Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter includes an accompanying lecture presentation that has been prepared by the authors: ![]() .
.
Functional neurosurgery in the first half of the 20th century centered around the treatment of psychiatric disorders as noninvasive therapeutics were ineffective at the time.
Surgical ablation was the most efficacious therapeutic method for movement disorders in the era before the discovery of levodopa.
Surgical applications for both psychiatric and movement disorders declined in the mid-20th century with the emergence of new pharmacologic therapies that are efficacious and safe.
In the last quarter of the 20th century, side effects and loss of efficacy in medical treatment began to become apparent, renewing interest in modern methods of surgical treatment, such as high-frequency stimulation of subcortical targets.
Stereotactic tools and methods are inseparable from the success of functional neurosurgery and have been developed in parallel to these developments as functional surgery evolved.
As functional neurosurgery has gone through decades of advancement and refinement, ethical guidelines have been established to protect the most vulnerable populations. However, ethical concerns in functional neurosurgery remain abundant, many remain unresolved, and new issues will continue to surface as neurotechnology reaches new frontiers.
In the late 19th century, the correlation of neurological functions to neuroanatomy began to emerge. Through this new knowledge, the first procedures for treating psychiatric disorders were performed by the Swiss psychiatrist Gottlieb Burckhardt (1836 to 1907). These were performed as cerebral topectomies in six patients with intractable mental illness characterized by pronounced aggression and auditory hallucinations. Most of these patients were diagnosed with primare Verruecktheit, translated as “primary madness,” analogous to the modern diagnosis of schizophrenia. Although three of the six patients showed partial improvement, Burckhardt’s subsequent presentation of these results at the 1889 International Medical Congress in Berlin generated firm condemnations from the medical community, leading to a consensus that these interventions should not be performed in the future. ,
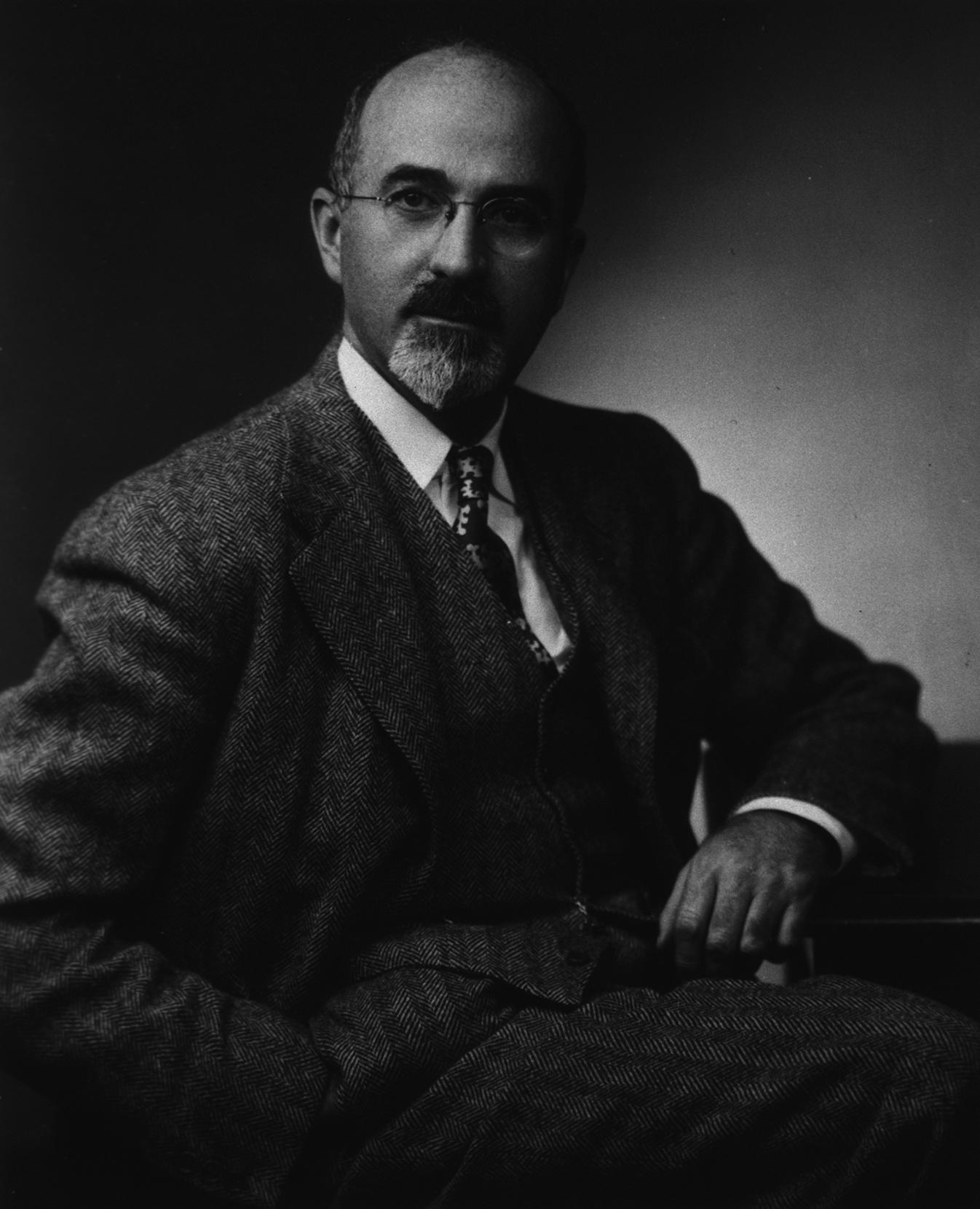
At the International Neurological Congress in London in 1935, Yale physiologists John Fulton and Carlyle Jacobsen presented postoperative behavioral alterations in two chimpanzees (Lucy and Becky) after surgical frontal lobe ablations, and the neurologist Richard Brickner presented a case of frontal lobe ablation for olfactory meningioma. , In attendance were Egas Moniz, a Portuguese neurologist, and Walter Freeman ( Fig. 120.1 ), an American neurologist. Inspired by these nonhuman primate cases together with the desire to alter the course of the “mentally insane,” one of the most burdensome public health crises of his time, Moniz and his neurosurgical colleague Almeida Lima performed the first prefrontal leucotomy at the Santa Marta Hospital in Lisbon in 1935. With nonexistent ethical oversight of novel therapies at the time, surgical treatment of mental illness relied on neurosurgical tools and the experimental creativity of the surgeons.
In the ensuing 6 months, Moniz and Lima performed leucotomies in 20 patients by creating frontal lobe white matter lesions. At first, alcohol was used as the primary ablative agent, but soon afterward, Moniz and Lima led the development of the leucotome, and use of this instrument became their method of choice for leucotomy. The majority of patients (14 of 20) were documented to be symptomatically improved or recovered. , Moreover, Moniz and Lima demonstrated low rates of morbidity and zero mortality, which enabled further exploration of these techniques. In 1949, Moniz was awarded the Nobel Prize for this work.
At the time Moniz reported his initial experience, Walter Freeman (neuropsychiatrist) and James Watts (neurosurgeon) began investigating leucotomies for the treatment of behavioral disorders, reporting their experience on 200 patients in 1942. Some of the first prefrontal lobotomies (as they named their procedure) were performed by creating bilateral frontotemporal bur holes. A calibrated blunt instrument was passed toward the midline, followed by a sweeping motion to disrupt the frontal lobe white matter. Although most patients experienced satisfactory clinical improvement, some reported complications included seizures, behavioral abnormalities, and what was termed frontal lobe syndrome. Other groups took up what Freeman labeled psychosurgery . Long-term follow-up reported by the Connecticut Lobotomy Commission confirmed improvement of agitation and disruptive behavior in postoperative patients. However, the same report also noted that a number of patients experienced “post-leukotomy syndrome.” , Nonetheless, in the absence of efficacious nonsurgical alternatives for these severely disabling illnesses, Freeman would continue to promote surgical treatment of psychiatric patients, even after Watts departed from this collaboration.
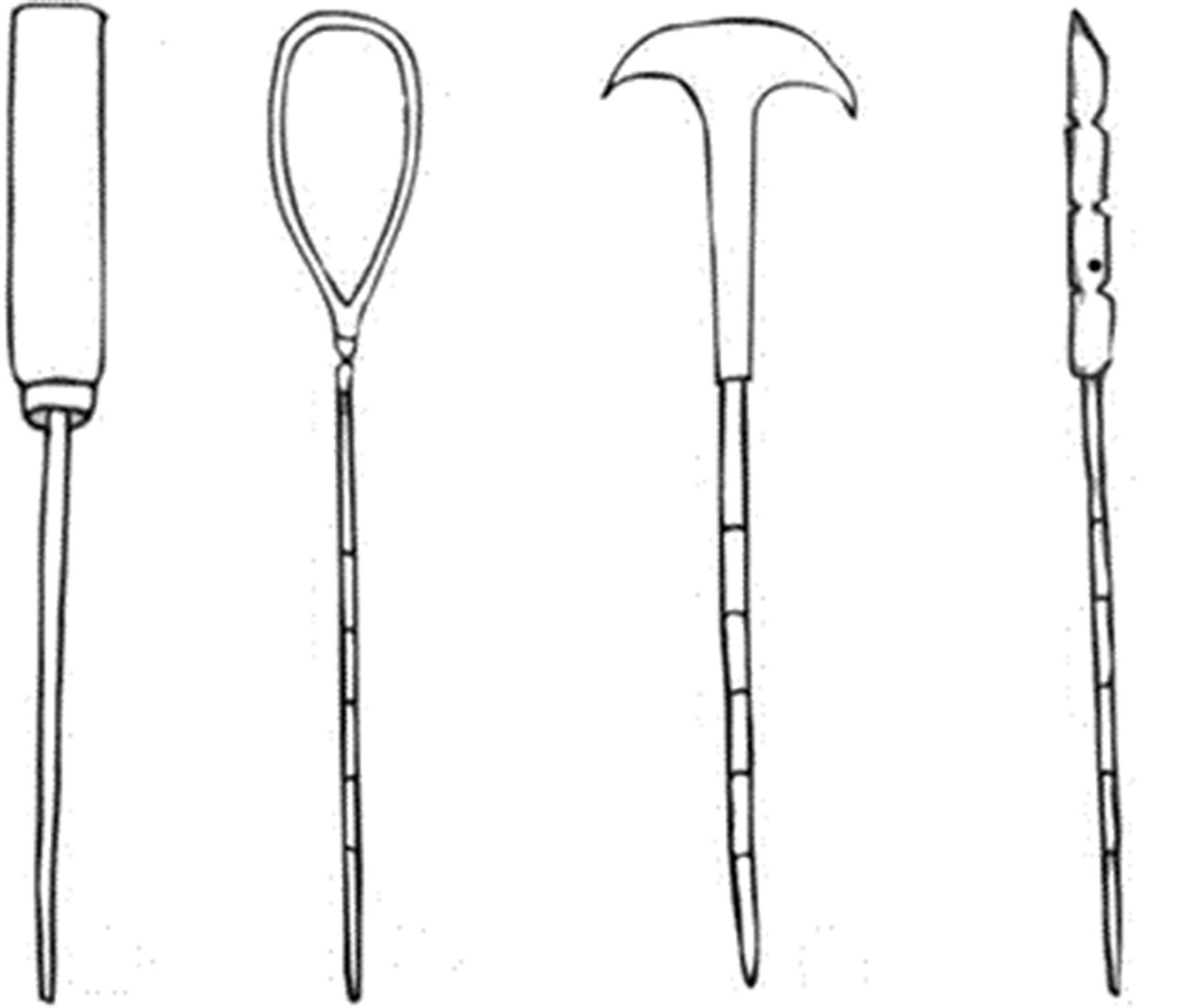
The transorbital leucotomy (also known as the “icepick” procedure) was developed by Freeman in 1948 to decrease the size of the psychosurgical lesions and thereby the related side effects. Freeman’s technique involved performing electroconvulsive therapy to induce a seizure and thereby unconsciousness. He then used a sharp instrument (an orbitoclast ) to break through the orbital roof ( Fig. 120.2 ), mechanically disrupting the posterior medial orbitofrontal cortex. Freeman traveled across the United States to advocate for this transorbital procedure, but Watts refused to participate, effectively ending their collaboration.
By 1949, an estimated 10,000 leucotomies had been performed across the United States and Britain. Based on initial reports, the procedure was at one point recommended by the US Department of Veterans Affairs for the treatment of World War II veterans suffering from intractable psychiatric symptoms. Given the limited treatment alternatives and overcrowding of psychiatric institutions, leucotomies were an opportunity to treat patients with mental illnesses who were imposing significant societal and economic burdens.
In 1954, the first clinically effective psychotropic drug, chlorpromazine, was approved by the US Food and Drug Administration, leading to a reduction in the number of leucotomies performed. Within the first year of release, chlorpromazine was taken by approximately 2 million patients. Acceptance and widespread use of this novel pharmacotherapeutic option was in part fueled by the public’s increasing skepticism about the outcomes of leucotomy and concerns about surgical complications. In the decades that followed, the development of other new medications combined with media stigmatization led to a dramatic reduction in surgical interventions for psychiatric illnesses. Although Freeman was regarded by some as a fierce advocate for those who were helplessly overcome by their illness, he was also detested by others who accused him of disregarding ethical bounds. Debates about his legacy endure.
Today, surgery for psychiatric disease is nearly exclusively practiced in specialized centers around the world as a treatment of last resort for carefully selected patients who are unresponsive to noninvasive treatment. Surgical interventions (including incisionless lesioning such as radiosurgery) are only considered for patients with severe, chronic, disabling, and treatment-refractory psychiatric illness. In the past several years, large numbers of professional organizations and associations across the globe have developed rigorous criteria and international guidelines. The major psychiatric diagnostic clusters , as defined by the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-V), that may benefit from surgical intervention include obsessive compulsive disorder (OCD) and major affective disorder (i.e., unipolar major depression or bipolar disorder). However, patients presenting with mixed or overlapping symptoms constituting a combination of anxiety, depression, and OCD may also remain candidates for surgery. On the other hand, no current indications exist for the surgical treatment of schizophrenia, although several authors have proposed revisiting this indication. One definite legacy of the era of psychosurgery, and of Walter Freeman, is an ongoing approach of extreme caution to the very idea of any surgery, no matter how precise or minimally invasive, for patients with psychiatric illness.
In the early years of treatment for patients with movement disorders, pharmacotherapy was nonexistent while surgeons tested ablative or resective procedures on various intracerebral targets. The rationale for lesioning the motor systems of patients with movement disorders is that a weakening of motor function would yield a reduction of motor disturbances and disorders. Early approaches for creating lesions include pyramidotomies or corticectomies, and the identification of efficacious targets were nonetheless incidental and serendipitous. Using existing knowledge of motor lesioning, Russell Meyers in the early 1940s conceived of lesioning the extrapyramidal system in the basal ganglia, specifically the caudate nucleus or the pallidofugal fibers of the ansa lenticularis. Although the caudate nucleus was regarded as a structure necessary for consciousness (as postulated by Walter Dandy), it was a clinical encounter that provided Meyers with the evidence that the caudate could be safely lesioned. Shortly thereafter, Meyers performed his first caudate resection in a young patient with disabling postencephalitic hemiparkinsonism, which led to a prolonged and significant reduction in tremor. Separately, during an intended surgical pyramidotomy, Irving Cooper injured the anterior choroidal artery. However, this did not lead to new deficits but surprisingly suppressed the patient’s tremor. Although the hypothetical mechanism derived from this finding was the potential efficacy of lesioning the pallidum (supplied by the disrupted artery), follow-up studies demonstrated that the most effective lesions were those originating in the thalamus.
In the treatment of Parkinson disease (PD), stereotactic pallidotomy (globus pallidus internus [GPi] lesioning) or thalamotomy (ventralis intermedius [VIM] nucleus of the thalamus [thalamotomy]) were the primary modalities. These procedures were applied for symptomatic treatment in refractory cases because little was available in the way of medical management for motor complications in patients with advanced PD. Stereotactic ablation concentrated on the pallidothalamic pathway, which includes the globus pallidus and the thalamus. Lesions in the GPi improved dyskinesias and parkinsonian motor symptoms, while thalamotomy was most effective at relieving tremor. Although surgical lesioning often resulted in overall motor symptom relief, the lack of medical alternatives exposed patients to the risk for permanent and severe neurological surgical complications such as dysarthria or hemiparesis. Furthermore, bilateral surgical procedures were rarely performed because of the significantly elevated risk for complications.
Before the 1960s, the only efficacious treatment of movement disorders was surgical lesioning. Through the 1957 work of the Nobel laureate Arvid Carlsson, the dopamine precursor levodopa was found to reverse reserpine-induced akinesia. This led to the subsequent widespread clinical use of levodopa in the treatment of PD to address three core symptoms of the disorder: tremor, akinesia, and rigidity. As levodopa gained momentum in the 1970s, the number of surgical ablations decreased. Although levodopa benefits from immediate effects, reversibility, and titratability, its efficacy often decreases after 5 to 7 years of treatment. Patients often experience motor fluctuations, such as periods of severe dyskinesia (immediately after taking levodopa) interrupted by akinesia (after the effects have worn off). In response, one ablative solution was pallidotomy, which relieved dyskinesia and allowed patients to tolerate higher doses of levodopa to combat akinesia.
In an effort to reduce the effects of long-term levodopa use, Alim Benabid and colleagues reported the use of electrical stimulation in the VIM at various frequencies. In 1987, while performing a thalamotomy for the treatment of essential tremor, Benabid et al. realized that, while using electrical stimulation to identify the functional target and based on previous trials, stimulation at frequencies of greater than 100 Hz led to acute and reversible improvements in tremor. Additionally, this range can be increased up to the kilohertz range and is adaptable with low morbidity, even with bilateral stimulation. These results led to the modern framework of subcortical deep brain stimulation (DBS), including targeting the GPi and the subthalamic nucleus for the treatment of PD.
Historical narratives of functional neurosurgery are inseparable from the inception of human stereotaxis, which was initially designed, implemented, and later improved by Ernst A. Spiegel (neurologist) and his student and colleague Henry T. Wycis (neurosurgeon) at Temple Medical School.
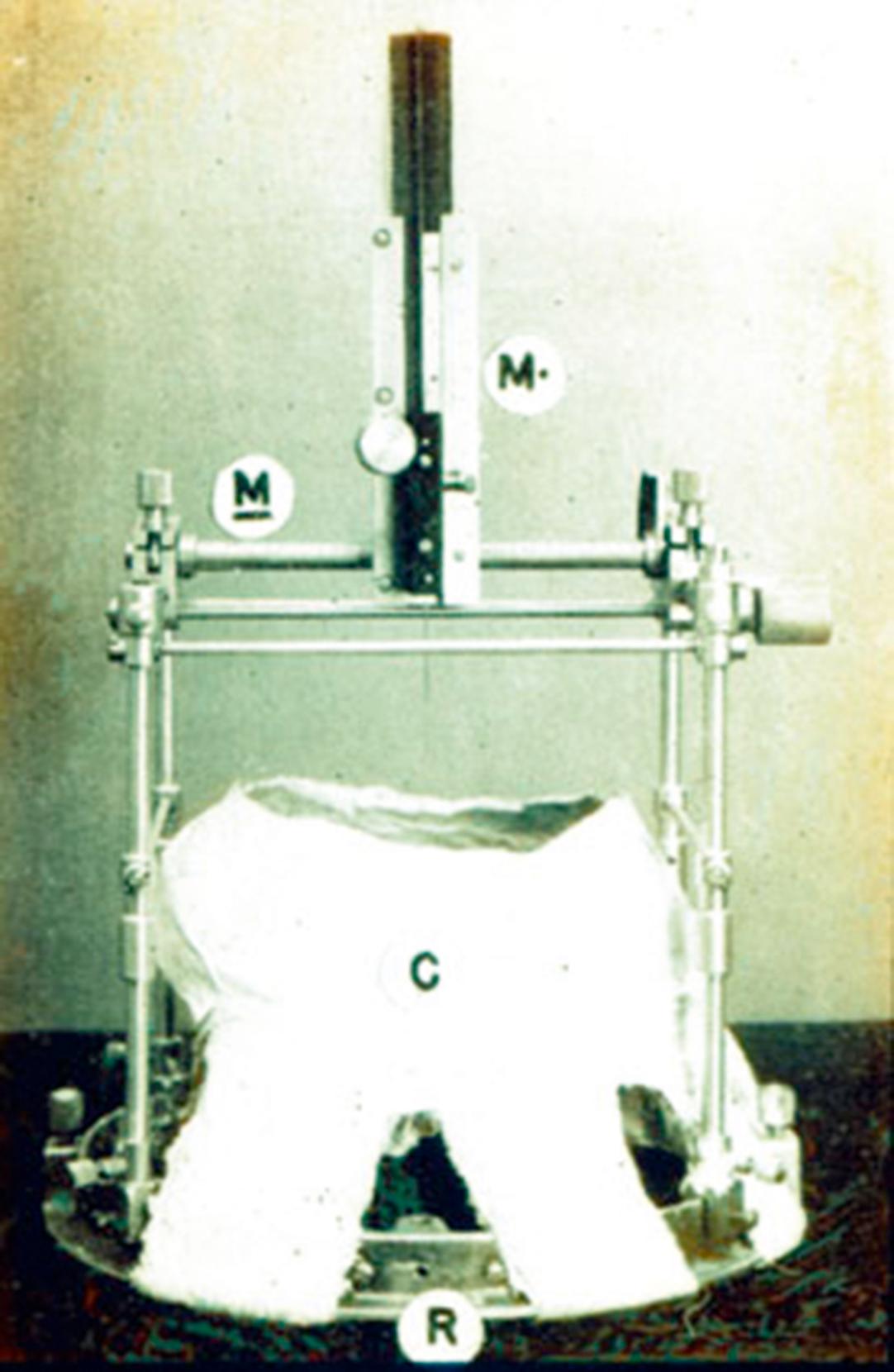
The first approach to human stereotaxis consisted of a ring-mounted Horsley-Clarke apparatus, which was suspended from a plaster cap that was individualized for each patient. The electrode was configured with two degrees of freedom and was advanced using a microdrive. After several revisions, Spiegel and Wycis settled on their model, which was introduced in 1956 ( Fig. 120.3 ), for the remainder of their careers. This apparatus was made to have legs and posts, allowing it to be detachable from four semipermanent screws placed into the cranium. The importance is highlighted by the necessity of pneumoencephalography for radiographic localization, which was performed on the day of admission when the skull screws and posts would be inserted. After proper alignment of the stereotactic instruments, a pneumoencephalogram was then performed and used for identification of the intraventricular landmarks relative to the intraparenchymal target. At this point of the procedure, the patient would nearly always develop nausea, vomiting, and severe headache, precluding a safe awake procedure. With the skull screws in place, the remainder of the apparatus would be removed, allowing the patient to recover for about 2 days, after which the apparatus would be reattached and the intended procedure resumed. Spiegel and Wycis consistently performed electrophysiologic stimulation and recording in all patients. Additionally, they attempted to correlate their human data with results from animal experiments in an effort to elucidate underlying neural mechanisms and expand the indications and targets for stereotactic neurosurgery.
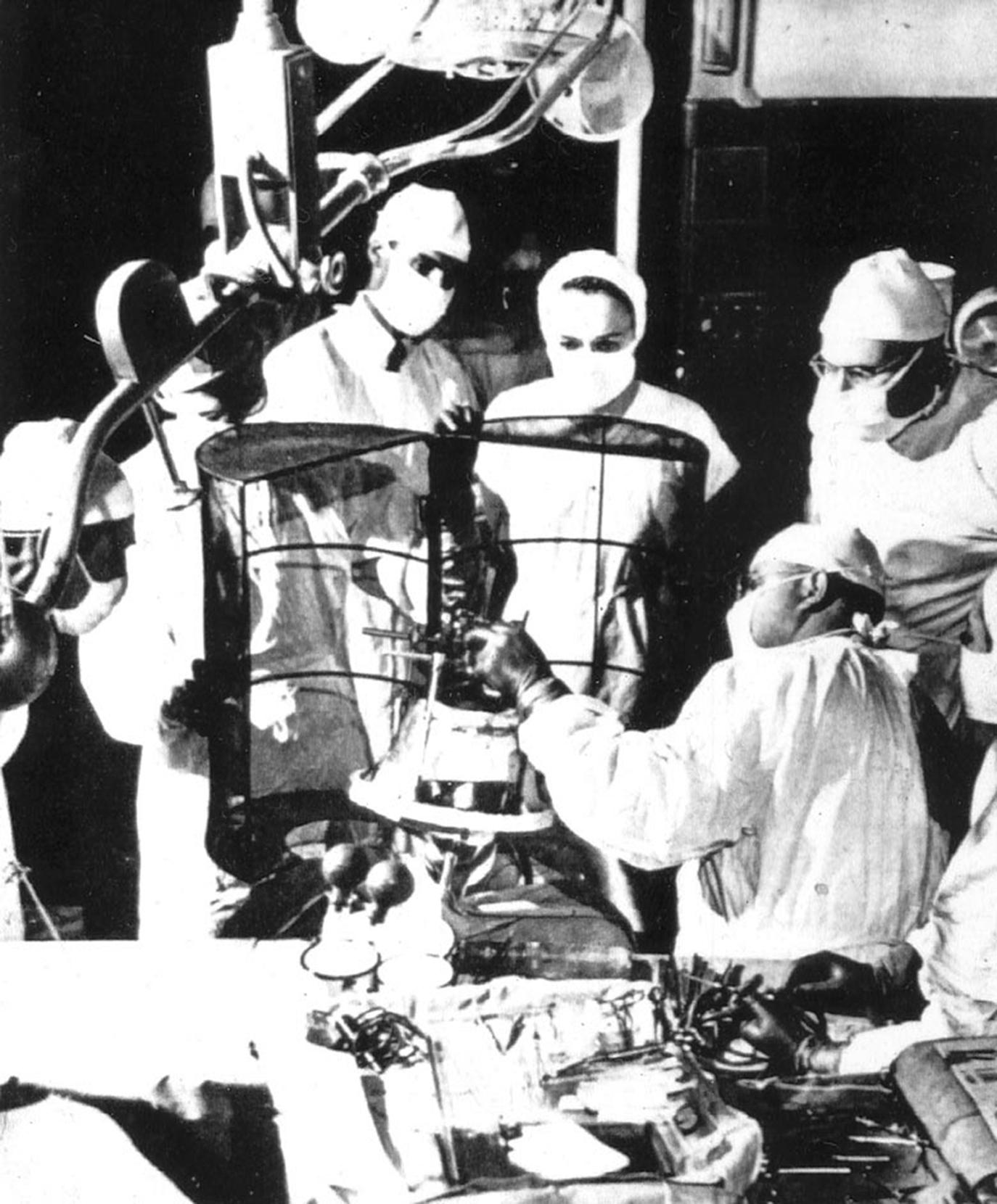
The electronic components used by Spiegel and Wycis to record from the human brain were primitive, large, and bulky. A cylindrical grounded copper cage that opened on a hinge, just large enough to incorporate the patient’s head and the stereotactic instruments ( Fig. 120.4 ), was created for shielding in the operating room. Advances in electrophysiology insulation made it possible to record in the operating room without such shielding by the end of the 1960s. Treatment was performed through delivery of alcohol to discrete deep nuclei, such as the globus pallidus (to perturb the extrapyramidal pathways), to produce lesions that would spare tracts in surrounding pathways. Additional targets included the dorsomedial nucleus of the thalamus (connected to the prefrontal areas) with the intention of achieving a sedative effect, as abnormal movements intensified with agitation. These initial procedures illustrated the principles of human stereotactic surgery and, more importantly, demonstrated the possibility that extrapyramidal lesioning could improve motor function without causing motor control deficits or weakness. This laid the groundwork for practical surgical management of patients with movement disorders and those with pain, epilepsy, and psychiatric illness.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here