Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A general rule for determining the size of the endotracheal tube (ET) in children is 4 + (age in years/4) for a cuffed tube and 3.5 + (age in years/4) for an uncuffed tube. It is generally safer to choose a smaller ET tube if the two tube sizes are debated.
Tracheostomy does not prevent chronic aspiration.
Inspiratory stridor with muffled voice and usually a lack of cough are symptoms of epiglottitis, a possible airway emergency. If the patient is stable, a lateral neck x-ray may demonstrate a “thumb sign,” indicating a swollen epiglottis.
Biphasic stridor with barking cough is consistent with subglottitis, or “croup.” An AP neck x-ray may demonstrate a “steeple sign,” indicating subglottic narrowing.
Significant bleeding from a tracheostomy should be taken seriously and investigated to rule out trachea-innominate fistula, a surgical emergency that carries a mortality rate of 73%.
A vertical incision can be used in newborns to decrease the risk of subglottic stenosis.
The trachea is the anatomic location in the head and neck with the highest rate of cocaine absorption.
A cuff pressure of 34 cm H 2 0 compromises capillary blood flow to the tracheal mucosa and causes pressure necrosis.
What are the steps in the management of an airway fire?
Turn off the oxygen flow
Douse fire with saline
Remove damaged tube
Reintubate as atraumatically as possible
Administer IV steroids and antibiotics
Perform bronchoscopy before leaving the OR to remove any charred tissue or other debris and evaluate the extent of airway injury
Delayed extubation with repeat endoscopic airway examinations
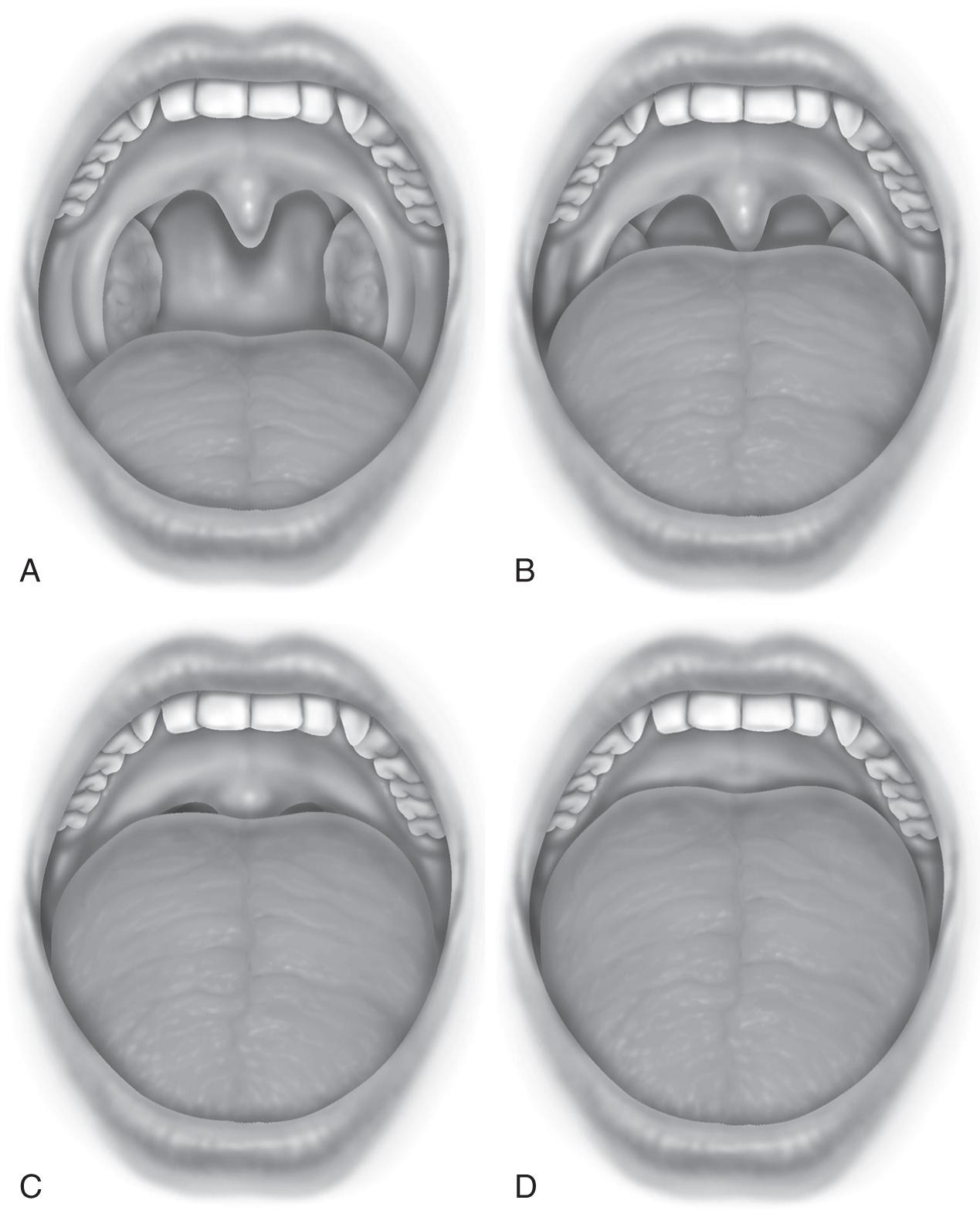
Friedman Palate Position ( Fig. 79.1 ):
Visualization of entire uvula and tonsils/tonsillar pillars
Visualization of the uvula but not tonsils
Visualization of the soft palate but not uvula
Visualization of hard palate only
Similarly, the Mallampati Score (more commonly used in anesthesiology):
Class I Soft palate, uvula, fauces, pillars visible
Class II Soft palate, uvula, fauces visible
Class III Soft palate, base of uvula visible
Class IV No soft palate visible
The higher the score, the more difficult exposure of the larynx may be during intubation.
The number refers to the inner diameter of the endotracheal tube. Thus a 5.0 ET tube will have an inner diameter of 5 millimeters, a 5.5 ET tube will have an inner diameter of 5.5 millimeters, and so on. The outer diameter of the ET tube can vary according to the material, manufacturer, and type of tube.
Cuffed tube = age 4 years + 3 years
Uncuffed tube = age 4 years + 4 years
This is generally accurate for children aged 1 through 12 years.
See Table 79.1 .
| AGE | ENDOTRACHEAL TUBE SIZE (MM) |
|---|---|
| Neonate | 2.5–3.0 |
| Infant, 1–6 months | 3.0–3.5 |
| Infant, 6–12 months | 3.5–4.0 |
| Toddler | 4.0–5.0 |
| Adult female | 6.0–7.0 |
| Adult male | 7.0–8.0 |
As a general rule, between two ET tube sizes, it is safer to put in a slightly smaller ET tube rather than one that is too large and difficult to pass. If ventilation is difficult with a small tube, some ventilation can be administered to stabilize the patient, and a tube exchanger can be used to change the ET tube, with a very low risk of losing the airway.
Cormack-Lehane Classification grades the view of the larynx during direct laryngoscopy:
Grade I Visualization of the entire glottis
Grade II Partial view of the glottis; may see only arytenoids
Grade III Visualization of the epiglottis only; none of the glottis is seen
Grade IV Not even the epiglottis is visible
Trachea – usually expiratory, occasionally inspiratory
Subglottis – biphasic stridor, barking cough, hoarse voice
Glottis – biphasic or inspiratory stridor, hoarse voice
Supraglottic – inspiratory stridor, muffled voice, inability to feed, no cough
Oropharynx/nasopharynx – stertor, muffled voice, or hyponasal voice
Chin lift with jaw thrust, oropharyngeal airway , and nasopharyngeal airway are anatomical manipulations that can help alleviate upper airway obstruction. The first two are generally used for unconscious patients. The latter is best used for patients with oral obstruction (i.e., trauma, Ludwig’s angina) or in neonates with nasal obstruction who are obligate nasal breathers. Heliox can be used to deliver oxygen in cases of airway obstruction. Heliox is a mixture of helium and oxygen and is a lower-density gas compared to room air or pure oxygen. This allows a higher flow rate, which reduces turbulent flow past an obstruction and delivers more oxygen distally to the lungs. This reduced turbulent flow also decreases the pressure gradient needed to move air across an obstruction, thus reducing airway resistance and breathing. Typical concentrations are 21%:79% oxygen to helium. Helium is inert, insoluble in human tissues, and noncombustible. Heliox is used as a temporizing measure while planning to perform a more definitive airway stabilization.
Racemic epinephrine – administered via nebulizer to cause vasoconstriction and reduce mucosal edema. Racemic epinephrine has been shown to help treat croup and postextubation stridor from laryngeal edema. Racemic epinephrine is not as effective for epiglottitis, and the practice of trying to administer it can be dangerous because agitation for these patients can cause acute obstruction by the swollen epiglottis.
IV steroids – glucocorticoids, such as dexamethasone, are used to reduce airway inflammation and edema. This is thought to occur through reduced capillary dilation, decreased plasma extravasation, and inflammatory mediator release. They are also indicated for croup and laryngeal edema and are often used for other causes of upper airway obstruction (i.e., abscess or other infectious edema, including epiglottitis and angioedema). IV steroids act gradually, unlike racemic epinephrine, which acts fairly rapidly.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here