Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Several fundamentals of perioperative care for shunt-dependent dual-distribution circulation (see Chapter 70 ) extend to transitional care from the intensive care unit and throughout the interstage period in an effort to preserve organ function and promote somatic growth. Conventional outpatient surveillance limited to vital signs and routine growth assessment has historically been associated with high interstage mortality rates after discharge from Norwood or stage I palliation and prior to stage II palliation. (For the purposes of this chapter, stage II palliation refers to the general concepts of a superior cavopulmonary connection, the specific type of which depends on the individual patient's anatomy and surgical preference.) Interstage programs that leverage engagement of families and providers for vigilant monitoring of physiologic variances has led to improved interstage survival. The initial report of interstage monitoring noted a reduction of interstage death with a sustained single-center interstage survival rate for infants discharged to home of 98% over a 10-year period. Over the past 15 years, the unanticipated benefits of interstage monitoring have included improvement in somatic growth and less arbitrary timing of stage II palliation. Additional value has been the growing collaboration between numerous health care disciplines and parent advocates for the sole purpose of not only improving survival but also quality of life for infants born with hypoplastic left heart syndrome and related variants.
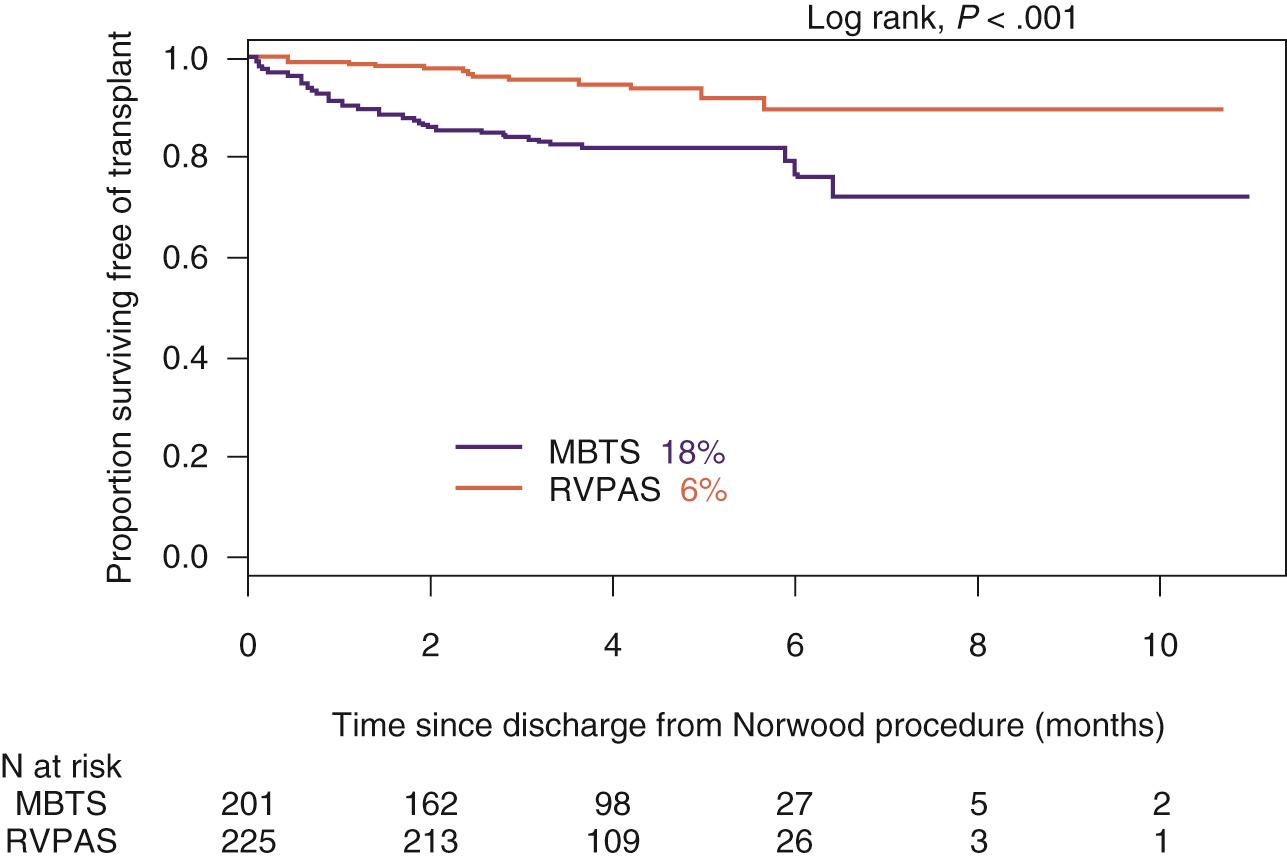
A variety of mechanisms have been proposed for infant demise during the first interstage period. Some single-center reports have identified nonmodifiable risk factors such as anatomic subtype including aortic atresia/mitral atresia and possibly aortic atresia/mitral stenosis, although larger single-center and multicenter investigations have failed to link anatomic subtype to interstage mortality other than an independent association between aortic atresia/mitral atresia as noted in the Pediatric Heart Network Single Ventricle Reconstruction trial. Potentially modifiable cardiac risk factors linked to interstage mortality include the presence of a restrictive atrial communication, neoaortic arch obstruction, obstruction of the systemic to pulmonary artery shunt, pulmonary artery distortion, atrioventricular valve insufficiency, and the presence of arrhythmias. Interstage mortality for patients in the Pediatric Heart Network Single Ventricle Reconstruction trial was significantly higher in those patients palliated with a modified Blalock-Taussig-Thomas shunt compared with the right ventricle to pulmonary artery (Sano) conduit (18 vs. 6%, P < .001) ( Fig. 72.1 ). Noncardiac risk factors associated with interstage mortality include commonly acquired gastrointestinal losses, respiratory illnesses, and/or feeding difficulties. Any of the mentioned processes may influence systemic vascular resistance, potentially lead to progressive hypoxia and/or shock (hypovolemia or cardiogenic), and, in the presence of limited myocardial reserve inherent to shunt-dependent dual-distribution circulation after stage I palliation, place infants at greater risk for serious morbidity and death regardless of their apparent physiologic reserve early after initial palliation.
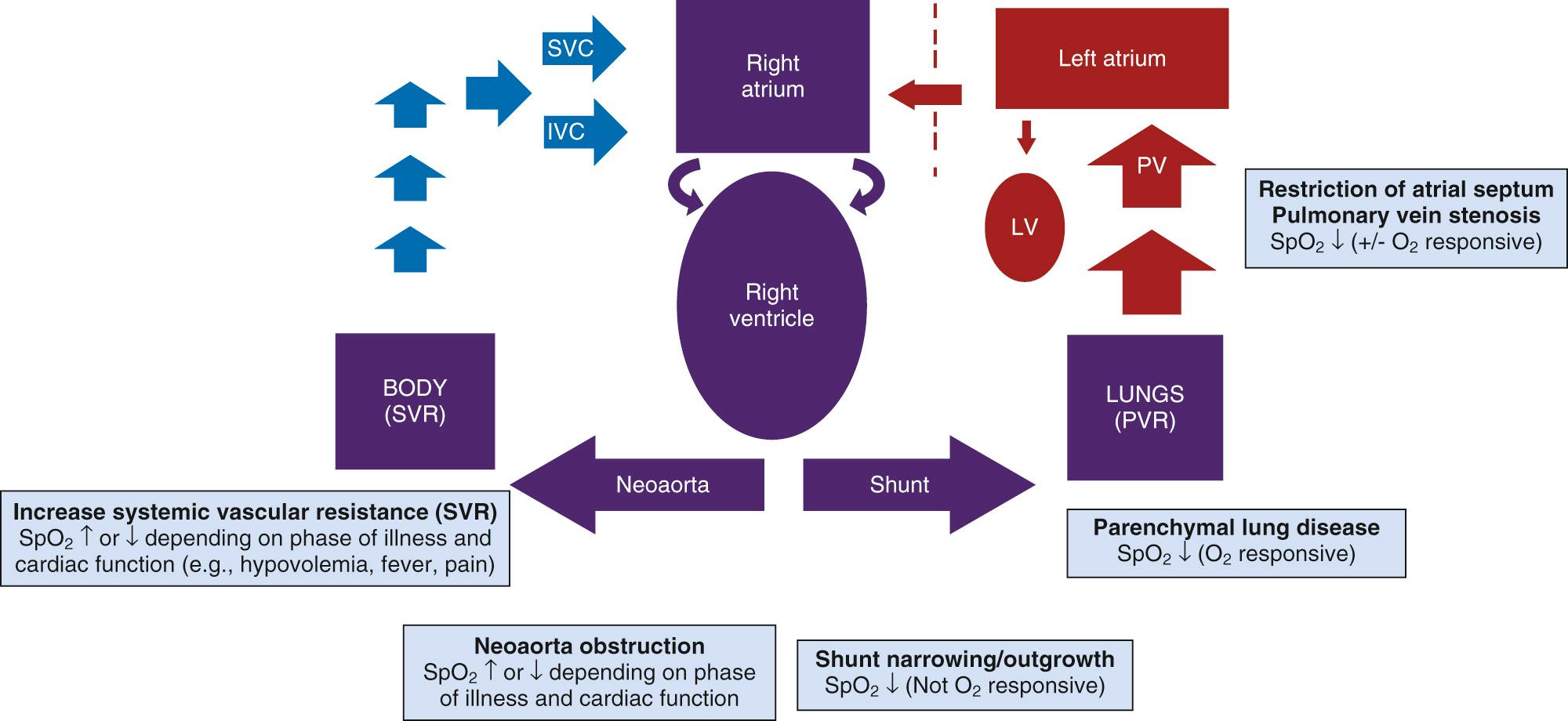
Monitoring within the medical home environment necessitates technology that is reliable, accessible, and easy to use, which led to the selection of pulse oximetry as the primary physiologic monitor. In infants with a dual-distribution circulation, desaturation from baseline may be indicative of limited pulmonary flow from myocardial dysfunction, shunt obstruction or outgrowth, anemia, or an acute illness leading to pulmonary venous desaturation. Alternatively, saturations higher than baseline may also be indicative of progressive disease that leads to escalation in systemic vascular resistance and hence increased pulmonary blood flow such as mild dehydration. These clinical scenarios have guided triage parameters for home monitoring of oxygen saturations ( Fig. 72.2 ). Specifically, arterial saturation less than 75% or greater than 90% warrants consideration for evolving pathology.
Daily assessment of infant weight with a digital scale sensitive to 10 g was initially adopted as part of the interstage monitoring program to earlier detect mild dehydration due to inadequate oral intake (less than 100 mL/kg per day) or excessive gastrointestinal losses. Consensus-driven criteria for assessment by a health care provider was set at weight loss of 30 g or failure to gain 20 g of weight over 3 days. Interestingly, breach of weight criteria was less commonly due to dehydration from gastrointestinal losses and more commonly associated with inadequate enteral intake, with volumes less than 100 mL/kg per day in nearly half the patients who breached weight criteria.
Early experience with interstage monitoring of weight trends highlighted growth failure that was associated with functionally univentricular heart. The growth failure can be attributed to a variety of factors that lead to inadequate enteral intake such as heart failure, genetic or extracardiac anomalies, gastrointestinal dysmotility, and/or malabsorption. Although some of the contributing factors are not modifiable, ensuring adequate nutrition in the presence of these comorbidities is an essential function of interstage monitoring and important for more health maintenance and outcomes at stage II palliation, the superior cavopulmonary connection. Multiple studies have shown that poor growth velocity and lower weight-for-age z -score at stage II palliation predicts a more complex postoperative course.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here