatous response | |
| Formalin pigment | No | Yes | Most commonly seen in bloody tissues | Brown or black finely granular extracellular deposits | Due to a reaction between formic acid and heme during fixation. Can be avoided by using buffered formalin Can be mistaken for malaria pigment |
|
| Gelfoam | No/yes | No/yes | Within vascular spaces of hemangiomas or other vascular lesions, sometimes used to mark breast core needle biopsy sites | Irregular fenestrated bluish or clear material | Numerous substances are used for embolization including polymer foams (such as gelfoam), poly (vinyl alcohol) particulates, gelatin products, microspheres, and drug- eluting beads. , , Autologous tissue including blood clots and tissue (subcutaneous tissue or muscle) have been used in the past. Metallic coils are also used | |
| Gold | Yes | No | Skin, lymph nodes, organs of patients treated with gold for rheumatoid arthritis | Small intracellular black particles in histiocytes | Gold in intramammary LNs can mimic mammographic calcifications. This treatment is now uncommon. Black deposits in lymph nodes are more likely to be due to tattoo pigment | |
| Graft material—Gortex or Dacron | Yes | Yes | Grafts | Numerous uniform round filaments with small black granules | ||
| India Ink (tattoo pigment) |
No | No | Injected into the site of biopsied colonic polyps | Black granular pigment in stroma or within histiocytes | Used to document the site of a previously biopsied polyp on the serosal surface to aid in colonic resection. Indocyanine green and autologous blood are also used , | |
| Kayexalate (sodium polystyrene sulfonate) | No | Yes | GI tract | Rectangular purple to red crystals with a fish scale pattern. PAS + and AFB black | Used to treat patients with renal-failure as a potassium-binding agent. Can cause ulcers, perforation, necrosis, and pseudotumors (Gonzalez) | |
| Melanosis coli | No | No | Lamina propria of the colon | Fine brown to black granules in macrophages. PAS +, silver stain + | Associated with anthracene-derived bowel cathartics. Can cause grossly pigmented colonic mucosa | |
| Mercuric chloride | Yes/no | No | Tissues fixed in mercury containing fixatives | Dark brown granular extracellular deposits throughout the tissues | Should be removed by proper tissue processing | |
| Metal | No | No | Tissue around prosthetic joints, rarely at surgical sites | Small black irregular angulated or needle shaped fragments that may be intra or extracellular | ||
| Minocycline | No | No | Thyroid, atheromatous plaques, substantia nigra | Black granular pigment | Found in patients treated with minocycline | |
| Myospherulosis | No | No | Nasal cavity and paranasal sinuses and subcutaneous tissue | Sac-like structures with outer lipid surrounding endobodies (red blood cells) | Due to packing with a petroleum based ointment resulting in a benign mass formed by erythrocytes and exogeneous or endogenous lipids Can be mistaken for protothecosis or fungi, carcinoma, osteofibrosis, or metastasis |
|
| Polyethylene | Yes | Yes | Tissue around prosthetic joints | Large fragments, filaments, shards, or small intracellular fragments. Often with a giant cell reaction. Oil red O + | ||
| Polymethylmethacrylate (bone cement) |
No | No | Tissue around prosthetic joints | Round to oval holes surrounded by a giant cell reaction | Dissolves in xylene. Barium sulfate may be present within the bone cement | |
| Sevelamer | GI tract | Rectangular crystals with a fish scale texture, usually pink center and yellow edges (also brown, red, purple). AFB magenta | This is used as a phosphate-lowering medication in patients with renal failure. Can cause mucosal injury | |||
| Silicone | No | Yes | In tissue around implants, rarely in draining lymph nodes | Silicone may be removed during processing and appear as empty holes with residual refractile material around the edge | Intracellular silicone appears like multiple vacuoles in histiocytes that can be mistaken for lipoblasts Other organic oils can have the same appearance |
|
| Surgical gut sutures | Yes | No | Prior biopsy sites (often seen in breast) | Ovoid deeply eosinophilic monofilament often surrounded by a chronic inflammatory response and giant cells | Comprised of connective tissue (predominantly collagen) from cows or sheep. Nuclei may be spindle shaped (due to sterilization by cautery) and the suture may develop jagged edges during resorption. Gut sutures may be mistaken for metaplastic bone | |
| Other sutures | Yes | Yes | Surgical sites | May be monofilament or polyfilament. Often colorless | Absorbable sutures may be surrounded by chronic inflammation | |
| Talc | Yes | Yes | Pleura after talc pleurodesis, abdominal sites after perineal talc use, granulomas in intravenous drug abusers | Irregular clear to yellow crystalline material | Talc can be present in pelvic region lymph nodes, cervix, uterine corpus, fallopian tubes, and ovaries of women using perineal talc and has been associated with ovarian carcinoma , | |
| Tattoo pigment | No | No | Dermis of skin at site of tattoo or in draining lymph nodes | Black (or other colors) granules, may be in histiocytes | Tattoo pigment in axillary lymph nodes can mimic mammographic calcifications. , , It can also mimic melanin in patients with melanoma. During surgery, the darker nodes can mimic sentinel nodes marked with blue dye | |
| Thorotrast (thorium dioxide) | No | No | Liver, spleen, and lymph nodes | Coarse light brown or gray granules in histiocytes or stroma—similar to the appearance of hemosiderin | This radiocontrast agent was used in the 1930s–1940s until it was realized it was associated with cirrhosis, hepatocellular carcinoma, bile duct carcinoma, and angiosarcomas of the liver and spleen (Takekawa). It has a half-life of 400 years. Slides of tissue with thorotrast are radioactive, which can be demonstrated by autoradiography | |
| Environmental Material | ||||||
| Anthracotic pigment (carbon) | No | No | Lymph nodes of the respiratory tract | Black granular deposits in macrophages | The appearance is very similar to tattoo pigment and gold. However, these substances are seen in peripheral lymph nodes | |
| Asbestos fibers | No/yes | No | Lung | Thin fibers encrusted with beaded protein and iron (ferruginous bodies) | Specific identification requires spectroscopic analysis. Similar bodies can be seen with aluminum silicate, fiberglass, or lung elastin Quantification and identification of fibers can be performed by energy dispersive X-ray analysis |
|
| Insects (flies and ticks) | Yes | Yes | Skin and subcutaneous tissue | Variable | ||
| Silica | Yes | No | Lymph nodes of the respiratory tract, silicotic nodules | Minute polarizable material in histiocytes and fibrotic nodules | May be seen in workers exposed to silica Lung disease is often complicated by superimposed infections |
|
| Plant material | Yes | Yes | Colonic rupture, lung (if aspirated) | Cell walls are readily identifiable by polarization | Can be useful to document colonic rupture | |
“Refractile” objects: These objects have a refractive index different than that of normal tissue. Refractility can be highlighted by increasing the contrast (i.e., by lowering the condenser or closing the aperture diaphragm). Refractile objects look brighter and shinier than tissues. This material is usually foreign (e.g., suture material) but can be endogenous such as calcium oxalate crystals. “Doubly refractile” is sometimes used to describe objects that are polarizable.
“Polarizable” objects: Polarized light is light oriented in one specific plane and is produced by using two crossed polarizing filters. Most tissues are isotropic and do not change the quality of light passing through them. They appear dark under polarized light, as very little light passes through the filters in any given plane.
“Polarizable,” “birefringent,” and “anisotropic” are terms used to describe substances that change the direction and speed of the light passing through them. Polarized light passing through such an object is deviated in a particular plane or planes and can pass through a second polarizing filter at an angle to the first. A “polarizable” object appears bright in comparison to the surrounding dark nonpolarizable tissue. Some substances can reflect light at two different wavelengths (e.g., the “dichroic birefringence” of amyloid). Many of these polarizable substances have regular repeating structures (e.g., crystalline) and may be biologic (e.g., amyloid or collagen) or synthetic (e.g., polyethylene).
How to use polarizing filters:
Some microscopes have built-in high-quality polarizing filters. Polarizing material may also be purchased as sheets that can be cut into squares. Polarizers and polarizing material in sheets are available from Edmund Optics ( www.edmundoptics.com or 1-800-363-1992) as well as from other businesses. These lower-cost polarizers can be used to detect foreign material but may not detect other types of substances. Tissues (especially with suspected amyloid) should be observed using the higher-quality built-in polarizers before it is determined that polarizable material is not present.
Definitions:
Polarizer: The polarizing disk below the condenser.
Analyzer: The polarizing disk above the specimen (laid on top of the slide or built into microscope above the objective).
When the polarizer and the analyzer are at 90° to each other, no light can pass through and the field is dark. As the angle between the filters is changed by rotating the polarizer, substances that preferentially reflect light in a specific direction (i.e., polarizable materials) allow light to pass through the analyzer and appear bright.
The determination of “positive” and “negative” birefringence requires using a compensating first-order red filter under polarized light and can be used to distinguish uric acid crystals from CPPD crystals. However, this determination is best performed on crystals in solution and cannot be reliably performed on fixed tissue.
Substances may be neither refractile or polarizable (most tissues and cells), refractile but not polarizable (e.g., hemosiderin), polarizable but not (or poorly) refractile (e.g., amyloid), or both (e.g., suture material). Amyloid can be identified by the apple-green color, as well as other colors, seen under polarization. ,
The microscope can be used to precisely measure objects and distances in microns. Measurement can be important for grading and staging cancers. For example measurements are necessary for the following:
Depth of invasion of malignant melanomas and cervical carcinomas
Fuhrman nuclear grading
Grading breast carcinomas and sarcomas (the size of the microscopic field size must be known in order to score mitoses)
Classification of the size of lymph node metastases for AJCC N category (isolated tumor cells vs. micrometastasis vs. macrometastasis)
Approximate measurements of very small objects can be made by comparison to cells with relatively constant sizes:
a lobe of a neutrophil nucleus2 µm
nucleus of a small lymphocyte5–6 µm
a red blood cell7 µm
a histiocyte nucleus10 µm
However, more commonly larger objects or distances need to be measured. Four different methods can be used depending on the need for accuracy, the size of the object to be measured, and the equipment available ( Table 7.2 ).
| METHOD | LOWER LIMIT OF ACCURACY | COMMENT |
|---|---|---|
| Direct measurement on slide | ~1 mm | Only applicable for larger objects |
| Estimation from field diameters | ~0.5 mm | Very easy to use |
| Vernier scale on stage | 0.1 mm | Available on most microscopes and very accurate. Difficult to remember method |
| Ocular reticule (graticule) | 0.01 mm (10 µm) | Very accurate. Requires special ocular |
This is the most convenient method for objects measuring several millimeters in size. The borders to be measured are carefully marked by ink, and an accurate ruler is used to make a direct measurement.
There are some coverslip films that are permanently marked by ink. Marking on such slides should be minimized.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here