Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Nerves can be seen in computed tomography (CT) scans and in routine magnetic resonance imaging (MRI) scans. However, because they are similar in size, shape, and location to other structures such as blood vessels and lymphatics, they cannot be identified reliably at all locations along their length unless specialized tissue-specific imaging strategies are applied. The optimal strategies provide both definitive identification of a nerve at any point along the nerve and also demonstrate pathology based on an intrinsic image signal from the nerve itself.
The basis for tissue-specific MRI of nerve derives from the existence of a variety of unique types of tissue water in nerve. The three major types of neurographic techniques that have been described are diffusion neurography, diffusion tensor tractography–neurography, and T2-based neurography. It is conventional to use the term tractography for neural tracts in the brain and spinal cord, and to use the term neurography for peripheral nerve; however, peripheral nerve tractography is an appropriate description when the nerve images are based on assembling and linking calculated vectors rather than on direct image intensity measurements.
Diffusion neurography and the closely related diffusion tensor tractographic technique were the first methods reported. These methods have extremely high selectivity for nerves and should be very sensitive to a variety of types of more subtle pathology. Technical demands necessary to perform diffusion neurography delayed their clinical application ; however, diffusion tensor imaging (DTI) and tractography are increasingly important in clinical nerve imaging. While diffusion images tend to degrade in detail at locations of more severe pathology, they provide a critical additional assessment of function along with the structural data from T2-neurography in a wide variety of clinical applications.
T2-based neurography, however, can be applied on a reliable basis on many existing top-quality clinical scanners with minor modifications. , Even when the technical equipment requirements can be met, there may be limitations on the provision of MR neurography because of the lack of expertise in prescribing, postprocessing, interpreting, and acting upon the MR data. Once technical limitations are resolved, however, T2 neurography has the advantage of improving in quality of detail as the severity of the nerve abnormality increases, which is not always the case with diffusion-based neurography–tractography techniques. Although 3 T MRI scanners provide improved signal-to-noise and spatial resolution when configured properly, these images are far more sensitive to a variety of artifacts that degrade the image, which do not occur at 1.5 T.
Neural tissue is among several tissues in the body that demonstrate the property of linearly correlated water diffusion. Instead of diffusing freely in any direction (isotropic diffusion), the water molecules in neural tissue are restricted in their diffusion so that they tend to move in a directed fashion along the main longitudinal axis of the neural tissue (anisotropic diffusion). The detailed biophysical basis of this restricted diffusion is still not fully understood because water molecules should move freely through cell membranes.
In diffusion-based imaging, tissue contrast arises because it is possible to use the relative degree of diffusional isotropy and anisotropy in a given tissue to affect the rate of signal decay in that tissue. MR images can be sensitized to anisotropy by applying magnetic field gradients during the pulse sequence of the image acquisition process. When diffusion carries a proton to a new position in the gradient, it experiences a slightly different local magnetic field strength, and so its spin rate changes, resulting in desynchronization of the spins. When water diffuses equally in all directions in a tissue, the rate of this cause of signal decay is not affected by how the gradient is oriented.
When there is anisotropic diffusion, however, there is a large impact on the decay rate if the gradient is directed strictly perpendicular or strictly parallel to the direction of the nerve. When the uniform components of the gradient are perpendicular to the nerve and the slope of the gradient is parallel to the nerve (progressing from strong to weak along the length of the nerve), the nerve protons move rapidly to new positions in the gradient and their signal decays more rapidly than in an isotropic tissue. When the reverse is true, then the protons stay in the same field strength region of the gradient as they diffuse along the longitudinal axis of the nerve and they show little or no signal decay relative to surrounding isotropic tissues.
When a strong diffusion gradient is applied in the appropriate direction, along with fat suppression and heavy T2 weighting, it is possible to produce a relatively pure nerve image. This is a method that has been applied to produce whole-body neurography images. ,
For both peripheral and central nervous system (CNS) neural tissue, Filler and colleagues pointed out that it was possible to measure each voxel (three-dimensional pixel) in an image volume using three or more gradients in order to calculate both the magnitude and the direction in the three-dimensional space of the anisotropy. These two data components could then be used to depict actual curving neural tracts, rather than to simply display two-dimensional contrast differences in cross section. When six or more gradient directions are used, the vector processing can be accomplished using a tensor model, and the result becomes very robust across any curve or angle of progression. Vector models are used with as many as 256 directions of data acquisition. The end result is to determine the orientation of the primary characteristic vectors (eigenvector in tensor models) in a voxel. This can be done to determine more than one axonal direction in a voxel (crossing fibers) when large numbers of acquisition directions are used in vector methods.
Until this technologic development took place, the relative amount of apparent diffusion had been used as a signal intensity to assign contrast to a given image pixel in a cross section or to assign colors to regions of neural tissue that responded to a given gradient direction. In tractography, however, each voxel can be represented by an arrow that is a vector in three-dimensional space that provides a summary estimate of the main direction of the complex tensor that describes the entire pattern of diffusion in the nerve. The arrow also has a magnitude that encodes the degree to which water in that voxel is diffusing in an anisotropic fashion relative to isotropic diffusion.
When the arrows are followed from voxel to voxel, the result is a linear tract image that moves through the three-dimensional volume of the tissue, following the course of the neural tissue. A variety of three-dimensional computer graphic techniques are now used to assemble tractographic images from these linear anisotropy traces. This is the basis of tractographic DTI.
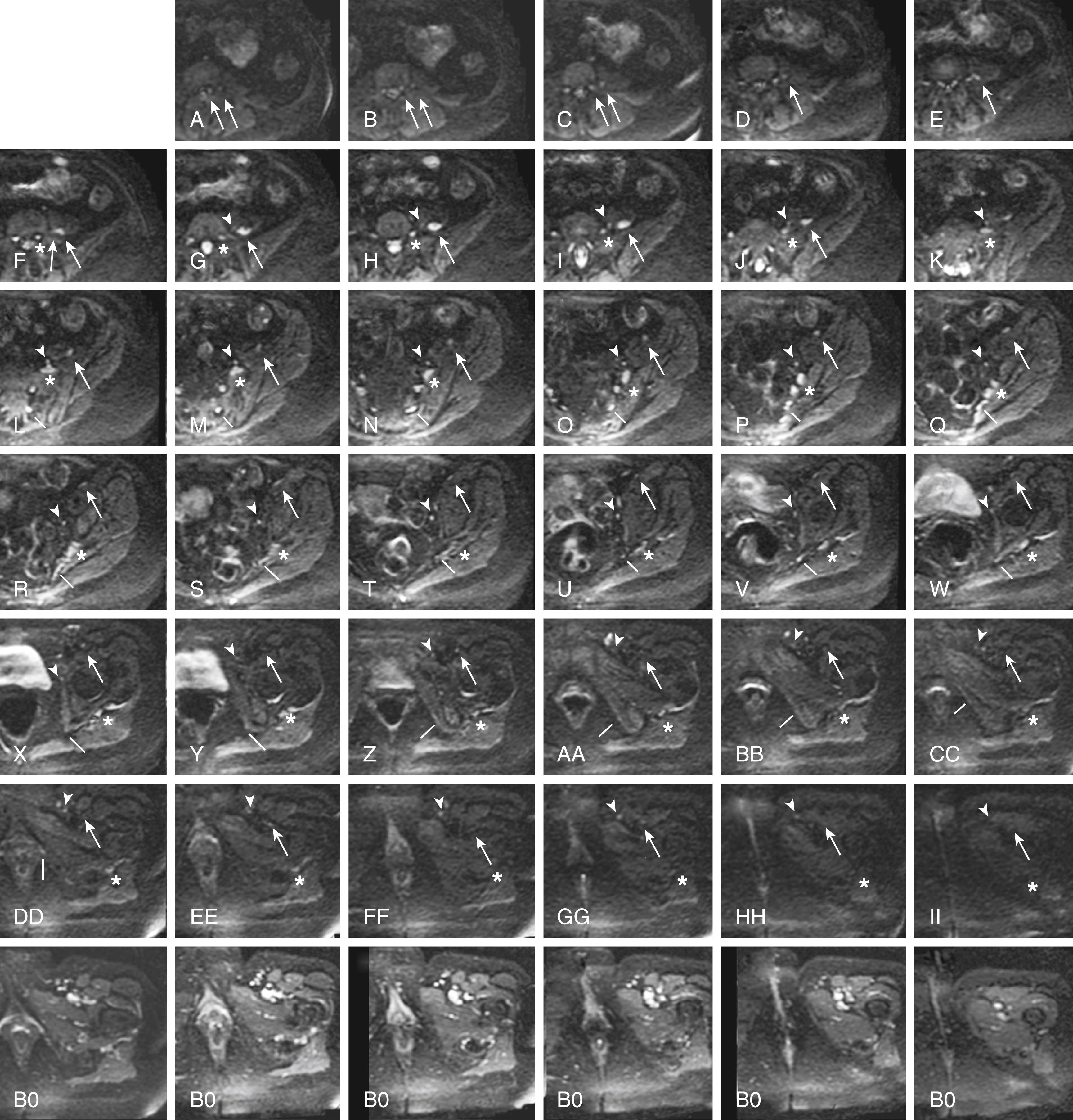
When diffusion images are obtained in multiple different directions for a DTI study, the raw diffusion images can be helpful for identifying the nerve. This step can be done using the original images because they suppress signals from vessels and other structures that are bright on T2-weighted fat-suppressed images, leading to relatively pure nerve images, depending on the orientation of the nerve and the image at a given location. Unlike fully processed DTI images, the raw diffusion component images remain embedded in the original DICOM (Digital Imaging and Communications in Medicine) format spatial grid and can be precisely correlated with T2 neurographic images obtained in the same imaging session ( Fig. 183.1 ).
Fully processed DTI tractography of peripheral nerve is proving to be a very sensitive method for evaluating peripheral nerve pathology. These data can also be overlaid as fractional anisotropy measures onto structural images to provide a novel and important functional perspective. ,
Once the diffusion method was understood, it was possible to show that structures with long decay times (imaged at a relatively long echo time) in fat-suppressed spin-echo images were, in fact, nerves. Previously, nerves had been misinterpreted as exhibiting short decay times on T2 imaging. This was because nerves are a mixture of different tissues, including protein-laden axoplasmic water, myelin, fatty interfascicular epineurium, and connective tissues. Older methods allowed the image signal from these various component tissues to mix. In a variety of different imaging techniques, the result of the image signal mixing was a featureless gray image of the nerve that left nerves difficult to distinguish clearly in an image and caused confusion about the fundamental imaging characteristics of nerve.
In a number of settings, MR neurography has proved to be more efficacious than electrodiagnostic studies for identifying nerve compressions that will improve with surgical treatment. This is true both in diagnoses that are typically evaluated by electrodiagnostics, such as carpal tunnel syndrome, , and in diagnoses in which electrodiagnostics have proved difficult to rely on, such as thoracic outlet syndrome, , piriformis syndrome, , and related sciatic nerve entrapments and injuries, , as well as for pudendal nerve entrapment syndromes , and various complex lumbosacral plexus nerve pathologies.
The utility of MR neurography has now been established in evaluation of entrapment syndromes, , nerve injury and evaluation of repair, and assessment of nerve tumors, as well as in the setting of neuritis and a variety of neuropathies. It has also proved effective for evaluating nerve disorders affecting young pediatric patients, such as obstetric brachial plexus palsy.
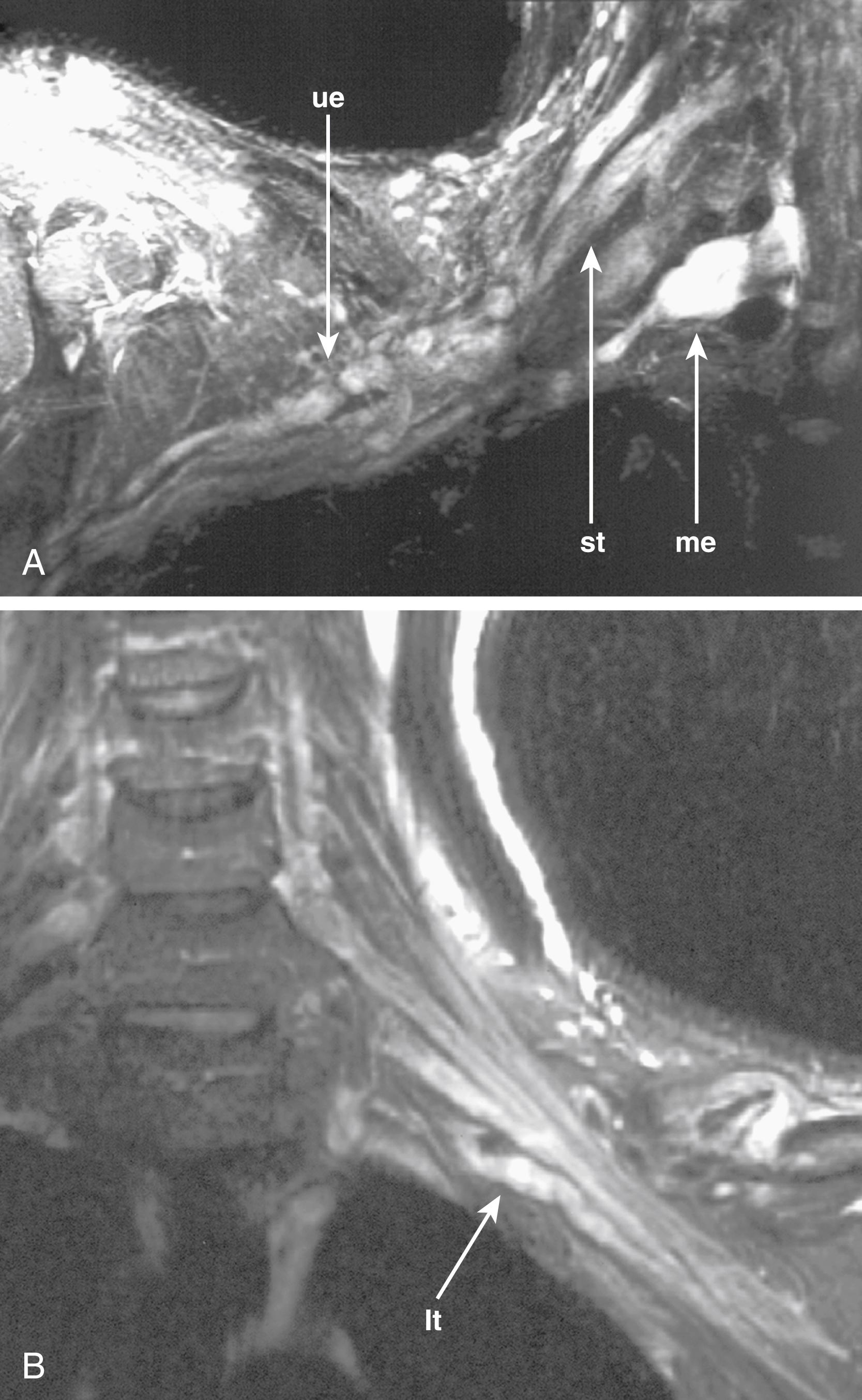
An additional remarkable new area that promises to have a significant impact on neurological pain management in the future is the ability to map autonomic plexus anatomy. A variety of puzzling pelvic pain syndromes, post lumbar fusion dysfunction syndrome, and genital dysfunctions relate to impar ganglion (inferior hypogastric plexus) and superior hypogastric plexus injuries. These are now becoming accessible for image diagnosis and image-guided treatment.
Image findings in MR neurography studies include regions of nerve hyperintensity or nerve swelling, which result from edema at the fascicular level ( Fig. 183.2 ). Distortions of normal nerve course, abnormal contours, and alterations of nerve caliber are also readily seen, any of which can be classed by the degree or severity of the abnormality. These findings can indicate entrapment or adhesions, as well as posttraumatic effects.
In trauma, assessments of nerve continuity and/or location of severed nerve endings are feasible. With the elapse of time after injury or repair, the development of traumatic neuromas may be readily appreciated ( Fig. 183.3 ).
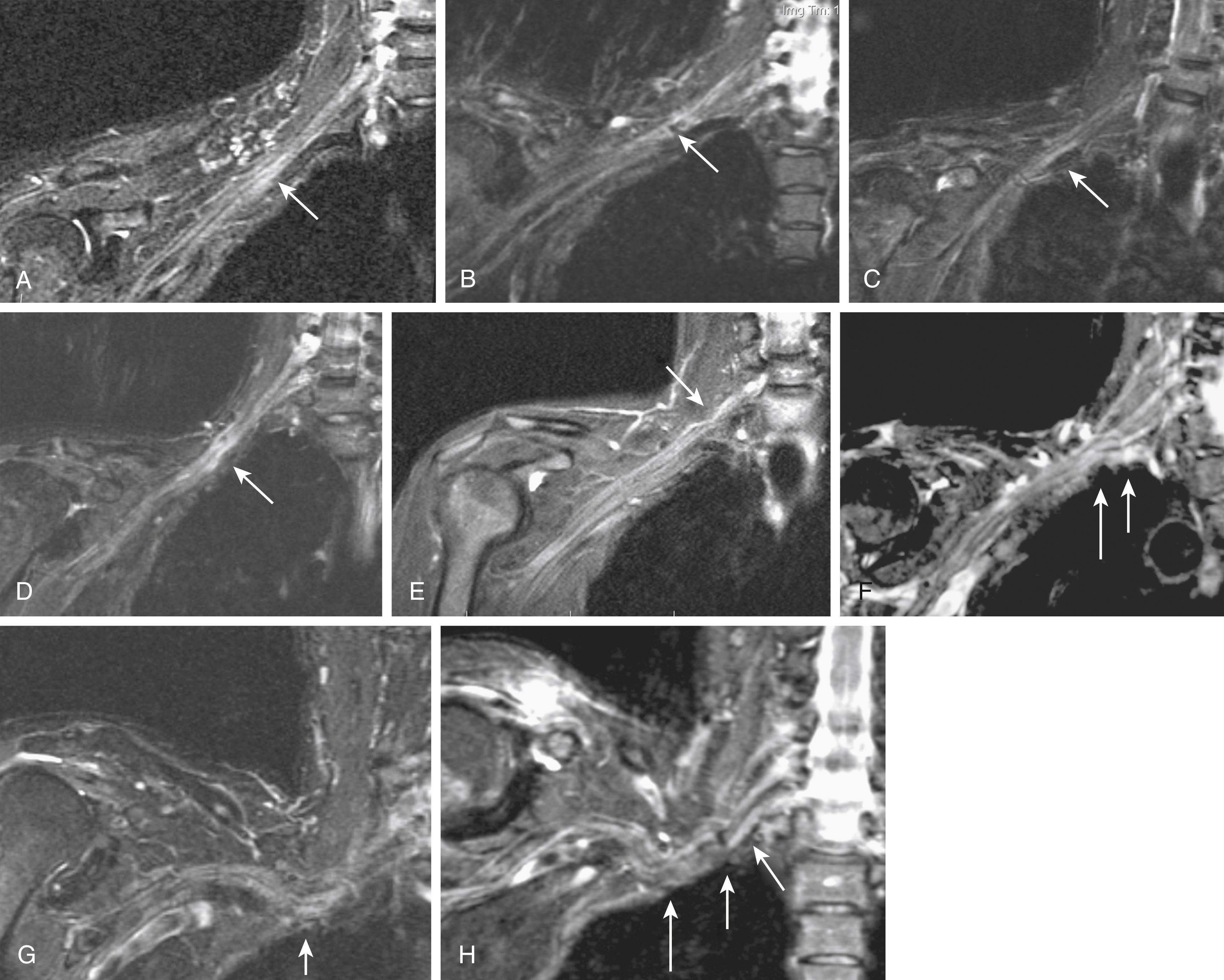
Thoracic outlet syndromes have been problematic diagnostically because of the difficulty of obtaining surgically useful localization of brachial plexus compression sites. Indeed, the limitations in the quality of diagnostic techniques have led to ongoing disagreements about the very existence of this class of nerve entrapment syndromes.
In part, these problems arise because of the difficulty of placing diagnostic electrodes for electrophysiologic studies in this region. Also, because many cases of thoracic outlet syndrome are due to nerve compression by the scalene muscle, it is often the case that patients present with pain elicited by motions such as arm raising but do not have sufficient motor symptoms to produce an abnormal electromyogram (EMG). Finally, the diagnosis of thoracic outlet syndrome is greatly complicated because the term describes a variety of diverse underlying pathologies that have in common only the fact that they affect some part of the brachial plexus.
MR neurography has shown promising capabilities for discriminating among several different types of thoracic outlet syndrome lesions and in many cases can depict well-delineated and readily treatable specific pathologies. , , These include distortions of the course of the proximal elements at the scalene triangle (see Fig. 183.2A–D ), fibrous band entrapments affecting C8 and T1 spinal nerves and the lower trunk of the brachial plexus (see Fig. 183.2F ), gross distortions of the mid-plexus (see Fig. 183.2G and H), irritation at the level of the first rib, and distal plexus irritation.
MR neurography is also helpful when it demonstrates a completely normal course and caliber for all nerve elements that are under suspicion. In the presence of normal findings, it is possible to take a firm stance against surgical treatment of the hand, arm, or shoulder problems that might have been tentatively attributed to a thoracic outlet syndrome.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here