Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
© 2018 Elsevier Inc. All rights reserved. Please note that the copyright for the original figures submitted by the contributors is owned by Contributors.
Chordomas and chondrosarcomas are uncommon primary bone tumors that may arise in the spine. Computed tomography (CT) and magnetic resonance (MR) are the preferred noninvasive tools used to diagnose these lesions and to distinguish them from other spinal masses. Imaging defines the tumor’s relationship to the spinal cord, nerve roots, neural foramina, and adjacent soft-tissue structures, allowing for detailed surgical and radiation treatment planning. After primary treatment, imaging helps to evaluate for treatment-related complications and tumor recurrence.
Plain radiographs may be the first imaging studies obtained to evaluate spinal chordoma and chondrosarcoma, as these lesions often present with nonspecific symptoms such as neck or back pain. Screening radiographs are usually obtained in anteroposterior and lateral views. If a lucent or dense lesion of unknown origin is identified on a radiograph, cross-sectional imaging is essential for further characterization. CT and MR provide complementary information, and both imaging studies are generally obtained to evaluate primary spinal tumors. Table 8.1 summarizes some cross-sectional imaging characteristics for chordoma and chondrosarcoma. A CT without iodinated contrast should be performed with 0.625–1.25 mm continuous axial sections through the level of concern and through adjacent levels. Images should be filtered through both bone and soft-tissue kernels and viewed in both bone and soft-tissue windows. Sagittal and coronal multiplanar reconstructions are essential for evaluating adjacent bone and soft-tissue structures. An MR using a gadolinium-based contrast agent should also be performed. A serum creatinine should be checked prior to gadolinium administration to calculate a glomerular filtration rate (GFR). Gadolinium is not generally administered to patients with a GFR less than 30 (mL/min/1.73 m 2 ), even if they are on dialysis. Key imaging sequences include sagittal and axial T1-weighted precontrast images, sagittal and axial T2-weighted images (usually with fat suppression in one or both planes), and sagittal and axial T1-weighted postcontrast, fat-suppressed images. Fat suppression helps distinguish tumor from fat in the adjacent marrow spaces, as normal bone marrow in adults is bright on both T1-weighted images and fast spin echo T2-weighted images. Diffusion-weighted imaging and perfusion imaging of the spine are not routinely performed to evaluate tumors, as they are technically challenging in the spine, add time to already lengthy examinations, and are not often useful due to artifacts related to susceptibility, motion, respiration, and vascular pulsation.
| Feature | Chordoma | Chondrosarcoma |
|---|---|---|
| Location | Sacrococcygeal > mobile spine Vertebral body |
Thoracic > lumbar > cervical > sacra Vertebral body and/or posterior elements |
| CT | Expansile Lytic and/or sclerotic; can be mixed No internal calcifications |
Expansile Lytic with endosteal scalloping 50% with internal calcification; arcs and whorls |
| T1 | Low to intermediate signal | Low signal |
| T2 | High signal; some components can be intermediate | High signal |
| Postgadolinium Enhancement |
Homogenous or heterogeneous | Homogenous or heterogeneous Internal septations may enhance |
Definitive treatment of spinal tumors often requires surgical resection with subsequent instrumented fusion of adjacent vertebral levels. Posttreatment imaging protocols must be adjusted to minimize metal-related artifacts that can obscure or distort the surgical bed. Indicating the presence of metallic hardware in imaging requests is helpful because metal artifact can be reduced by modifying several geometric parameters such as field of view and slice thickness as well as other more technical acquisition variables that are beyond the scope of this chapter. If hardware is present, CT and MR images should be acquired with standard metal reduction sequences to optimize image quality. In addition, MR examinations should be performed at lower magnetic field strengths, such as 1.5 T instead of 3 T, because a stronger magnetic field generally produces more significant metal artifacts.
In addition to lymphoproliferative tumors, chordomas are the most common primary malignant tumor of the adult spine, accounting for 2%–4% of primary malignant bone tumors. Chordomas occur in late middle age with a peak incidence in the fifth decade. Men are affected about twice as frequently as women. Spinal chordomas grow slowly, so presenting symptoms are often subtle until the tumor reaches a large size. Local pain is the most common symptom, though nerve compression or infiltration can result in numbness, weakness, constipation, and incontinence.
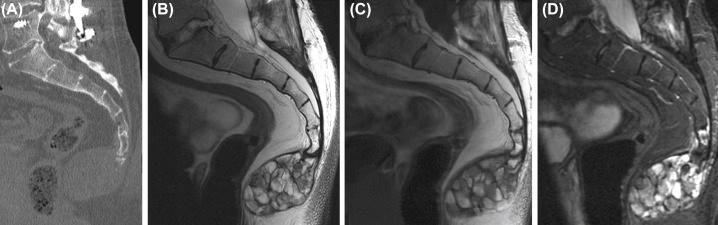
Chordomas arise in the midline because they originate from remnants of the primitive notochord, a structure that develops into the intervertebral regions and nucleus pulposus. They have a predilection for the lower sacrum and sacrococcygeal regions ( Fig. 8.1 ). Overall, 50% of chordomas occur in the sacrococcygeal region, 35% occur in the clivus, and 15% occur in the mobile spine. Within the mobile spine, chordomas occur more commonly in the cervical spine compared to the thoracic and lumbar spines.
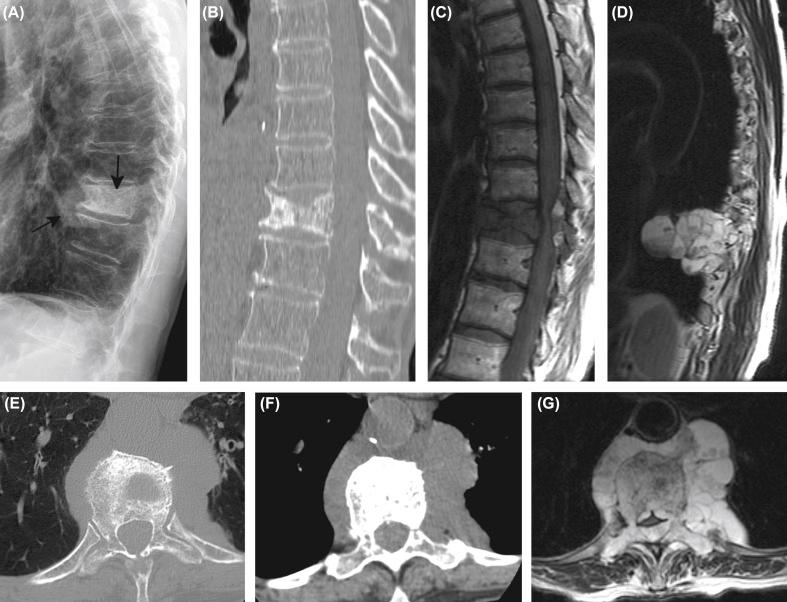
Chordomas often present as large, well-circumscribed, locally aggressive masses with both bone and lobulated soft-tissue components. They may involve multiple spinal levels. CT is useful for showing the bone–tumor interface and the extent of disease. The amount of bone destruction helps determine whether stabilization will be required after surgical resection. On CT, the soft-tissue component may have low internal density reflecting mucoid content and the high water content of physaliphorous cells. A destructive lytic bone component is common, though lesions in the mobile spine may have a sclerotic or a mixed lytic/sclerotic appearance ( Fig. 8.2 ). The presence of bony sclerosis in spinal chordomas is different from clival chordomas, which usually show purely lytic bone changes. If calcifications are present, they are often distributed in an amorphous or punctate pattern ( Fig. 8.3 ), and some may represent lysed bone fragments.
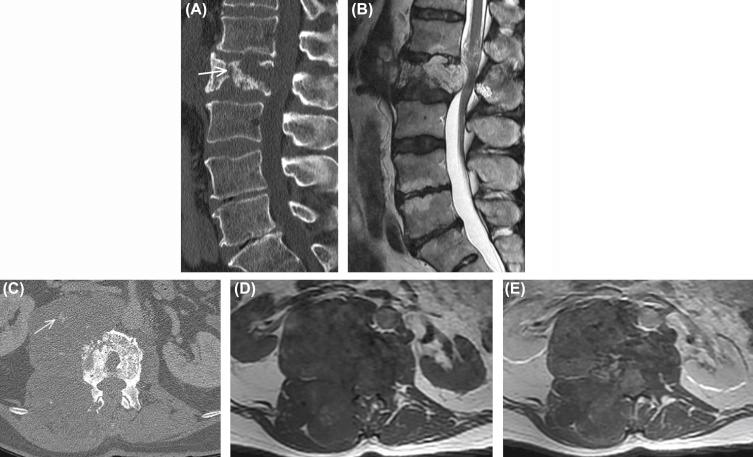
MR has greater soft-tissue contrast resolution compared to CT, and so MR more completely evaluates the internal tumor architecture and the tumor’s relationship to critical structures such as spinal cord, nerve roots, and pelvic organs. On MR, chordomas characteristically have low to intermediate signal on T1-weighted images, high signal on T2-weighted images, and mild-to-moderate enhancement on gadolinium-enhanced images ( Fig. 8.3 ). However, variable or heterogeneous internal T1 and T2 signal is common. Chordomas may have internal septations, with low-signal bands on T2-weighted images separating gelatinous cystic-appearing areas ( Fig. 8.1 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here