Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Q36.1 What are the mechanisms by which intravenous immunoglobulin (IVIg) affects (1) antibody (Ab) production, (2) Ab neutralization, (3) the complement system, (4) T-cell activation, (5) immune cell trafficking, and (6) Fas/Fas ligand interaction? (Pg. 398)
Q36.2 What is the likelihood of success and unique risks when using IVIg for patients with severe, recalcitrant dermatomyositis? (Pg. 399)
Q36.3 What is the likelihood of success and unique risks when using IVIg for patients with severe, recalcitrant pemphigus? (Pg. 400)
Q36.4 What is the likelihood of success and unique risks when using IVIg for patients with severe, recalcitrant cicatricial (especially) ocular pemphigoid? (Pg. 401)
Q36.5 What is the likelihood of success and unique risks when using IVIg for patients with Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN)? (Pg. 401)
Q36.6 What is the rationale for ordering immunoglobulin levels for patients who are about to receive IVIg therapy? (Pg. 403x2)
Q36.7 Which categories of patients are at greatest risk for fluid overload with IVIg therapy? (Pg. 403)
Q36.8 What are the available options to reduce the risk of thromboembolism with IVIg therapy? (Pg. 403)
Q36.9 What are the most common regimens for IVIg therapy regarding: (1) dosage per kilogram, (2) duration of therapy per cycle, and (3) interval between cycles? (Pg. 404)
Q36.10 What is the typical cost range for a single cycle of IVIg using the two most common dosage regimens? (Pg. 404)
Q36.11 Overall, which conditions managed at least in part by dermatologists have the greatest evidence for efficacy of IVIg? (Pg. 404)
Atopic dermatitis
Adverse effects (events)
Bone marrow transplant
Bullous pemphigoid
Bullous pemphigoid antigen
Creatine phosphokinase
Drug reaction with eosinophils and systemic symptoms
Epidermolysis bullosa acquisita
Graft-versus-host disease
Intercellular adhesion molecule
Intravenous immunoglobulin
Linear IgA bullous dermatosis
Major histocompatibility complex
Mucous membrane pemphigoid
Pemphigus foliaceus
Pyoderma gangrenosum
Pemphigus vulgaris
Stevens–Johnson syndrome
Systemic lupus erythematosus
Toxic epidermal necrolysis
The editor would like to thank Anita Ruetter and Kai Thomas for their contribution to the previous edition of this chapter.
Since the 1960s, immunoglobulin products for intramuscular injection were developed to prevent and treat viral diseases as well as treat primary Ab deficiency syndromes. In the early 1980s, preparations for intravenous application allowed for a broader therapeutic use, including the administration of larger amounts of immunoglobulin.
Intravenous immunoglobulin (IVIg) is currently derived from a purified human plasma pool of more than 1000 healthy blood donors and contains IgG in supraphysiologic levels, including traces of other immunoglobulins. IVIg exerts a variety of immunomodulating activities and is currently used for the treatment of (1) primary and secondary immunodeficiency diseases, (2) autoimmune disorders, and (3) certain infectious diseases. The exact mechanisms responsible for the immunomodulating activity of IVIg are not yet completely understood and need to be further investigated.
In times of targeted therapies using biologicals, IVIg still plays an important role in the treatment of a wide variety of skin diseases. There is accumulating evidence that IVIg is an effective and safe treatment for various skin diseases, and thus its use may lead to a significant reduction in adjunctive therapy with immunosuppressive agents. Randomized double-blind, placebo-controlled trials have been published for dermatomyositis and pemphigus, and other dermatologic indications may follow. This chapter will summarize the currently available clinical experience with IVIg in the treatment of skin diseases. Wherever possible, a critical evaluation of IVIg efficacy and safety will be given for various indications.
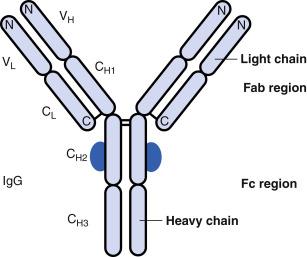
IVIg mainly consists of immunoglobulin (Ig)G, but also has small amounts of other immunoglobulins (IgA, IgE, IgM) and albumin, together with sugars, salts, and solvents. Exact concentrations depend on the individual manufacturers preparation (multiple products are available). Peak serum concentrations occur immediately after intravenous injection and are dose related. Within 24 hours, up to 30% of the dose may be removed by catabolism and distribution. IVIg distributes itself throughout the intravascular (60%) and extravascular (40%) spaces, crosses the placenta, and may be excreted into milk. The serum half-life is 2 to 5 weeks. Fig. 36.1 demonstrates the structure of IgG.
Q36.1 The complex spectrum of various mechanisms of action for IVIg is still not completely understood. One of the mechanisms first postulated was the suppression of Ab production by IgG binding via its Fc fragment to corresponding cellular surface receptors on B lymphocytes. This may result in the downregulation of pathogenic autoantibody production. Moreover, application of IVIg leads to a reduced half-life of circulating immunoglobulins, probably by saturating the protective neonatal Fc receptor (FcRn), and in this way causing an accelerated Ab catabolism.
IVIg also appears to function via the neutralization of complement-mediated effects. Accordingly, antibodies in IVIg preparations are capable of binding to complement components such as C3 and C5 convertases, and thereby block complement activation at an early stage. In addition, IVIg seems to interfere with the formation of the terminal membrane attack complex C5b–C9 (MAC).
Because IVIg preparations contain a diversity of immunoglobulins, there are ‘anti-idiotypic’ antibodies that can bind and neutralize pathogenic antibodies. After infusions of IVIg, a marked reduction or even disappearance of these antibodies could be demonstrated. Furthermore, there is evidence that IVIg binds to Fc receptors on macrophages, subsequently saturating, altering, or downregulating these receptors. This may lead to an inhibition of the autoantibody-mediated cellular activation and therefore suppresses cytokine production. In addition, the binding of antibodies to the inhibitory receptor FcγRIIB may lead to a modulation of the inflammatory activity.
In addition, there are implications of numerous effects on T-cell activation. IVIg preparations contain amounts of soluble CD4, CD8, MHC-I, and MHC-II molecules, which may have the ability to inhibit autoreactive T lymphocytes. A similar effect could be attributed to antibodies against the T-cell receptor Vβ chain. IVIg has been reported to downregulate the expression of costimulatory molecules such as lymphocyte function-associated antigen 1 (LFA-1) on activated T cells, interfering with T-cell activation. The presence of neutralizing Ab to cytokines, bacterial, and viral superantigens is able to attenuate the specific and nonspecific activation of T cells. Another possible mechanism of action of IVIg is the restoration of a T helper (Th)1/Th2 cytokine balance by supplying neutralizing antibodies.
IVIg may affect the migration of immunocompetent cells from blood to the target tissue. Antibodies against the extracellular matrix protein Arg-Gly-Asp may inhibit the cellular adhesion and subsequent cellular migration, and thereby modify the local inflammatory response.
IVIg also contains anti-Fas-receptor Ab, which is able to block molecular Fas ligand/Fas receptor interactions and consequently keratinocyte apoptosis. This mechanism seems to play a vital role in the therapy of Stevens–Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN) with IVIg. Findings suggest that IVIg can modulate the cellular proliferation of activated T and B lymphocytes and induce selective apoptosis, thereby altering overall immune responses.
In a wide range of dermatologic diseases, the adjunctive use of IVIg has led to reduced dose requirements for systemic corticosteroid (CS). This was because of the increased glucocorticoid receptor sensitivity, and because IVIg and CS can synergistically suppress the lymphocyte activation.
Box 36.1 lists indications for IVIg and Box 36.2 presents the ‘risk profile’ for IVIg.
| Dermatologic uses |
|---|
Vascular Diseases
Autoimmune Connective Tissue Disorders
Autoimmune Bullous Dermatoses
|
Other Inflammatory Dermatoses
Other Dermatoses
|
DRESS, Drug Rash with Eosinophilia and Systemic Symptoms.
| Contraindications | |
|
|
| Boxed Warnings | |
|
|
| Warnings & Precautions a | |
Renal
Hypersensitivity Reactions
Cardiovascular & Pulmonary
|
Hypercoagulability
Hematologic
Miscellaneous
|
| Pregnancy Prescribing Status | |
|
|
a Under “Warnings & Precautions” these adverse effects can be considered relatively high risk or important clinical scenarios to avoid.
b See Chapter 65 Dermatologic Drugs During Pregnancy and Lactation, for detailed explanations of terms for “Newer rating” based on 2015 US Food and Drug Administration rulings.
AKI, Acute kidney injury; IgA, immunoglobulin A.
Data from Facts & Comparisons eAnswers (online database). St. Louis: Wolters Kluwer. (https:// www.wolterskluwercdi.com/facts-comparisons-online/
Kawasaki disease is an acute febrile multisystem vasculitis syndrome of unknown etiology that occurs in infants and children. The disease primarily involves medium and large arteries, and thus represents one of the leading causes of acquired heart disease in children, because of the risk of coronary artery aneurysms. Clinical and epidemiological data support an infectious cause; many bacterial and viral agents have been implicated. A role of IgA-producing cells within the vascular wall has also been suggested. The acute stage of Kawasaki disease is characterized by fever, conjunctivitis, mucocutaneous inflammation, and cervical lymphadenopathy. Thus, it is associated with an uncontrolled activation of the immune system, including immunocompetent cells, cytokines, autoantibody production, and adhesion molecule expression.
Clinical studies have demonstrated that IVIg together with aspirin (acetylsalicylic acid) given within the first 10 days of illness (as early as possible) leads to a significant reduction in the frequency of coronary artery abnormalities. The current recommendations for the treatment of Kawasaki disease suggest IVIg as a single 2 g/kg infusion over 8 to 12 hours in combination with aspirin (30–100 mg/kg per day) as first-line therapy. IVIg seems to block Fc receptors, neutralize autoantibodies and bacterial superantigens, and modify cytokine production. However, it should be remembered that despite treatment, cardiovascular sequelae and lack of disease responsiveness can occur.
Of note, IVIg might be used as a treatment in other forms of severe vasculitis. In 1995, a small study of 15 patients (poor response to conventional immunosuppressive therapy) with granulomatosis with polyangiitis (GPA, formerly known as Wegener granulomatosis) showed a significant effect in 6 of 15 patients, but none of these patients was in complete remission after IVIg. Recently, other studies were able to demonstrate a clinical benefit of IVIg therapy.
Also, patients with eosinophilic granulomatosis with polyangiitis (EGPA, formerly known as Churg–Strauss syndrome) experienced an improvement after IVIg.
Livedoid vasculopathy is a chronic, recurrent vasculopathy characterized by thrombotic occlusion of the cutaneous capillaries of the distal lower extremities. Patients report severe pain and often show livedoid skin changes, recurrent superficial leg ulcers, and atrophie blanche. Current treatment strategies involve an effective anticoagulation, with low molecular weight heparin (enoxaparin) or anti-Xa-inhibitors (rivaroxaban, others). Also, IVIg was shown to have a positive effect on the clinical symptoms (ulcers and pain). Thus, IVIg can be considered as a treatment of livedoid vasculitis in refractory cases.
Dermatomyositis is an idiopathic autoimmune myopathy with characteristic cutaneous manifestations, including heliotrope rash, Gottron papules, periungual telangiectasia, scaling scalp with alopecia, and erythema or poikilodermatous skin changes. Muscle weakness is present in >90% of the patients and esophageal involvement with dysphagia or aspiration can also occur. In some patients, dermatomyositis is observed to be associated with malignancy, particularly ovarian and breast cancer in female patients, and colorectal and lung cancer in male patients. A further characteristic feature is the occurrence of myositis-specific Ab as well as elevated serum levels of creatine phosphokinase (CPK).
Q36.2 Treatment of dermatomyositis may be difficult as patients may become resistant or intolerant to standard regimens, including CS in combination with various immunosuppressive agents (azathioprine or methotrexate as first-line options, and rituximab, cyclosporine, mycophenolate mofetil, or cyclophosphamide as second-line options). Dermatomyositis is one of the best-studied indications for IVIg treatment, with published class 1 evidence. Current treatment concepts suggest using IVIg as an effective second-line therapy, particularly for patients with refractory disease incompletely responding to CS and for patients with life-threatening disease (suffering from dysphagia with a risk for aspiration). In a double-blind, placebo-controlled crossover study, a total of 15 patients with therapy-resistant dermatomyositis received either IVIg 2 g/kg per day for 2 days or placebo. Treatment with IVIg resulted in a significant improvement in muscle strength, neuromuscular symptoms, and skin involvement. In addition, there was a decrease in (1) serum CPK levels, (2) muscular intercellular adhesion molecule 1 (ICAM-1), (3) major histocompatibility complex (MHC) class I expression, (4) transforming growth factor (TGF)-β production, and (5) immune complex deposition in the intramuscular capillaries. Numerous trials and case reports indicate a remarkable clinical improvement after monthly IVIg infusions. Concomitant administrations of immunosuppressive agents could be significantly reduced. The successful use of IVIg for pregnant women with dermatomyositis and for children with juvenile dermatomyositis has been reported underlining the safety of the treatment.
Of note, dermatomyositis can also occur without muscle involvement (amyopathic dermatomyositis), which is often difficult to treat. First-line treatments include topical therapy (photoprotection, topical CS, topical calcineurin inhibitors) and systemic treatments (methotrexate, hydroxychloroquine). As a second-line treatment for refractory cutaneous dermatomyositis, IVIg therapies were shown to be effective.
For polymyositis, controlled clinical trials for IVIg are still lacking, although open studies demonstrated a benefit for patients.
Scleroderma is a chronic autoimmune disease affecting the microvasculature and connective tissue of multiple organ sites, and is characterized by fibrosis and obliteration of blood vessels in the skin. It may occur in a localized form (morphea, linear scleroderma) or as a systemic sclerosis (diffuse cutaneous, limited cutaneous) with multiple organ involvement. In systemic sclerosis, different autoantibodies can be found (antitopoisomerase I [Scl 70], anticentromere [ACA], or anti-RNA-polymerase I, II, or III).
Treatment with immunosuppressive agents is difficult and the disease often shows a progressive course. According to open-label studies and case reports, treatment with 2 g/kg of IVIg on a monthly basis in patients with scleroderma resulted in an improvement in joint and muscle involvement, skin scores, and gastrointestinal symptoms.
Scleromyxedema is a severe connective tissue disease, characterized by a generalized skin thickening caused by fibrosis and mucinosis, and is associated with monoclonal gammopathy in more than 90% of sufferers. A cutaneous finding in addition to the skin thickening is lichenoid papules, especially in the face, neck, hands, forearms, trunk, and thighs. The glabella shows typically deep longitudinal furrows. As it is a systemic disease, sclerosis of kidney and coronary arteries, lung fibrosis, polyneuropathies, arthralgias, and gastrointestinal motility dysfunctions can occur.
Treatment of this rare, chronic disease is difficult and CS, cyclophosphamide, plasmapheresis, melphalan, and thalidomide are suggested.
According to current guidelines, IVIg can be used to treat severe cases of scleromyxedema. Although no randomized trials have been performed, some small case studies showed a significant clinical improvement and even a complete remission after therapy with IVIg. Of note, continued IVIg therapy seems to be necessary to remain in remission.
Pemphigus vulgaris (PV) is a potentially fatal mucocutaneous autoimmune disease. It is characterized by an eruption of flaccid blisters that rupture easily, resulting in painful erosions. Involvement of the mucous membranes is very common. Autoantibodies in patients with PV target desmosomal cadherins, especially desmoglein 3 and, less commonly, desmoglein 1. Sera of patients contain circulating Ab to one or more keratinocyte cell surface antigens, and frequently the Ab titer correlates with disease activity. Patients with pemphigus foliaceus (PF) develop superficial blisters. The target antigen for PF is desmoglein 1, which is predominantly expressed in the upper layers of the epidermis of the skin, but not in the mucous membranes, thus only a cutaneous involvement is typically seen.
Q36.3 Treatment strategies include CS, usually in combination with other immunosuppressive agents. Recently, a randomized double-blind trial for IVIg in pemphigus showed significantly reduced disease activity in the treatment group treated with 400 mg/kg per cycle. Other reports suggest that the use of IVIg (1–2 g/kg per cycle) for the treatment of PV has been promising. In the majority of patients, a favorable response has been reported, allowing for a reduction or withdrawal of the concomitant immunosuppressive therapy. This ultimately resulted in a decreased rate of immunosuppressive drug-related adverse effects (AE). However, a recent study reported that the best results in lowering pemphigus Ab are obtained by combining IVIg and immunosuppressive drugs. In an open-label study, 9 of 11 patients with refractory PV treated with both IVIg and rituximab showed rapid resolution of lesions. Further studies are required to better define dosage, duration, and mechanism of action of IVIg in pemphigus treatment.
Bullous pemphigoid (BP) is characterized by large tense blisters that frequently occur on flexural surfaces of the extremities, axillae, groin, and abdomen. Mucosal lesions are found in 10% to 30% of the patients. The disease usually develops in the elderly; the patients often report an intense pruritus and occasionally BP occurs in association with malignancy. Subepidermal blister formation is caused by autoantibodies directed against two hemidesmosomal antigens, BP antigen 1 (BPAg1, also known as BP230 or dystonin) and BP antigen 2 (BPAg2, also known as BP180 or type XVII collagen).
Conventional treatment consists of CS (topical or systemic) in combination with immunomodulative (tetracyclines and dapsone) or immunosuppressive drugs such as azathioprine, cyclophosphamide, methotrexate, chlorambucil, cyclosporine, and mycophenolate mofetil. In severe cases, rituximab is appropriate. Controlled trials for the efficacy of IVIg in BP are still lacking, but several clinical studies and case reports including pediatric patients have been published. IVIg treatment in case reports was given every 4 weeks at a dose of 2 g/kg per cycle, with a significant reduction in the number of relapses and recurrences observed. Moreover, a significant decrease in autoantibody titers to both BPAg1 and BPAg2 resulted during treatment with IVIg. Overall, IVIg seems to be a promising approach for the treatment of BP, especially in patients not responding to conventional therapy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here