Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In the history of neurosurgery there have occurred a number of events and landmarks, and these will be the focus of this chapter. In understanding the history of our profession, perhaps the neurosurgeon will be able explore more carefully the subsequent chapters in this volume to avoid having his or her “hands cut off.”
To identify major trends and events in neurosurgery, this chapter has been organized into a series of rather arbitrary historical time periods. In each period the key themes, personalities, and neurosurgical techniques developed and used are discussed.
Neurosurgeons are often considered the second oldest profession, the first being prostitution. Early man (and woman) recognized that to take down a foe or an animal, a direct injury to the head was the quickest means. Having said that, prehistoric surgery, compared with its modern successor, lacked several essentials in its early development: an understanding of anatomy, recognition of the concept of disease, and comprehension of the origin of illness in an organic system. Failure to grasp these vital principles retarded the practice of both medicine and surgery. The “modern” art of surgery, and in particular that of neurosurgery, was not recognized as a discrete specialty until the early 20th century. Neurosurgeons have now advanced from mere “hole drillers” to sophisticated computer nerds running complex 21st-century stereotaxic frameless guided systems.
In many museum and academic collections around the world are examples of the earliest form of neurosurgery—skull trephination. A number of arguments and interpretations have been advanced by scholars as to the origin and surgical reasons for this early operation—to date no satisfactory answers have been found. Issues of religion, treatment of head injuries, release of demons, and treatment of headaches have all been offered. Unfortunately, no adequate archaeological materials have surfaced to provide us with an answer. In reviewing some of the early skulls, the skills of these early surgeons were quite remarkable. Many of the trephined skulls show evidence of healing, proving that these early patients survived the surgery. Fig. 1.1 shows examples of two early (Peru circa AD 800) skulls that have been trephined and show evidence of premorbid bone healing. In the Americas the tumi was the most common surgical instrument used to perform a trephination, and some examples of these tumis are shown in Fig. 1.1 . Fig. 1.2 presents a fine example of a well-healed gold inlay cranioplasty done by an early South American surgeon.


Included in many museum and private collections are examples of terra cotta and stone figures and other carvings that clearly depicted several common neurologic disorders. Commonly depicted by contemporary artisans were images of hydrocephalus, cranial deformation, spina bifida, and various forms of external injuries and scarring. We have added two examples from the Olmec and Mayan civilizations that demonstrate a young adult with achondroplasia and a young adult with severe kyphoscoliosis likely due to a myelomeningocele ( Fig. 1.3 ).

The Egyptian period, covering some 30 successive dynasties, gave us the earliest known practicing physician: Imhotep (I-em-herep) (3000 BC). Imhotep (“he whom cometh in peace”) is considered the first medical demigod, one likely more skilled in magic and being a sage. From this period came three important medical and surgical documents that give us a contemporary view of the practice of surgery. These collections are the Ebers, Hearst, and Edwin Smith papyri, two of which are considered here.
The Egyptians are well remembered for their skills developed in the practice of mummification. Historians have now shown that anatomic dissection was also performed in this period. An examination of the existing Egyptian papyri shows that the practice of medicine was based largely on magic and superstition. Therapeutic measures depended on simple principles, most of which allowed nature to provide restoration of health with little intervention. In treating skeletal injury, the Egyptians realized that immobilization was important and they prescribed splints for that purpose. Their materia medica was impressive, as their substantial pharmacopeias attest.
Written some 500 years after Hammurabi (1792–50 BC), and the oldest medical text believed to exist (including about 107 pages of hieratic writing), the Ebers papyrus is of interest for its discussion of contemporary surgical practice. The text discusses the removal of tumors and recommends surgical drainage of abscesses.
The Edwin Smith papyrus, written after 1700 BC, is considered to be the oldest book on surgery per se and is a papyrus scroll 15 feet in length and 1 foot in width (4.5 m by 0.3 m; Fig. 1.4 ). The text contains a total of 48 cases, including those with injuries involving the spine and cranium. Each case is considered with a diagnosis followed by a formulated prognosis. Owing to the scholarly work of James Breasted, this papyrus has been translated from the original Egyptian to English. The original document remains in the possession of the New York Academy of Medicine.
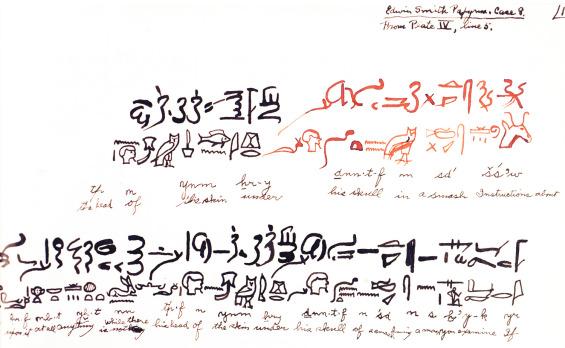
Other than the isolated cases found in these papyrus fragments, little can be gleaned on the actual practice of neurosurgery. However, it is evident from these papyri that the Egyptian physician could classify a head and spine injury and would even elevate a skull fracture if necessary. The Edwin Smith papyrus (ca. 1700 BC) offers the first descriptions of the skull sutures, the presence of intracranial pulsations, and the presence of cerebrospinal fluid (CSF). The use of sutures in closing wounds and the applications of specifically designed head dressings for cranial injury appear here for the first time. The Egyptian physician's understanding of the consequences of a cervical spine injury is clear from case 31, in which the injured individual is described with quadriplegia, urinary incontinence, priapism, and ejaculation in a cervical spine subluxation. The understanding of head and spine injury was further developed in the Greek schools of medicine; here we see the first treatment principles being offered on the management and codification of head injury.
The first formal development of neurosurgery occurred with the golden age of Greece. During the ancient period there were no surgeons who restricted themselves in stricto sensu to “neurosurgery.” Head injuries were plentiful then as the result of wars and internecine conflicts, as recorded by Herodotus and Thucydides as well as by Homer. The Greeks' love of gladiator sports also led to serious head injuries. So sports and war were then, as now, a principal source of material for the study and treatment of head injury.
The earliest medical writings from this period are those attributed to Hippocrates (460–370 BC), that most celebrated of the Asclepiadae, and his schools ( Fig. 1.5 ). To Hippocrates we owe the description of a number of neurologic conditions, many of them resulting from battlefield and sport injuries. Hippocrates was the first to develop the concept that the location of the injury to the skull was important in any surgical decision. The vulnerability of the brain to injury was categorized from lesser to greater by location, with injury to the bregma representing a greater risk than injury to the temporal region, which in turn was more dangerous than injury to the occipital region.

Hippocrates wrote on a number of neurologic conditions. From his Aphorisms is one of the earliest descriptions of subarachnoid hemorrhage: “When persons in good health are suddenly seized with pains in the head, and straightway are laid down speechless, and breathe with stertor, they die in seven days, unless fever comes on.”
Hippocrates provides the first written detailed use of the trephine. Insightful, he argued for trephination in brain contusions but not in depressed skull fractures (the prognosis was too grave) and cautioned that a trephination should never be performed over a skull suture because of the risk of injury to the underlying dura. Hippocrates demonstrated good surgical technique when he recommended “watering” the trephine bit while drilling to prevent overheating and injury to the dura.
Hippocrates had great respect for head injury. In the section on “Wounds of the Head,” Hippocrates warned against incising the brain, as convulsions can occur on the opposite side. He also warned against making a skin incision over the temporal artery, as this could lead to contralateral convulsions (or perhaps severe hemorrhage from the skin). Hippocrates had a simple understanding of cerebral localization and appreciated serious prognosis in head injury.
Herophilus of Chalcedon (fl. 335–280 BC) was an important early neuroanatomist who came from the region of the Bosporus and later attended the schools of Alexandria. Unlike his predecessors, Herophilus dissected human bodies in addition to those of animals—more than 100 by his own account. Herophilus was among the first to develop an anatomic nomenclature and form a language of anatomy. Among his contributions was tracing the origin of nerves to the spinal cord. He then divided these nerves into motor and sensory tracts. He made the important differentiation of nerves from tendons, which were often confused at that time. In his anatomic writings are the first anatomic descriptions of the ventricles and venous sinuses of the brain. From him comes the description of confluens sinuum or torcular Herophili. The first description of the choroid plexus occurs here, so named for its resemblance to the vascular membrane of the fetus. Herophilus described in detail the fourth ventricle and noted the peculiar arrangement at its base, which he called the “calamus scriptorius” because it “resembles the groove of a pen for writing.” Among his many other contributions was his recognition of the brain as the central organ of the nervous system and the seat of intelligence, in contrast to Aristotle's cardiocentric view.
All was not perfect with this anatomist, as Herophilus is also remembered for introducing one of the longest standing errors in anatomic physiology: the rete mirabile ( Fig. 1.6 ), a structure present in artiodactyls but not in humans. This structure acts as an anastomotic network at the base of the brain. This inaccurately described structure later became dogma and important in early physiologic theories of human brain function. The rete mirabile was later erroneously described in detail by Galen of Pergamon and further canonized by later Arabic and medieval scholars. Scholarship did not erase this anatomic error until the 16th century, when the new anatomic accounts of Andreas Vesalius and Berengario da Carpi clearly showed it did not exist in humans.
Entering the Roman era and schools of medicine, we come to Aulus Cornelius Celsus (25 BC to AD 50). Celsus was neither a physician nor a surgeon; rather, he can best be described as a medical encyclopedist who had an important influence on surgery. His writings reviewed, fairly and with moderation, the rival medical schools of his time: dogmatic, methodic, and empiric. As counsel to the emperors Tiberius and Gaius (Caligula), he was held in great esteem. His book, De re Medicina , is one of the earliest extant medical documents after the Hippocratic writings. His writings had an enormous influence on early physicians. So important were his writings that when printing was introduced in the 15th century, Celsus' works were printed before those of Hippocrates and Galen.
Celsus made a number of interesting neurosurgical observations. De re Medicina contains an accurate description of an epidural hematoma resulting from a bleeding middle meningeal artery. Celsus comments that a surgeon should always operate on the side of greater pain and place the trephine where the pain is best localized. Considering the pain sensitivity of dura and its sensitivity to pressure, this has proved to be good clinical acumen. Celsus provided accurate descriptions of hydrocephalus and facial neuralgia. Celsus was aware that a fracture of the cervical spine can cause vomiting and difficulty in breathing, whereas injury of the lower spine can cause weakness or paralysis of the legs, as well as urinary retention or incontinence.
Rufus of Ephesus (fl. AD 100) lived during the reign of Trajan (AD 98–117) in the coastal city of Ephesus. Many of Rufus' manuscripts survived and became a heavy influence on the Byzantine and medieval compilers. As a result of his great skill as a surgeon, many of his surgical writings were still being transcribed well into the 16th century. Rufus' description of the membranes covering the brain remains a classic. Rufus clearly distinguished between the cerebrum and cerebellum and gives a credible description of the corpus callosum. He had a good understanding of the anatomy of the ventricular system with clear details of the lateral ventricle; he also described the third and fourth ventricles, as well as the aqueduct of Sylvius. Rufus also provided early anatomic descriptions of the pineal gland and hypophysis, and his accounts of the fornix and the quadrigeminal plate are accurate and elegant. He was among the first to describe the optic chiasm and recognized that it was related to vision. The singular accuracy of Rufus' studies must be credited to his use of dissection (mostly monkeys) in an era when the Roman schools were avoiding hands-on anatomic dissection.
An individual of enormous influence was Galen of Pergamon (Claudius Galenus, AD 129–200). Galen was skilled as an original investigator, compiler, and codifier, as well as a leading advocate of the doctrines of Hippocrates and the Alexandrian school. As physician to the gladiators of Pergamon he had access to many human traumatic injuries.
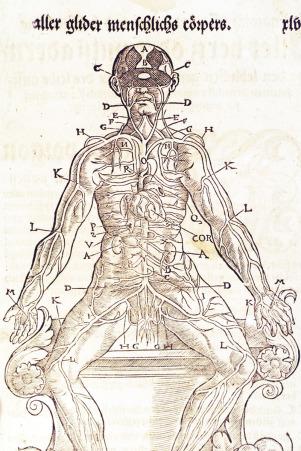
His experience as a physician and his scientific studies enabled Galen to make a variety of contributions to neuroanatomy. Galen was the first to differentiate the pia mater and the dura mater. Among his contributions were descriptions of the corpus callosum, the ventricular system, the pineal and pituitary glands, and the infundibulum. Long before Alexander Monro's Secundus (1733–1817) 18th-century anatomic description, Galen clearly described the structure now called the foramen of Monro. He also gave an accurate description of the aqueduct of Sylvius. He performed a number of interesting anatomic experiments, such as transection of the spinal cord, leading him to describe the resultant loss of function below the level of the cut. In a classic study on the pig, he sectioned the recurrent laryngeal nerve and clearly described that hoarseness was a consequence ( Fig. 1.7 ). Galen provides the first recorded attempt at identifying and numbering the cranial nerves. He described 11 of the 12 nerves, but by combining several, he arrived at a total of only 7. He regarded the olfactory nerve as merely a prolongation of the brain and hence did not count it.
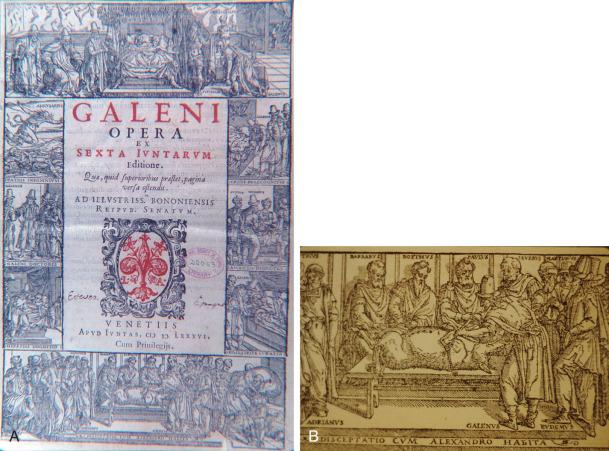
In viewing brain function Galen offered some original concepts. He believed the brain controlled intelligence, fantasy, memory, and judgment. This was an important departure from the teaching of earlier schools, for example, Aristotle's cardiocentric view. Galen discarded Hippocrates' notion that the brain is only a gland and attributed to it the powers of voluntary action and sensation.
With animal experimentation Galen recognized that cervical injury can cause disturbance in arm function. In a study of spinal cord injury, Galen detailed a classic case of what is today known as Brown-Séquard syndrome (ie, a hemiplegia with contralateral sensory loss in a subject with a hemisection of the cord). Galen's description of the symptoms and signs of hydrocephalus is classic. This understanding of the disease enabled him to predict which patients with hydrocephalus had a poorer prognosis. Galen was much more liberal in the treatment of head injury than Hippocrates, arguing for more aggressive elevation of depressed skull fractures, fractures with hematomas, and comminuted fractures. Galen recommended removing the bone fragments, particularly those pressing into the brain. Galen was also more optimistic than Hippocrates about the outcome of brain injuries, commenting that “we have seen a severely wounded brain healed.”
Paul of Aegina (AD 625–690), trained in the Alexandrian school, is considered the last of the great Byzantine physicians. He was a popular writer who compiled works from both the Latin and Greek schools. His writings remained extremely popular, being consulted well into the 17th century. Besides his medical skills Paul was also a skilled surgeon to whom patients came from far and wide. He venerated the teachings of the ancients as tradition required but also introduced his own techniques with good results. This author is best remembered for his classic work, The Seven Books of Paul of Aegina , within which are excellent sections on head injury and the use of the trephine. Paul classified skull fractures in several categories: fissure, incision, expression, depression, arched fracture, and, in infants, dent. In skull fractures he developed an interesting skin incision which involved two incisions intersecting one another at right angles, giving the Greek letter X. One leg of the incision incorporated the scalp wound. To provide comfort for the patient, the ear was stuffed with wool so that the noise of the trephine would not cause undue distress. In offering better wound care he dressed it with a broad bandage soaked in oil of roses and wine, with care taken to avoid compressing the brain.
Paul of Aegina had some interesting views on hydrocephalus, which he felt was sometimes a result of a man-handling midwife. He was the first to suggest the possibility that an intraventricular hemorrhage might cause hydrocephalus:
The hydrocephalic affection … occurs in infants, owing to their heads being improperly squeezed by midwives during parturition, or from some other obscure cause; or from the rupture of a vessel or vessels, and the extravasated blood being converted into an inert fluid … (Paulus Aeginetes).
An innovative personality, he designed a number of surgical instruments for neurosurgical procedures. Illustrated in his early manuscripts are a number of tools including elevators, raspatories, and bone-biters. An innovation for his trephine bits was a conical design to prevent plunging, and different biting edges were made for ease of cutting. Reviewing his wound management reveals some sophisticated insights—he used wine (helpful in antisepsis, although this concept was then unknown) and stressed that dressings should be applied with no compression to the brain. Paul of Aegina was later to have an enormous influence on Arabic medicine and in particular on Albucasis, the patriarch of Arabic/Islamic surgery.
From approximately AD 750 to AD 1200 the major intellectual centers of medicine were with the Arabic/Islamic and Byzantine cultures. As Western Europe revived after AD 1000, a renewed study of surgery and medicine developed there as well.
As we move out of the Byzantine period the Arabic/Islamic schools became paramount in the development of medicine and surgery. Thriving Arabic/Islamic schools undertook an enormous effort to translate and systematize the surviving Greek and Roman medical texts. Thanks to their incredible zeal, the best of Greek and Roman medicine was made available to Arabic readers by the end of the 9th century, an enormous contribution. Although a rigid scholastic dogmatism became the educational trend, original concepts and surgical techniques were clearly introduced during this period. In anatomic studies some of the more prominent figures actually challenged Galen and some of his clear anatomic errors.
Islamic medicine flourished from the 10th century through the 12th century. Among the most illustrious scholars/writers/physicians were Avicenna, Rhazes, Avenzoar, Albucasis, and Averroes. In the interpretative writings of these great physicians one sees an extraordinary effort to canonize the writings of their Greek and Roman predecessors. Islamic scholars and physicians served as guardians and academics of what now became Hippocratic and Galenic dogma. But having said this, there is clear evidence that these scholars and physicians continued original research and performed anatomic studies, a procedure not forbidden in either the Koran or Shareeh, a common Western view.
In reviewing this period, one finds that physicians rarely performed surgery. Rather, it was expected that the physician would write learnedly and speak ex cathedra from earlier but more “scholarly” writings. The menial task of surgery was assigned to an individual of a lower class—that is, to a surgeon. Despite this trend several powerful and innovative personalities did arise, and we will review their contributions.
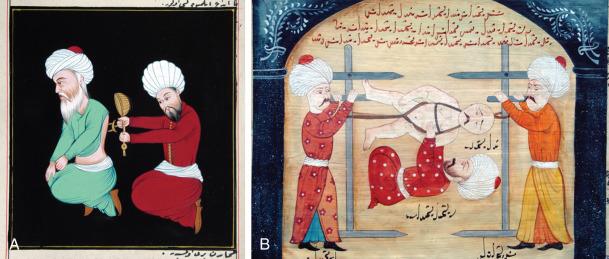
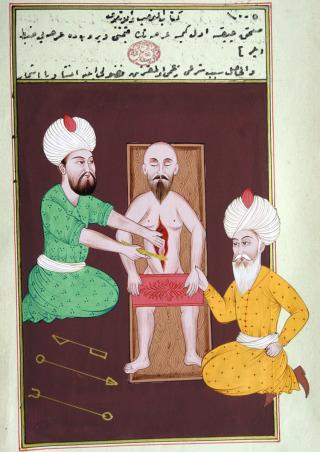
In this era of Islamic medicine we see introduced a now common medical tradition—bedside medicine with didactic teaching. Surgeons, with rare exceptions, remained in a class of low stature. One unfortunate practice was the reintroduction of the Egyptian technique of using a red-hot cautery iron, applied to a wound, to control bleeding. In some cases hot cautery was used instead of the scalpel to create surgical incisions, and this practice clearly led to a burned and subsequent poorly healed wound ( Fig. 1.8 ).
An important Islamic scholar of this period, as reflected in his writings, was Rhazes (Abu Bakr Muhammad ibn Zakariya' al-Razi, AD 845–925). Reviewing his works one sees clearly a scholarly physician, loyal to Hippocratic teachings, and learned in diagnosis. Although primarily a court physician and not a surgeon, he provided writings on surgical topics that remained influential through the 18th century. Rhazes was one of the first to discuss and outline the concept of cerebral concussion. Head injury, he wrote, is among the most devastating of all injuries. Reflecting some insight, he advocated surgery only for penetrating injuries of the skull as the outcome was almost always fatal. Rhazes recognized that a skull fracture causes compression of the brain and thereby requires elevation to prevent lasting injury. Rhazes also understood that cranial and peripheral nerves have both a motor and sensory component. In designing a surgical scalp flap one needed to know the anatomy and pathways of the nerves so as to prevent a facial or ocular palsy.
Avicenna (Abu ‘Ali al-Husayn ibn ‘Abdallah ibn Sina, AD 980–1037), the famous Persian physician and philosopher of Baghdad, was known as the “second doctor” (the first being Aristotle). During the Middle Ages his works were translated into Latin and became dominant teachings in the major European universities until well into the 18th century. With the introduction of the printed book it has been commented that his Canon (Q'anun) was the second most commonly printed book after the Bible. Avicenna disseminated the Greek teachings so persuasively that their influence remains an undercurrent to this day. In his major work, Canon Medicinae (Q'anun) , an encyclopedic effort founded on the writings of Galen and Hippocrates, the observations reported are mostly clinical, bearing primarily on materia medica ( Fig. 1.9 ). Avicenna's medical philosophy primarily followed the humoral theories of Hippocrates along with the biologic concepts of Aristotle. Within Avicenna's Canon (Q'anun) are a number of interesting neurologic findings, such as the first accurate clinical explanation of epilepsy, for which treatment consisted of various medications and herbals along with the shock of the electric eel. He describes meningitis and recognized it was an infection and inflammation of the meninges. It appears that Avicenna might have conducted anatomic studies inasmuch as he gives a correct anatomic discussion of the vermis of the cerebellum and the “tailed nucleus,” now known as the caudate nucleus. Avicenna introduced the concept of a tracheostomy using a gold or silver tube placed into the trachea and provided a number of innovative techniques for treating spine injuries and included some devices for stabilizing the injured spine. Avicenna also had some insightful thoughts on the treatment of hydrocephalus. He recognized that external hydrocephalus (fluid between the brain and dura) could be drained with low morbidity risk. However, true internal hydrocephalus was more dangerous to treat and best left alone or treated with herbals and medications. The Canon (Q'anun) was clearly his greatest contribution, along with his collation and translation of Galen's collected works, a book that remained a dominant influence until well into the 18th century.
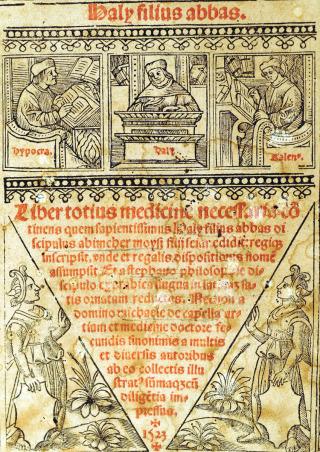
A personality often overlooked in neurosurgical history was a prominent Persian/Islamic physician by the name of Haly Abbas (Abdul-Hasan Ali Ibn Abbas Al Majusi) (?AD 930–44). This writer from the Golden Age of Islamic medicine produced a work called The Perfect Book of the Art of Medicine , also known as the Royal Book ( Fig. 1.10 ). Born and educated in Persia, a place he never left, it was here he produced his important writings on medicine. In his book he dedicated 110 chapters to surgical practice. A review of his work shows that his writings on spine injuries were essentially copied from the earlier Greek writers, in particular Paul of Aegina, and consisted mostly of external stabilization of spinal column injuries. Surgical intervention via a scalpel was rarely advocated. In his nineteenth discourse, Chapters 84 and 85, his management of depressed skull fractures is clearly presented. He also described the different types of fractures that can occur along with potential mechanisms of injury. He clearly appreciated that the dura should be left intact and not violated, the exception being those fractures where the skull bone had penetrated through the dural membrane, in which case these fragments needed to be removed. His technique of elevating a bone flap involved drilling a series of closely placed holes and then connecting them with a chisel. He showed some interesting consideration for the patient by advocating placing a ball of wool into the ears so as to block the sounds from the drilling. The head wound was then dressed with a wine-soaked dressing, the wine likely providing a form of antisepsis. These chapters also contain an interesting discussion about intraoperative brain swelling and edema, in which case the surgeon should look further for possible retained bone fragments and remove them. If later swelling occurred from too tight a head dressing, then it should be loosened. Unfortunately, Haly Abbas also advocated cephalic vein bleeding and inducing diarrhea for those who did not respond well; such primitive techniques were not to be abandoned until the mid-19th century.
In the Islamic tradition Albucasis (Abu al-Qasim Khalaf ibn al-Abbas Al-Zahrawi, AD 936–1013) was both a great compiler as well as a serious scholar, whose writings (some 30 volumes!) focused mainly on surgery, dietetics, and materia medica. In the introduction to his Compendium there is an interesting discussion of why the Islamic physician had made such little progress in surgery—he attributed this failure to a lack of anatomic study and inadequate knowledge of the classics. One unfortunate medical practice that he popularized was the frequent use of emetics as prophylaxis against disease, a debilitating medical practice that survived, as “purging,” into the 19th century.
The final section of the Compendium is the most important part for surgeons and includes a lengthy summary of surgical practice at that time. This work was used extensively in the schools of Salerno and Montpellier and hence was an important influence in medieval Europe. A unique feature of this text was the illustrations of surgical instruments along with descriptions of their use, which Albucasis detailed in the text. Albucasis designed many of the instruments, and some were based on those described earlier by Paul of Aegina. His design of a “nonsinking” trephine is classic (he placed a collar on the trephine to prevent plunging) and was to become the template of many later trepan/trephine designs ( Fig. 1.11 ).
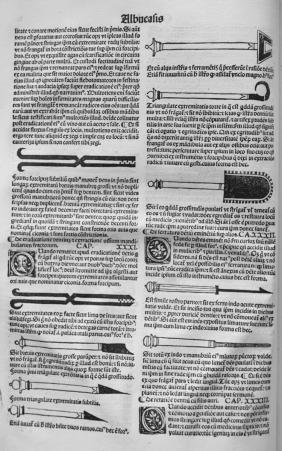
Albucasis' treatise on surgery is an extraordinary work—a rational, comprehensive, and well-illustrated text designed to teach the surgeon the details of each treatment, including the types of wound dressings to be used. Yet one can only wonder how patients tolerated some of the surgical techniques. For chronic headache a hot cautery was applied to the occiput, burning through the skin but not the bone. Another headache treatment required hooking the temporal artery, twisting it, placing ligatures, and then in essence ripping it out! Albucasis recognized the implications of spinal column injury, particularly dislocation of the vertebrae: in total subluxation, with the patient showing involuntary activity (passing urine and stool) and flaccid limbs, he appreciated that death was almost certain. Some of the methods he advocated for reduction of lesser spinal injuries, using a combination of spars and winches, were rather dangerous. With good insight he argued that bone fragments in the spinal canal should be removed. To provide comfort for the patient undergoing surgery he developed an “anesthesia” sponge in which active ingredients included opium and hashish; the sponge would be applied to the lips of the patient until the patient became unconscious.
For hydrocephalus (following the teachings of Paul of Aegina, he associated the disorder with the midwife grasping the head too roughly) Albucasis recommended drainage, although he noted that the outcome was almost always fatal. He attributed these poor results to “paralysis” of the brain from relaxation. With regard to the site for drainage, Albucasis noted that the surgeon must never cut over an artery, as hemorrhage could lead to death. In the child with hydrocephalus he would “bind” the head with a tight constricting head wrap and then put the child on a “dry diet” with little fluid—in retrospect a progressive treatment plan for hydrocephalus.
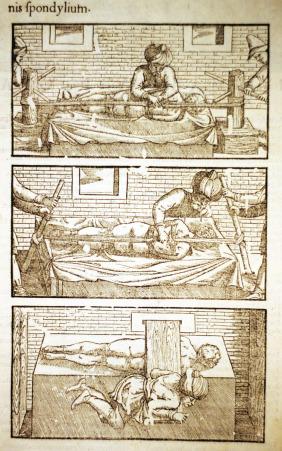
An important figure in the history of surgery, and one who bridged the Islamic and medieval schools, was Serefeddin Sabuncuoglu (1385–1468). Sabuncuoglu was a prominent Ottoman surgeon who lived in Amasya, a small city in the northern region of Asia Minor, part of present-day Turkey. This was a glorious period for the Ottoman Empire and Amasya was a major center of commerce, culture, and art. While working as a physician at Amasya Hospital, and at the age of 83, he wrote a medical book titled Cerrahiyyetü'l-Haniyye [Imperial Surgery] , which is considered the first colored illustrated textbook of Turkish medical literature. There are only three known copies of this original manuscript, two are in Istanbul and the third at the Bibliothèque Nationale in Paris. First written in 1465 the book consists of three chapters covering 191 topics, all dealing with surgery. Each topic consists of a single, poetical sentence in which the diagnosis, classification, and surgical technique of a particular disease are described in detail. This book is unique for this period in that virtually all the surgical procedures and illustrations were drawn in color, even though drawings of this type were prohibited in the Islamic religion ( Fig. 1.12 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here