Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Hybrid coronary revascularization (HCR) is defined as the combination of coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) to treat multivessel coronary artery disease (CAD). HCR most commonly combines a minimally invasive CABG procedure involving a left internal thoracic artery (LITA) to the left anterior descending coronary artery (LAD) anastomosis with PCI to non-LAD vessels. This technique offers and combines the advantages of surgical and percutaneous revascularization, eliminating at the same time the disadvantages of both procedures. In fact, this evolving revascularization technique uses the survival benefits conferred by the LITA to LAD graft while providing the patient with complete and minimally invasive coronary artery revascularization with PCI to the non-LAD vessels. The sequence and timing of the surgical and interventional components of hybrid therapy can be in three different ways: PCI first followed by surgery, surgery followed by PCI (two-stage HCR), or both carried out during the same setting (single-stage HCR). In the era of primary PCI for ST-segment elevation myocardial infarction (MI), it is probable that patients requiring immediate PCI of the right coronary artery (RCA) or circumflex artery as the culprit lesion may require subsequent surgical revascularization of a complex LAD or left main lesion at some time in the future. Hence, HCR, by definition, generally refers to a revascularization strategy that has been strategically planned in a coordinated fashion by interventional cardiologists and cardiac surgeons.
The optimal revascularization strategy for multivessel CAD is still debated. Although there are survival benefits of complete arterial coronary revascularization, in practice only a fraction of patients referred for CABG actually receive this; most of them receive at least one saphenous vein graft (SVG). If it is true that recent trials, including SYNTAX, have helped establish which anatomic categories are best addressed with traditional CABG versus multivessel PCI with a drug-eluting stent (DES), it is also true that there is still potential for prognostic and symptomatic improvement from coronary revascularization in certain patients with multivessel CAD. The modality depends on many factors, the most important of which is the coronary anatomy itself. Other crucial factors include the clinical setting (e.g., emergent, acute, chronic); left ventricular function; degree of myocardial viability; and presence or absence of comorbidities, assessed through the risk score of the Society of Thoracic Surgeons (STS) or EuroScore (e.g., diabetes, associated valvular heart disease, presence of calcification of the ascending aorta, which could preclude safe cross-clamping during surgical intervention, age, patient preference, availability of bypass conduits). Outcomes in diabetic patients, in particular, seem to favor a surgical strategy over PCI for multivessel disease, although first-generation sirolimus-eluting and paclitaxel-eluting stents were the predominant types of DESs used in the FREEDOM trial and may underestimate the benefits of current (third-generation) stenting.
However, CABG is still considered the gold standard treatment for patients with multivessel CAD. The major therapeutic benefits of CABG arise from the graft of the LITA to LAD, which has been shown to have excellent long-term results in terms of patency, event-free survival, and relief of angina. On the other hand, SVGs have shown a high incidence of failure as opposed to multivessel PCI with a DES, which has shown lower restenosis rates, lower failure rates than SVG, and lower stroke rates compared with CABG. In addition, PCI is less invasive and has a shorter recovery time. HCR thus represents a promising coronary revascularization option due to the fact that it offers the advantages of the best of both treatment options. It takes advantage of the survival benefit conferred by the LITA to LAD graft while minimizing the invasiveness of revascularization therapy and providing a complete revascularization with PCI to the non-LAD vessels. Additionally, the use of the robotic-assisted, coronary artery bypass grafting (RA-CABG) graft of the LITA to the LAD minimizes surgical trauma further.
Several studies have already demonstrated similar results in terms of mortality, patency, and major adverse cardiac event rates—between a hybrid revascularization strategy and similar conventional on- and off-pump coronary bypass surgery. However, the safety and effectiveness of HCR is still understudied and further studies, especially randomized trials, are necessary before stronger recommendations can be made for this revascularization therapy.
HCR was first described by Angelini et al. in 1996. They used the classic minimally invasive direct coronary artery bypass (MIDCAB) procedure, in which the LITA is harvested by direct vision through a fourth interspace left minithoracotomy; the LITA is sutured to the LAD on the beating heart. After the pioneering work of Benetti et al. on minimally invasive CABG, MIDCAB was adopted by several groups in the mid-1990s. HCR then evolved as a result of the desire to treat patients with multivessel disease effectively while at the same time lowering procedure-related morbidity by combining minimal access coronary artery surgery with percutaneous techniques.
This was a very innovative and visionary new concept in the field of coronary revascularization, representing a mix and the natural evolution of the two disciplines, cardiac surgery and interventional cardiology. Interventional cardiologists were progressively more aggressive in their percutaneous treatment of CAD; surgeons were developing minimally invasive techniques with a smaller incision, avoidance of sternotomy, and beating heart surgery technique. Additionally, throughout the 1990s, endoscopic, video-assisted, and finally robot-assisted LITA dissection were performed. Successful endoscopic harvesting of LITA has been a crucial step in the performance of minimal access coronary artery bypass surgery through minithoracotomy incisions, and video-assisted LITA takedown has been further facilitated by the use of robotic assistance. In the last 15 years, telemanipulation surgical systems have significantly improved, and currently RA-CABG encompasses the use of robotic assistance to varying degrees, from robotic-assisted LITA harvest to manual anastomosis through a mini anterior non-rib spreading incision procedures to total endoscopic coronary artery bypass (TECAB). On the other hand, there has been a continuous improvement of DES performance and, in low-risk patients and those with single-vessel disease, PCI can now provide comparable short- and mid-term outcomes to those of CABG.
According to the 2011 American College of Cardiology/American Heart Association guidelines for CABG, HCR is a suitable coronary revascularization strategy for patients with multivessel CAD (e.g., LAD and one or more non-LAD stenoses) and an indication for revascularization:
Hybrid revascularization is ideal in patients in whom technical or anatomic limitations to CABG or PCI alone may be present and for whom minimizing the invasiveness (and therefore the risk of morbidity and mortality) of surgical intervention is preferred (e.g., patients with severe preexisting comorbidities, recent MI, a lack of suitable graft conduits, a heavily calcified ascending aorta, or a non-LAD coronary artery unsuitable for bypass but amenable to PCI, and situations in which PCI of the LAD artery is not feasible because of excessive tortuosity or chronic total occlusion).
HCR, defined as the planned combination of LITA to LAD artery grafting and PCI of one or more non-LAD coronary arteries, is reasonable in patients with one or more of the following (level of evidence: B):
Limitations to traditional CABG, such as heavily calcified proximal aorta or poor target vessels for CABG (but amenable to PCI).
Lack of suitable graft conduits.
Unfavorable LAD artery for PCI (i.e., excessive vessel tortuosity or chronic total occlusion).
HCR, defined as the planned combination of LITA to LAD artery grafting and PCI of one or more non-LAD coronary arteries, may be reasonable as an alternative to multivessel PCI or CABG in an attempt to improve the overall risk-benefit ratio of the procedures (level of evidence: C). According to the 2014 European Society of Cardiology/European Association for Cardio-Thoracic Surgery guidelines on myocardial revascularization :
Hybrid procedures consisting of LITA to LAD and PCI of other territories appear reasonable when PCI of the LAD is not an option or is unlikely to portend good long-term results or when achieving a complete revascularization during CABG might be associated with an increased surgical risk.
HCR may be clinically indicated in the following cases :
Select patients with single-vessel disease of the LAD, or in those with multivessel disease but with poor surgical targets, except for the LAD territory, in whom minimally invasive surgery can be performed to graft the LAD using the LITA. The remaining lesions in other vessels are subsequently treated by PCI.
Patients who had previous CABG and now require valve surgery and who have at least one important patent graft (e.g., LITA to LAD) and one or two occluded grafts with a native vessel suitable for PCI.
Combination of revascularization with nonsternotomy valve intervention (e.g., PCI and minimally invasive mitral valve repair, or PCI and transapical aortic valve implantation).
In addition, some patients with complex multivessel disease presenting with STEMI initially require primary PCI of the culprit vessel, but subsequently may require complete surgical revascularization. A similar situation occurs when patients with combined valvular and CAD require urgent revascularization with PCI. Finally, when a heavily calcified aorta is found in the operating room, the surgeon may elect not to attempt complete revascularization and to offer delayed PCI.
In the Canadian Cardiovascular Society/Canadian Association of Interventional Cardiology/Canadian Society of Cardiac Surgery Position Statement on Revascularization—Multivessel Coronary Artery Disease, it is stated that HCR:
Is typically performed with minimally invasive incisions.
Combines the advantage of the LITA to LAD graft with the less invasive nature of PCI.
Has been demonstrated by studies to date to be safe and effective, but definitive data (e.g., randomized trials) are lacking.
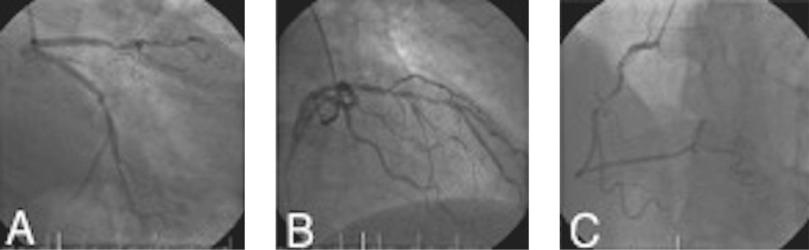
However, the lack of randomized controlled clinical trials does not allow the identification of an HCR target group of patients. Therefore, HCR should be considered an alternative treatment strategy that should be tailored to the individual patient based on the patient's anatomy and patient-related variables through a collaborative heart team approach. The ideal patient is a patient with multivessel CAD, with a complex proximal LAD lesion suitable for LITA-LAD grafting, associated with non-LAD lesions suitable for PCI, and no contraindications for dual antiplatelet therapy ( Fig. 6.1 ). Careful attention should be focused on the quality and size of the LAD, epicardial or intramyocardial LAD course ( Fig. 6.2 ), presence of large diagonal vessels, which can be mistaken as the LAD and inadvertently grafted, complexity of non-LAD vessel lesions for PCI, and number of stents necessary to treat the non-LAD stenosis effectively. PCI of overly complex non-LAD vessels (e.g., long lesions, bifurcations of major branches) will increase the risk of restenosis and may diminish the benefits of a percutaneous strategy over saphenous vein or other arterial grafting.

Other important factors in patient selection for HCR are patient variables, including clinical presentation, comorbidities, body habitus, chest wall anatomy, and surgeon experience with minimally invasive CABG procedures. Chest wall anatomy, obesity, and thoracic size may have a significant impact on the surgical part of the procedure. Patient comorbidities, such as chronic obstructive pulmonary disease and pulmonary hypertension, also have a significant impact. For a robotic-assisted approach, the patient must be able to tolerate single-lung ventilation and physiologic changes related to carbon dioxide insufflation. HCR could then serve patients at the two extremities of the risk spectrum—young and relatively healthy patients who prefer to avoid the sternotomy but do not want to renounce the durability of the LITA-LAD graft, and older and/or high-risk patients who may benefit from a less traumatic, minimally invasive but full and complete coronary revascularization. In the end, it is quite intuitive that the experience of the surgeon is a key factor in the successful outcome of this revascularization strategy, given the challenging nature and steep learning curve of the minimally invasive CABG techniques (from RA-CABG to TECAB).
A minimally invasive coronary artery bypass procedure is done first ( Fig. 6.3 ). The patient remains on aspirin preoperatively, intraoperatively, and postoperatively. After harvest of the LITA, bivalirudin at a loading dose of 0.75 mg/kg is administered; infusion at a rate of 1.75 mg/kg/hr is continued throughout the rest of the procedure, including the surgical revascularization and PCI. After the surgical revascularization is completed, the hybrid operating room is then reset to a cardiac catheterization configuration. The LITA graft check is performed. After hemostasis is confirmed, with evidence of minimal drainage from chest tubes, clopidogrel, 600 mg, or ticagrelor, 180 mg via a nasogastric (NG) tube, is administered ( Fig. 6.4 ). PCI is performed on non-LAD targets. The bivalirudin infusion is continued and overlapped with the clopidogrel over the next hour. Postoperatively, the patient is continued on aspirin and clopidogrel or ticagrelor.
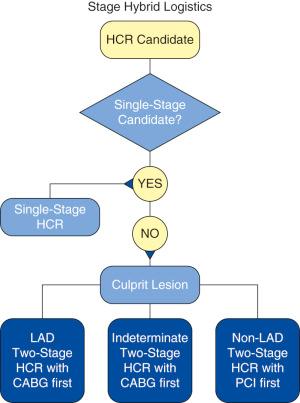
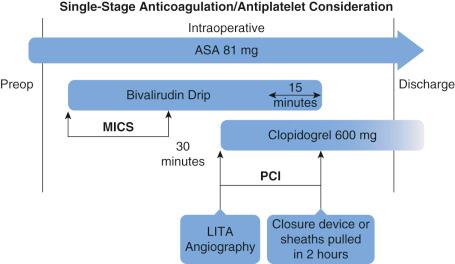
If PCI has already been performed on the culprit non-LAD vessel, then after 3 months the clopidrogrel or ticagrelor are held for 2 days prior to the surgery but not the ASA. The dual antiplatelet therapy is restarted the day after surgery. Minimally invasive surgical revascularization is performed as per routine using heparin and protamine for reversal. If PCI is to be performed postoperatively, the evening after surgery the patient is given a loading dose of clopidogrel or ticagrelor; the patient undergoes PCI on the next day. Postoperatively, the patient is continued on aspirin and clopidogrel or ticagrelor.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here