Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The earliest descriptions referencing the management of mandible fractures date back to Ancient Egypt (1650 BC) in which the pathology was described as incurable, inevitably resulting in infectious complications, and leading ultimately to demise. Hippocrates would revolutionize the management with his introduction of the concepts of reduction and stabilization with circumdental wiring and external bandages for stabilization, similar to the technique of “bridle wiring” still used today.
Through the centuries, a number of techniques to achieve closed reduction and stabilization of the various fracture patterns were introduced. In early times, external bandaging came into popularity with the introduction of the Barton Bandage. This would quickly fall out of favor, however, due to resulting “bird face” deformities and malunion in the setting posterior deformational forces. Subsequently, a number of extra-and intraoral appliances would be introduced. Early designs were primitive, vice-like, and only moderately effective in gaining proper occlusion and adequate immobilization to promote union. It would be Gunning who would first utilize a customized intraoral splint for immobilization in combination with a head-piece that allowed for relative intermaxillary fixation (IMF). A modified version of Gunning's approach to achieve IMF is still applicable today in the management of mandible fractures in edentulous individuals.
In patients with intact dentition, the mid- to late 19th century would bring the rise of advances in monomaxillary wiring, arches and custom-designed metal splint techniques; but without additional fixation, these methods were found to provide inadequate immobilization to promote bony union.
There are conflicting reports as to whether it was Gilmer or Guglielmo Salicetti who was the first to utilize the modern concept of IMF in the reduction and stabilization of the traumatic mandible. Each supported the use of individual transdental wires on mandibular and maxillary dentition, which were subsequently ligated in an opposing fashion to provide stability and restore occlusion. Gilmer would eventually expound upon this concept, introducing the modern day concept of IMF by fixation of full arch bars to the maxilla and mandible that could subsequently be stabilized with opposing ligatures.
As evidenced by the aforementioned management strategies, early management of the mandibular trauma was approached with closed reduction and immobilization with varied success. It was not until the late 19th century that the first reports of open reduction, internal fixation techniques were published. In 1869, the Thomas principle introduced an intraoral approach to mandibular open reduction followed by transosseous wire osteosynthesis using coil-like silver wire, which could be tightened periodically to achieve bony union. Modifications of transosseous wiring techniques would be frequently utilized in the primary management of mandibular trauma until the 1960s despite criticism that these methods lacked rigid stability across the fracture site.
The incidence of suboptimal unions and complications with wire/rod/splint technologies spurred early efforts to devise plate and screw fixation systems. In 1888, Schede would report the first usage of formal plate fixation across the fracture site, in the form of a steel plate stabilized by four screws. In the early part of the 20th century, Mahe, Ivy and Cole experimented with a combination of plates made of either steel or silver, combined with screw and/or wire fixation to stabilize the fractures. These early plate designs were ultimately abandoned due to a significant incidence of infection and surrounding tissue corrosion.
Despite early setbacks, recognition of the merits of rigid fixation in the promotion of primary bone healing furthered ingenuity in the engineering, materials, and fabrication of these systems. An understanding that plate fixation in the dynamic craniofacial skeleton is a different entity to that of the extra-axial skeleton eventually made way for the development of a number of fixation technologies: rigid versus semi-rigid fixation, locking versus nonlocking plates, threaded versus tapered plates, and bicortical versus monocortical fixation. An in-depth familiarity with this diverse armamentarium is critical to the successful management of the spectrum of mandibular trauma. In the sections that follow we will discuss the anatomy, classification, diagnosis, work-up, and management of fractures of the mandibular angle, ramus, body, and symphysis, highlighting best practice recommendations.
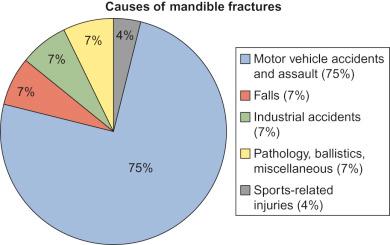
The causes of mandible fractures are diverse and include: motor vehicle collisions (MVCs), assaults, falls, sports- and industrial-related injuries, ballistic injuries, and pathologic fractures. Taking all-comers, approximately 75% of mandible fractures are caused by MVC and assault, 7% are due to falls, 7% and 4% are due to industrial- and sports-related injuries, respectively, and the remainder are due to pathological, ballistic, and other miscellaneous causes ( Fig. 1.14.1 ). The most common etiology is variable depending on the socioeconomic status of the patient and the population being examined. For example, in rural or developing countries, MVC remains the most common cause of mandibular trauma; whereas in certain urban settings of developed nations, assault and interpersonal violence can account for much of the mandibular trauma presenting to trauma centers.
An increasingly frequent and previously underrecognized cause of mandible fracture is pathological fracture associated with dental implantation. As indications for and access to restorative dentistry are ever-increasing, a wider range of patients are now the recipients of implant technologies and by extension at risk for unfavorable fractures. Greenstein et al. noted the following predisposing factors to implant-associated fractures: (1) poor bony stock (osteoporosis); (2) stress/strain at site of implant placement; and (3) trauma. An understanding of these risks and considerations for the management thereof are important for both the oral surgeon placing implants and the trauma surgeon who manages traumatic fractures in an increasing population of patients who may also have had dental rehabilitation.
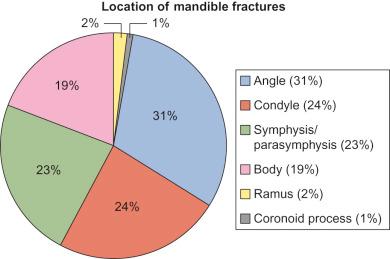
The incidence of mandible fractures by anatomical location is as follows: angle (31%), condyle (24%), symphysis and parasymphysis (23%), body (19%), ramus (2%), and coronoid process (1%) ( Fig. 1.14.2 ). In addition, a number of studies have looked at the association between causality and fracture location. In fractures secondary to MVC, the body is the most common site of injury. In those associated with assault the angle and body are most commonly involved. Boole et al. found that fractures after motorbike accidents most commonly involved the condyle or ramus.
When considering the incidence of concomitant facial fractures, 15% of individuals were found to have another facial fracture in addition to the mandible fracture. The number of fractures per mandible has also been analyzed retrospectively with a reported mean of 1.65. Several authors have extrapolated that between 40% and 50% of patients presenting with mandibular trauma have more than one fracture.
The surgeon managing complex mandibular trauma should also be versed in the risk of nonmaxillofacial trauma that can be associated with the mandibular fractures. The incidence of non-bony facial injuries has been reported to range from 15% to 34% in a review of UK and North American Trauma Databases, respectively. As expected, the mechanism of injury is an important predictor of the presence or absence of other injuries. Mandible fractures secondary to assault were most commonly isolated. In contrast, mandible fractures secondary to an MVC were associated with nonmaxillofacial injuries in 46% of patients reviewed. The risk of concomitant cervical spine injury has been reported to range from 2.6% to 6.5%. An understanding and appreciation for the mechanism of injury and the possibility of associated polysystem trauma is an important preoperative consideration for the trauma surgeon with respect to clearance and timing of fracture repair.
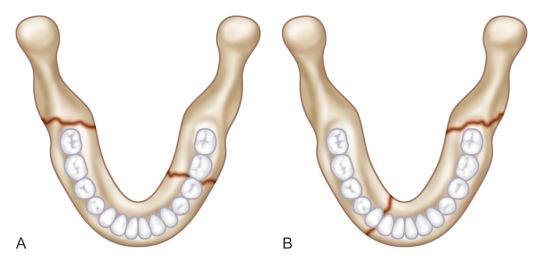
See Fig. 1.14.3 .
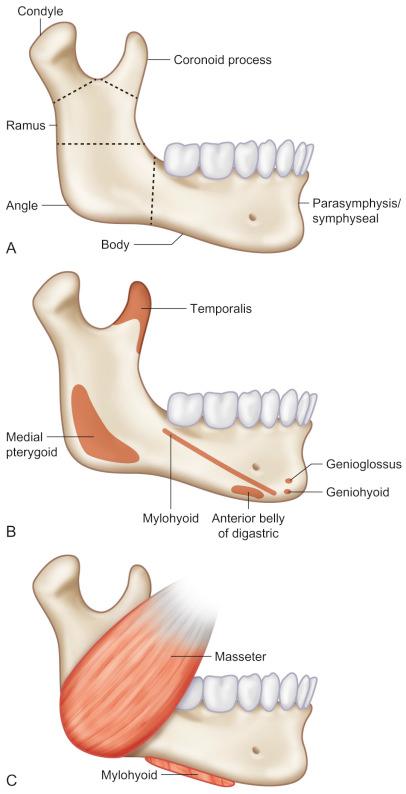
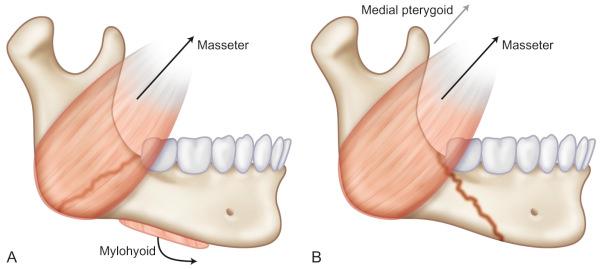
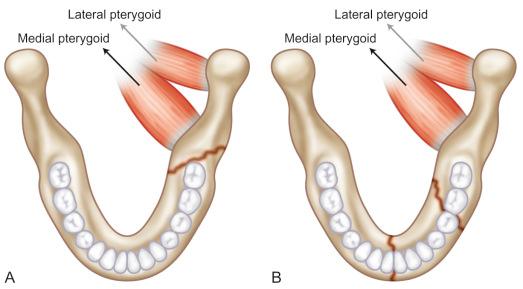
Though a myriad of classification schemes have been presented in the maxillofacial trauma literature, there is no single system globally accepted by practitioners by which to standardize communication. The most commonly referenced scheme is classification by anatomic region: symphysis, body, angle, ramus, condyle, coronoid, and alveolus. These anatomic units are often further subclassified into favorable and unfavorable patterns. Favorableness is determined by the direction of a fracture line when viewed on radiographs in the horizontal or vertical plane. The displacing forces of the muscles of mastication influence the favorableness of mandible fractures ( Fig. 1.14.4 ). Horizontally favorable fracture lines resist upward displacing forces. A vertically favorable fracture line resists the medial pull of the medial pterygoid on the proximal fragment when viewed in the vertical plane ( Fig. 1.14.5 ). The following defines each subunit by its anatomy and elucidates relevant favorable and unfavorable fracture patterns.
The symphyseal region of the mandible is defined as the region between the roots of the central incisors, running from the alveolar process through the inferior border of the mandible in a vertical orientation ( Fig. 1.14.6 ).

The parasymphysis region of the mandible is defined as the area between the lateral roots of the canines and the distal aspect of the lateral incisors, extending from the alveolar process to the inferior border of the mandible ( Fig. 1.14.7 ). Linear and oblique fracture orientations are characteristic in this region. The combined action of the digastric and suprahyoid muscles on a bilateral fracture can pull on the distal fragment inferiorly in an unfavorable fracture, placing the patient at risk of acute upper airway obstruction.
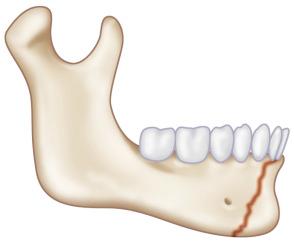
The body region of the mandible is defined as the line coincident with the anterior border of the masseter muscle to the canine. The buccal and lingual cortices of this area are well-defined. Fractures typically follow a linear pattern, however, in the incidence of high-energy trauma, comminution can be seen ( Fig. 1.14.8 ). Fractures of the body of the mandible are usually seen in combination with fractures on the contralateral side of the mandible or with ipsilateral fractures of the condyle or ramus.
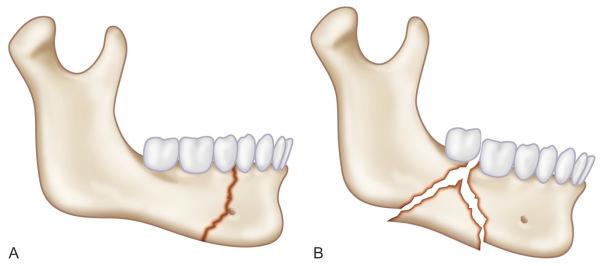
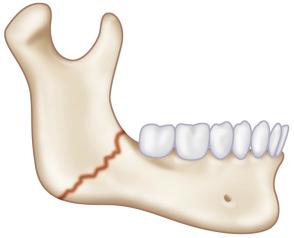
The angle region of the mandible is defined as a triangular area bounded by the anterior border of the masseter muscle to the posterosuperior attachment of the masseter muscle, usually distal to the third molar area. The angle of the mandible is thinner than the body of the mandible. Most fractures of the angle occur in the location of the third molar and extend to the antegonial notch anterior to the true angle. The masseter, temporalis, and medial pterygoid muscle attachments to the ramus cause displacement of the proximal segment of the angle of the mandible in a superior and medial direction when the fracture is horizontally and vertically unfavorable, respectively ( Fig. 1.14.9 ). Alternately, these muscles can serve to secondarily stabilize the proximal and distal bony segments in fracture patterns that are vertically and horizontally favorable. The more anterior a fracture occurs along the angle/body, the more the superior displacement of the fracture is counteracted by the pull of the mylohyoid muscle downward.
Combining the input and focus of a number of other classification schemes, Kruger presents a comprehensive four-category system ( Table 1.14.1 ).
| Relation to External Environment | Types of Fractures | Dentition of the Jaw With Reference to the Use of Splints | Localization |
|---|---|---|---|
|
|
|
|
The diagnostic work-up of mandible trauma starts with a thorough history. Special attention to past medical history may reveal previous trauma, bone disease, osteoporosis, neoplasms both primary and metastatic, pre-existing dental pathologies and interventions, nutritional and metabolic disorders, endocrinopathies, and psychiatric conditions that might influence both the etiology, timing of surgery, and choice of treatment stratagem for the relevant fracture. Preoperative temporomandibular joint (TMJ) dysfunction should be elucidated in the history and clearly documented in the preoperative evaluation if present, as it can have a profound impact on setting accurate patient expectations for postsurgical outcomes.
Ascertaining the velocity of the injury can help understand and predict the fracture patterns, as high- and low-speed impacts each manifest differently. As noted previously, assaults (low-velocity injuries) tend to cause isolated fractures, often nondisplaced, whereas high-speed MVCs are often associated with multiple fractures that are more likely to be displaced and comminuted.
The type of object also plays a role in the presenting fracture pattern. Blunt objects tend to cause multiple fractures due to the propagation and dispersion of forces throughout the jaw. Sharp or more well-defined objects isolate the injury forces to a single location within the jaw resulting in a localized comminuted fracture.
Similarly, the vector of injury forces often serves as a predictive indicator of the ultimate fracture profile. For example, traumatic forces directed anteriorly at the symphysis may result in associated bilateral condylar fractures and an anterior open-bite ( Fig. 1.14.10 ). Coup–contracoup patterns are often seen in high-velocity injuries when a force fracturing the parasymphysis may cause a concomitant contralateral angle fracture, and so forth ( Fig. 1.14.11 ).

Often overlooked and frequently underappreciated is the impact on surgical decision-making and outcomes of the patient's premorbid dental history and occlusion. The surgeon should be aware of any history of dental interventions, extractions (especially third molars), cosmetic and reconstructive dental rehabilitation, use of orthodontic appliances, significant carious and/or periodontal disease. Perturbations of the premorbid occlusion should be initially screened by asking if the patient feels that their bite is abnormal. If available, premorbid photographs can be reviewed to better elucidate the patient's baseline bite. In the patient who is completely or partially edentulous, the status of their dentures should be ascertained. For the patient engaged in phased orthodontic care, a preoperative discussion with the orthodontist may help guide treatment modalities.
The physical examination should consist of palpation and inspection. The four classic signs of inflammation, pain, swelling, redness and localized heat, are highly indicative signs of a mandible fracture. Fractured dentition, gingival bruising, lacerations, mobility of teeth, decreased incisal opening and malocclusion are common intraoral findings associated with mandible fractures. Alteration of sensation to the lower lip and chin is pathognomonic of a fracture of the mandible posterior to the mental foramen. However, nondisplaced fractures of the parasymphysis, body or angle rarely give rise to numbness in the distribution of the inferior alveolar nerve. Gingival tissue should be inspected for bruising or lacerations. Trauma causing bleeding, a hematoma, and discontinuity of skin or mucosa may indicate an injury to the underlying mandible. Sublingual ecchymosis is the most common pathognomonic sign of a fracture of the mandible, especially of the symphyseal, parasymphyseal or body regions. Depending on the direction and degree of displacement of a mandible fracture, the fractured segments can be visualized directly through the laceration. Forces that are strong enough to fracture or even loosen teeth have the ability to fracture the mandible. Fractured teeth should be evaluated along with any steps or irregularities within the dental arch. Missing teeth or fragments of teeth that have not been accounted for should be considered as swallowed, displaced into localized soft tissue, or aspirated. Abrasions, contusions, and lacerations of the gingiva and adjacent soft tissues should be examined for damage to vital structures. Mobility of fractured teeth should be assessed to determine risk of aspiration. Though alteration of occlusion can indicate displacement of teeth and fracture of dentoalveolar structures, it is highly suggestive of a mandible fracture. Changes in occlusion can be a result of fractures of the alveolar process, fractured teeth, mandible fracture, trauma to the muscles of mastication, temporomandibular joint effusion or dislocation. A posterior crossbite can be due to fractures of the parasymphysis region and condyle, causing bilateral splaying of the posterior mandible. An anterior open-bite with a posterior pre-mature contact can be indicative of an angle fracture, a condylar fracture or fracture of the maxilla. A posterior open-bite can indicate a fracture of the symphysis, parasymphysis, or alveolar process. Skin on the face of the affected area should be inspected for lacerations, hematoma and swelling, for example, a wound under the chin is a common site of laceration typically indicating symphyseal, parasymphysis, and/or subcondylar fractures. Asymmetries of a patient's face are indications of the possibility of a mandible fracture and abnormal facial contours of the mandible should be assessed. Bilateral parasymphysis fractures can cause a retruded chin. Bilateral body and subcondylar fractures can cause the downward displacement of the anterior mandible, leading to an elongated face. A fracture along the body or ramus of the mandible can lead to a flattened appearance on the lateral face.
Box 1.14.1 outlines the most common radiographic studies utilized in the diagnosis of mandible fractures. The panoramic radiograph (panorex) can be extremely useful in the initial evaluation of the patient with mandibular trauma. It is advantageous in that it allows a survey of all relevant anatomic subunits of the mandible in a single study, is comparatively cost-effective, and generally provides acceptable detail if taken by a skilled technician. There are several drawbacks, however, to this diagnostic approach: (1) panoramic radiography requires the patient to be upright or prone making this an unfeasible approach for most trauma patients; (2) medial condylar and buccal-lingual bony displacement is difficult to characterize; (3) resolution is poor when evaluating the symphysis, dentoalveolar arches, and the TMJ; and (4) though accessible in all dental, oral surgery, and orthodontic offices, the equipment is often not available in hospital-based radiology departments.
Panoramic radiograph
Caldwell posteroanterior
Lateral oblique
Mandibular occlusal view
Periapical view
Reverse Towne's view
Computerized tomography
Though panoramic radiography may not be readily available, most of the information on the location and vector of displacement can ultimately be garnered by a plain film mandible series inclusive of the following views: (1) Caldwell posteroanterior (PA) radiograph; (2) lateral oblique radiograph; (3) mandibular occlusal view; (4) periapical view; (5) reverse Towne's view. The advantage of the Caldwell PA is the clear demonstration of symphyseal fractures and the ability to discern medial or lateral displacement of fractures of the ramus, angle, body, and symphysis. The disadvantage of the PA view is that the condylar region is not well visualized. The lateral oblique view is easy to obtain and may be helpful in the diagnosis of angle, ramus, and posterior body fractures. The condylar, symphyseal, and premolar regions are often obscured. The occlusal view is helpful in determining the extent of medial and lateral displacement of body fractures. The reverse or modified Towne's view is helpful in elucidating the degree of medial displacement of the condyle. Anterior condylar displacement can be evaluated with transcranial TMJ views, although these are less often utilized by clinicians.
With the advent of helical computerized tomography (CT) offering better resolution, more expedient scan intervals, and decreased radiation exposure, trauma practice patterns have shifted to the more liberal utility of CT scanning in the evaluation of the polytrauma patient. Similarly, these practice patterns have been extended to include the evaluation of trauma within the craniomaxillofacial skeleton, and as such, helical CT with the addition of 3D reformatting has largely supplanted plain-film radiography as the diagnostic gold standard in the acute setting. CT of the craniofacial skeleton provides detailed resolution, and the ability to rapidly and accurately assess the fracture location, vector, and degree of displacement.
The indications dictating the chosen management strategy are best subdivided into nonoperative versus closed versus open reduction techniques ( Table 1.14.2 ).
| Closed Reduction | Open Reduction |
|---|---|
|
|
Nonoperative treatment of a mandible fracture with observation only and mechanical soft diet modification is considered in greenstick fractures or incomplete fractures without pain, functional disruption, malocclusion or pathology.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here