Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The superior mesenteric artery (SMA) and inferior mesenteric artery are susceptible to injury from both blunt and penetrating trauma. Injuries to the mesenteric arteries compose a small subset of intraabdominal vascular trauma. A multiinstitutional study involving 34 trauma centers reported only 250 patients with SMA injuries over 10 years. Due to its smaller size, the incidence of injury to the inferior mesenteric artery is even rarer. Mesenteric arterial injuries are associated with high morbidity and mortality and present challenges for even the most experienced trauma surgeon. Patients are susceptible to massive hemorrhage, and those who initially survive remain at risk for early and delayed complications related to visceral ischemia. Proximal injuries to the SMA are rare but highly lethal. Although trauma to the branches of these vessels is more common, it is managed much like injuries to the bowel parenchyma supplied and is not discussed in this chapter. The diagnosis and treatment of injuries to the superior and inferior mesenteric arteries will be covered. The chapter will describe the associated injury pattern between blunt and penetrating trauma to the mesenteric arteries and their intraoperative management.
As with all intraabdominal vessels, the mesenteric arteries are susceptible to injury from penetrating trauma. Due to their deep retroperitoneal location, they are well protected and more likely to be injured from gunshot wounds than stab wounds. Similarly, they are rarely injured in isolation, and, despite varying degrees of selective conservatism in the management of penetrating trauma, most will be diagnosed upon emergent laparotomy for hemorrhage or peritonitis. The intraoperative management algorithm is presented in the section following the diagnosis of blunt mesenteric artery injury.
The presentation of mesenteric arterial injury resulting from blunt trauma may vary from a stable patient with an incidental finding of intraperitoneal free fluid, or a mesenteric hematoma on imaging, to a an unstable patient with a major vascular injury causing exsanguinating hemorrhage. The management of these two scenarios is vastly different.
Although blunt mesenteric arterial injury generally causes abdominal pain, some patients may remain asymptomatic. Possible signs of mesenteric arterial injury may include bruising to the abdominal wall (seat belt sign), abdominal tenderness, or other signs of peritonitis. In stable patients, abdominal computed tomography (CT) scans are frequently obtained in a battery of imaging studies. Mesenteric hematomas may be seen in isolation but are frequently associated with other injuries to the gastrointestinal tract or solid organs. With the advent of multidetector CT, the recognition and diagnostic ability of minor mesenteric injury has improved over the past 20 years. Historically, patients with blunt abdominal trauma were evaluated with a diagnostic peritoneal lavage to diagnose solid organ or hollow viscus injury. For hemodynamically stable trauma patients, CT imaging is currently favored in the diagnosis of blunt abdominal trauma. Solid organ injury can readily be identified, but evidence of mesenteric arterial injury remains difficult and signs often overlap with blunt hollow viscus injury.
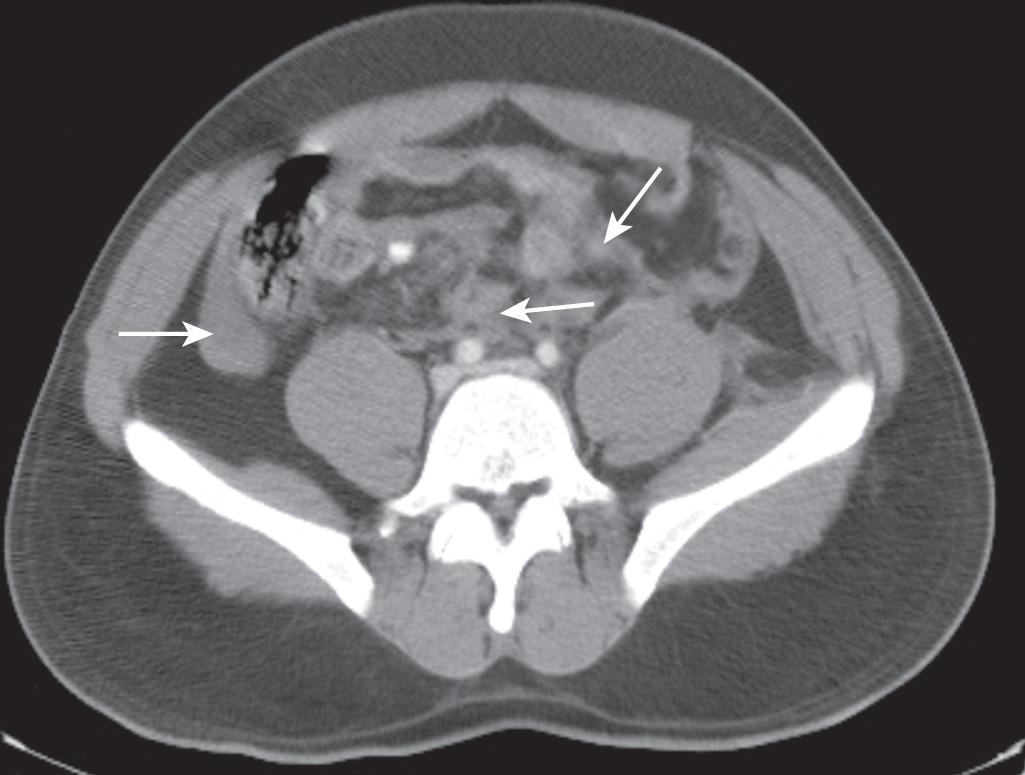
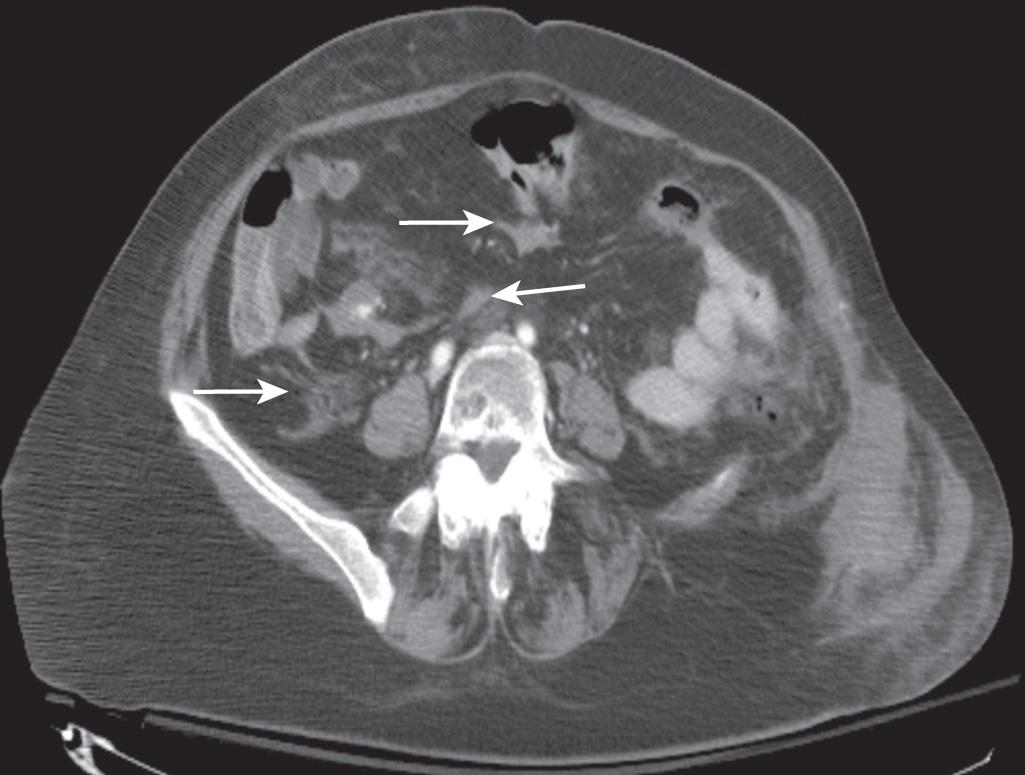
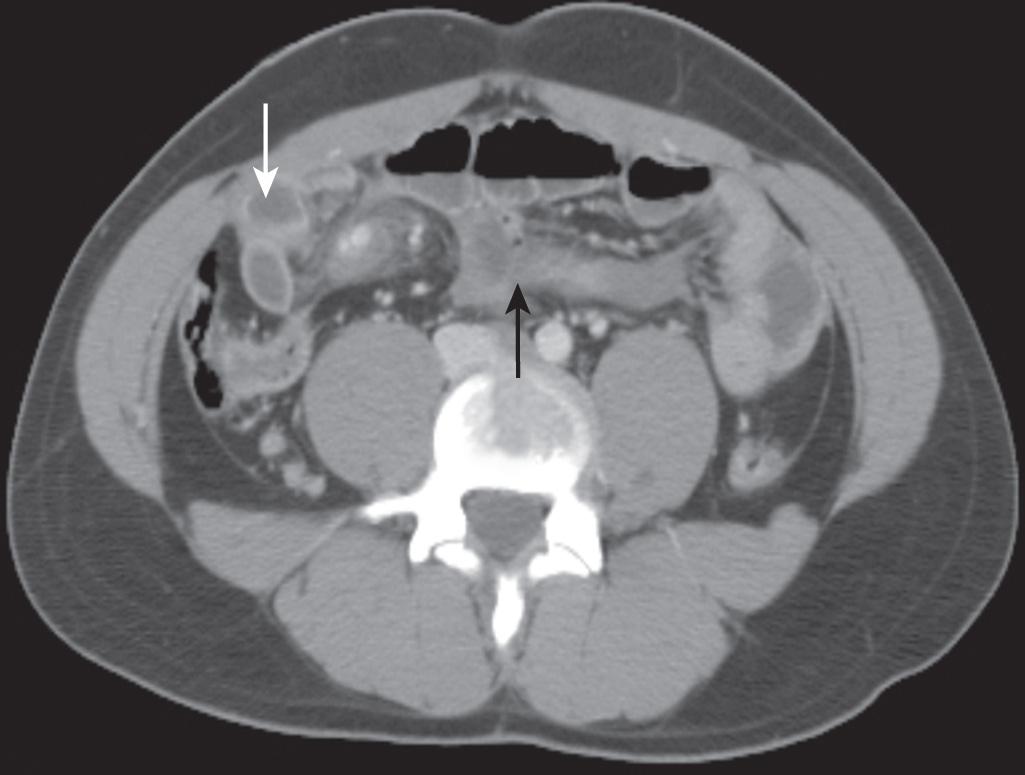
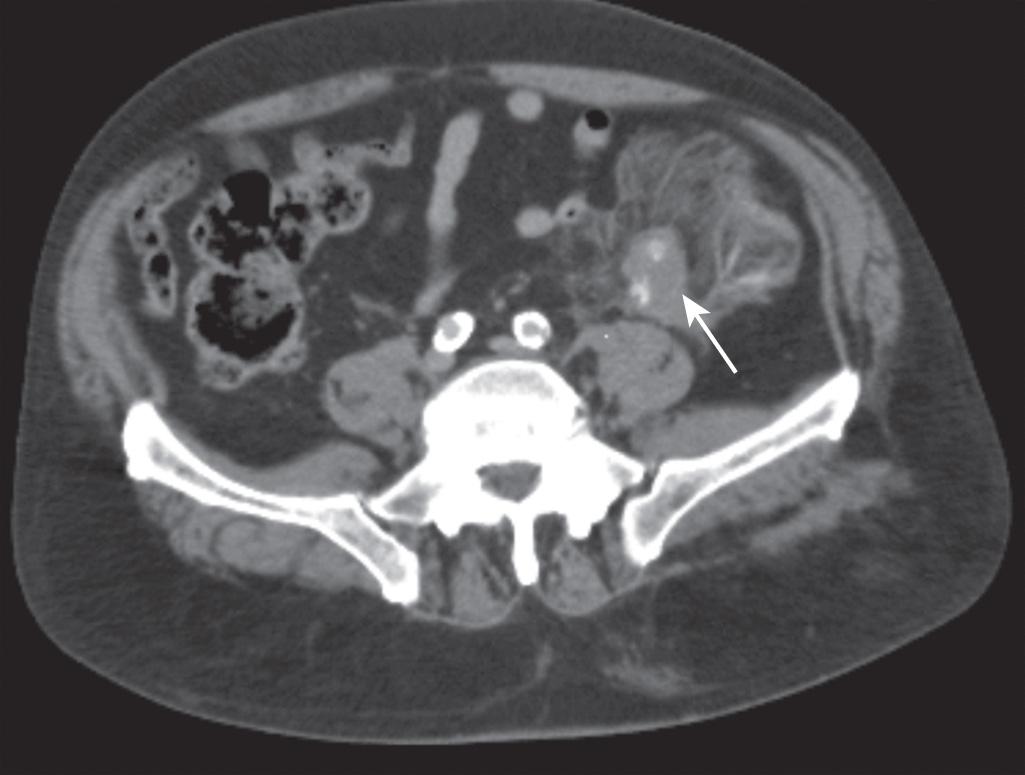
The newest generation multislice CT scanner has increased sensitivity and specificity in the diagnosis of mesenteric injury. CT findings that may suggest mesenteric injury include free intraperitoneal fluid ( Fig. 89.1 ), mesenteric hematomas that may look triangular or polygonal ( Fig. 89.2 ), fat stranding of the omentum, intramesenteric fluid adjacent to thickening bowel wall ( Fig. 89.3 ), mesenteric vessel beading, abrupt termination of mesenteric vessels, or active extravasation of contrast ( Fig. 89.4 ). Active extravasation has the best positive predictive value. Absence of peritoneal fluid has the best negative predictive value. Oral contrast is not required to detect mesenteric injuries. In children, these radiographic findings are less reliable, and clinical data and physical exam should guide the decision to operate. Although we are now better able to detect a mesenteric hematoma or laceration, predicting the clinical implications of a particular injury remains challenging. Due to variations in collateral supply, some patients can compensate for an injury that would cause bowel ischemia in another patient.
The management of stable patients with mesenteric injury should include close observation with serial abdominal exams and may require repeat CT imaging to evaluate for increase in the size of the hematoma or evidence of bowel ischemia secondary to disruption of the blood supply. If at any point the patient develops worsening abdominal pain, worsening or recurrent metabolic acidosis, worsening or delayed ileus, feeding intolerance, evidence of obstruction, peritonitis, or signs of sepsis, surgical exploration may be required.
A patient with active extravasation on CT imaging may require urgent exploration for control of hemorrhage and evaluation of bowel viability. If there is a question of bowel viability, a planned second-look operation is prudent. There are anecdotal case reports of laparoscopic procedures with intracorporeal control of hemorrhage and/or resection, as well as transcatheter arterial embolization of small mesenteric hemorrhage, but these techniques are not currently recommended except in centers with specialized expertise.
The long-term consequence of a mesenteric injury is difficult to determine. There are case reports of late small bowel obstruction and mesenteric fibrosis that occurred in patients with a history of blunt abdominal trauma. These late complications are thought to be a result of subclinical bowel perforation or localized gut ischemia caused by injury of the mesenteric vasculature. The majority of our discussion refers to injuries of the superior mesenteric arterial system. Injuries to the inferior mesenteric artery are rare and generally can be treated with ligation. An uninjured superior mesenteric system usually prevents ischemic sequelae.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here