Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Headaches are classified as primary or secondary. Primary headaches are benign, are not caused by underlying disease or structural problems, and include migraines, tension-type headaches (TTHs), and the trigeminal autonomic cephalgias (TACs). Migraines and TTHs are the most common primary headaches in children and can have less distinct features in children than they do in adults ( Table 34.1 ). While primary headaches may cause significant pain and disability, they are not intrinsically dangerous. Secondary headaches are caused by an underlying disease, such as infection, tumor, intracranial hemorrhage, or a vascular disorder, and may indicate an innocuous etiology or portend a serious illness. Most headaches in children are primary headaches or harmless secondary headaches. History and physical examination guide the diagnosis of primary headache disorders, assess the degree of headache-related disability, and reveal information that may prompt evaluation for secondary headaches. Each subsequent visit allows for assessment of the response to therapy and consideration of secondary headaches, the causes of which may confer significant morbidity and in rare cases may be life threatening.
| Headache Type | Genetics | Epidemiology | Characteristic Features | Length | Accompanying Symptoms |
|---|---|---|---|---|---|
| Migraine headache | Complex genetics but usually a family history | More frequent in women | Unilateral, bilateral; throbbing; moderate to severe; worsens with activity | Hours to days | Photophobia, phonophobia, nausea and/or vomiting |
| Tension-type headache | Usually a family history | Equal frequency in men and women | Tight bandlike pain; bilateral; pain may be mild to moderate; improves with activity | Hours to days | No nausea or vomiting; small amount of light or sound sensitivity, but not both |
| Cluster headache | May have a family history | More frequent in men | Unilateral severe pain in the face | Minutes to hours | Ipsilateral ptosis, miosis, rhinorrhea, eyelid edema, tearing |
| Paroxysmal hemicrania | Usually no family history | More frequent in women | Unilateral pain in the face | Minutes | Ipsilateral ptosis, miosis, rhinorrhea, eyelid edema, tearing; responds to indomethacin |
| Short unilateral headache with conjunctival injection, tearing | No family history | More frequent in men | Unilateral eye pain; orbit pain | Typically 4 min or less | Conjunctival injection, tearing |
| Hemicrania continua | No family history | More frequent in women | Unilateral continuous headache with episodic stabbing pains | Continuous | Ipsilateral ptosis, miosis, rhinorrhea, eyelid edema, tearing |
The specific headache diagnosis is determined by the headache phenotype, which is defined in terms of laterality, location ( Figs. 34.1, 34.2, and 34.3 ), timing, frequency, duration, quality, severity, associated symptoms, and alleviating and aggravating factors. In most cases, a single phenotypic headache is present. If the patient has more than one type of headache, the clinician must obtain a specific history for each type. Ideally, the history should be obtained from the child, parent, and any other caregivers, including teachers. Even a young child should be given the opportunity to describe the symptoms experienced with each headache episode and may use drawings to do this.
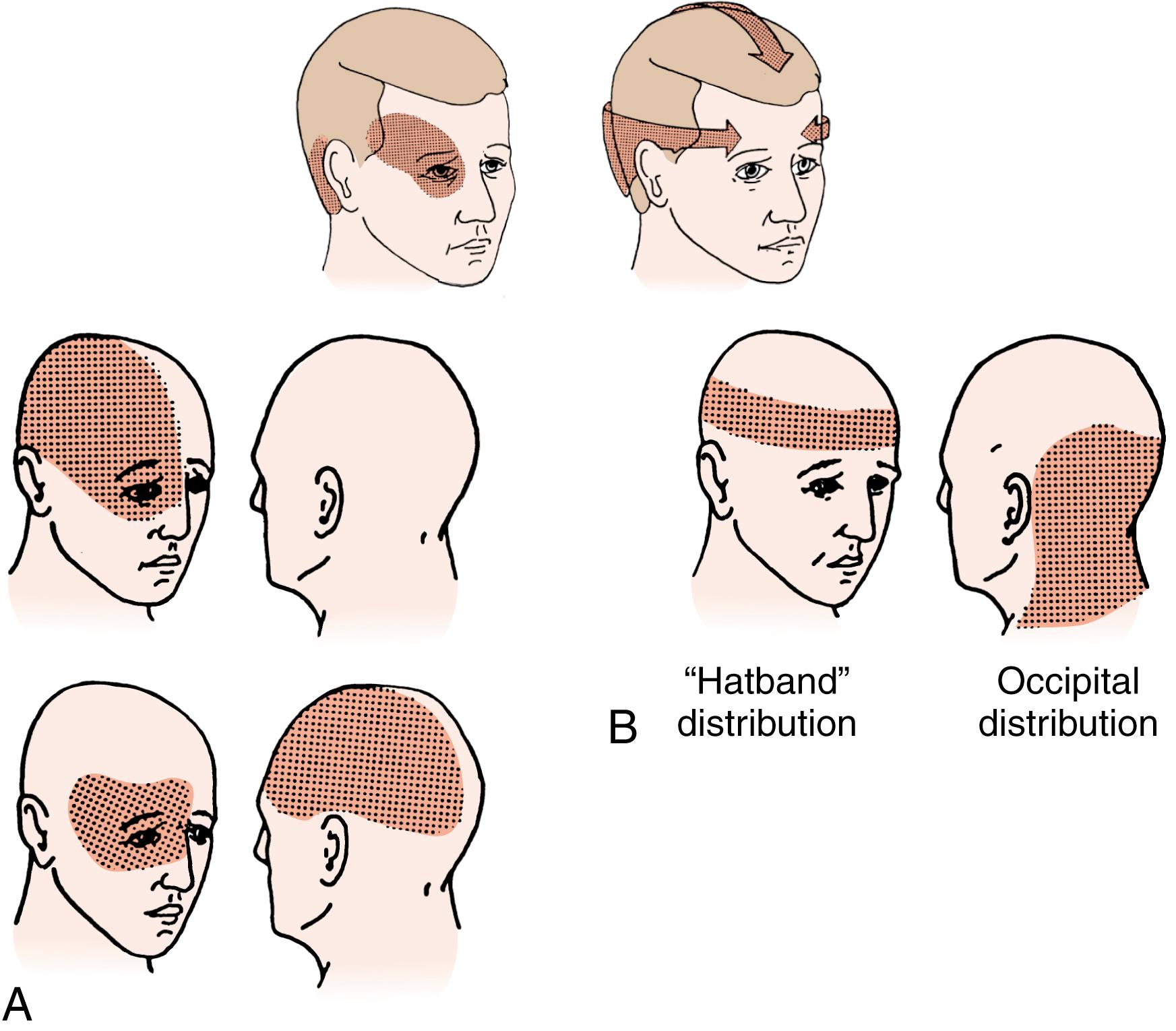
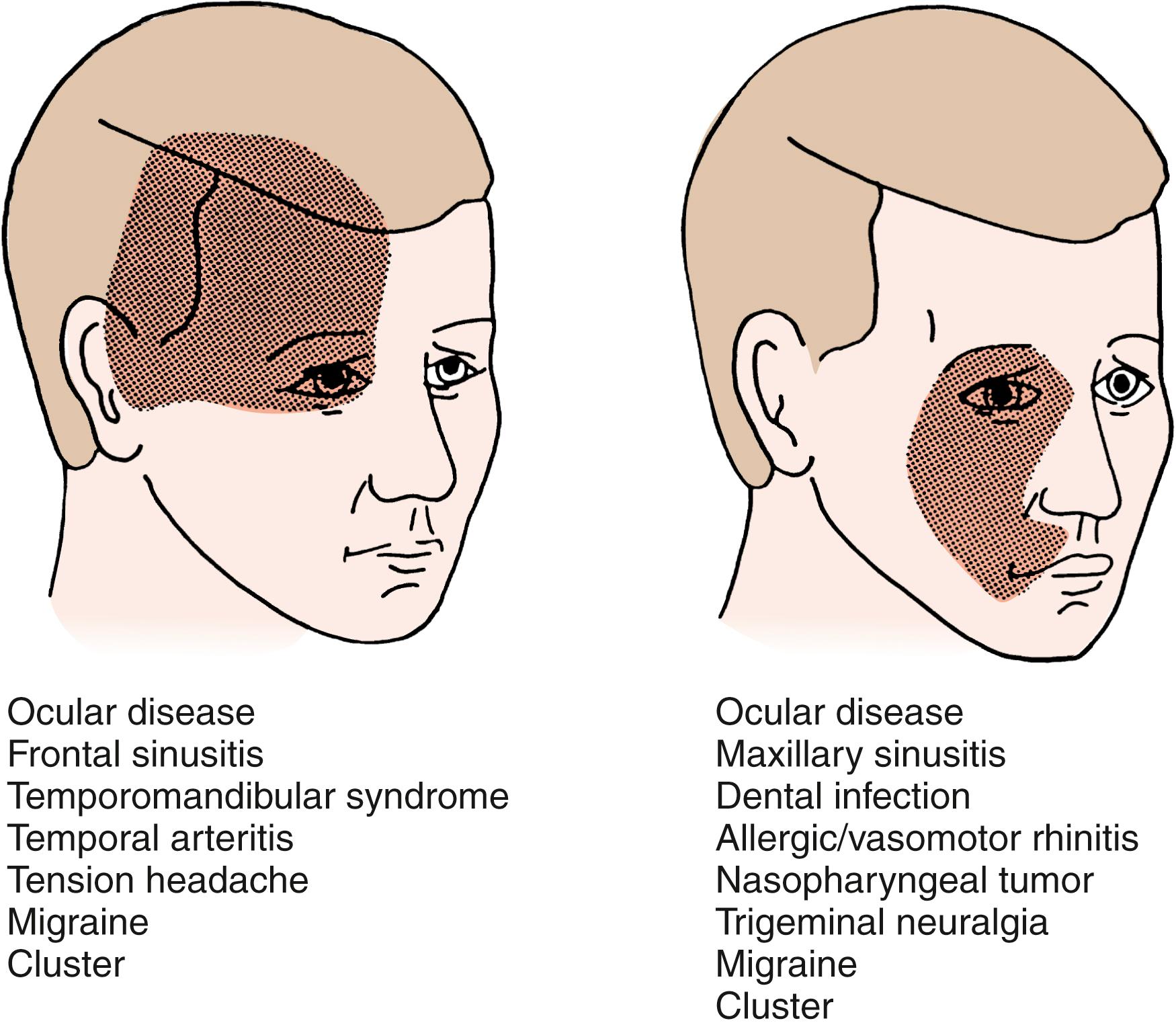
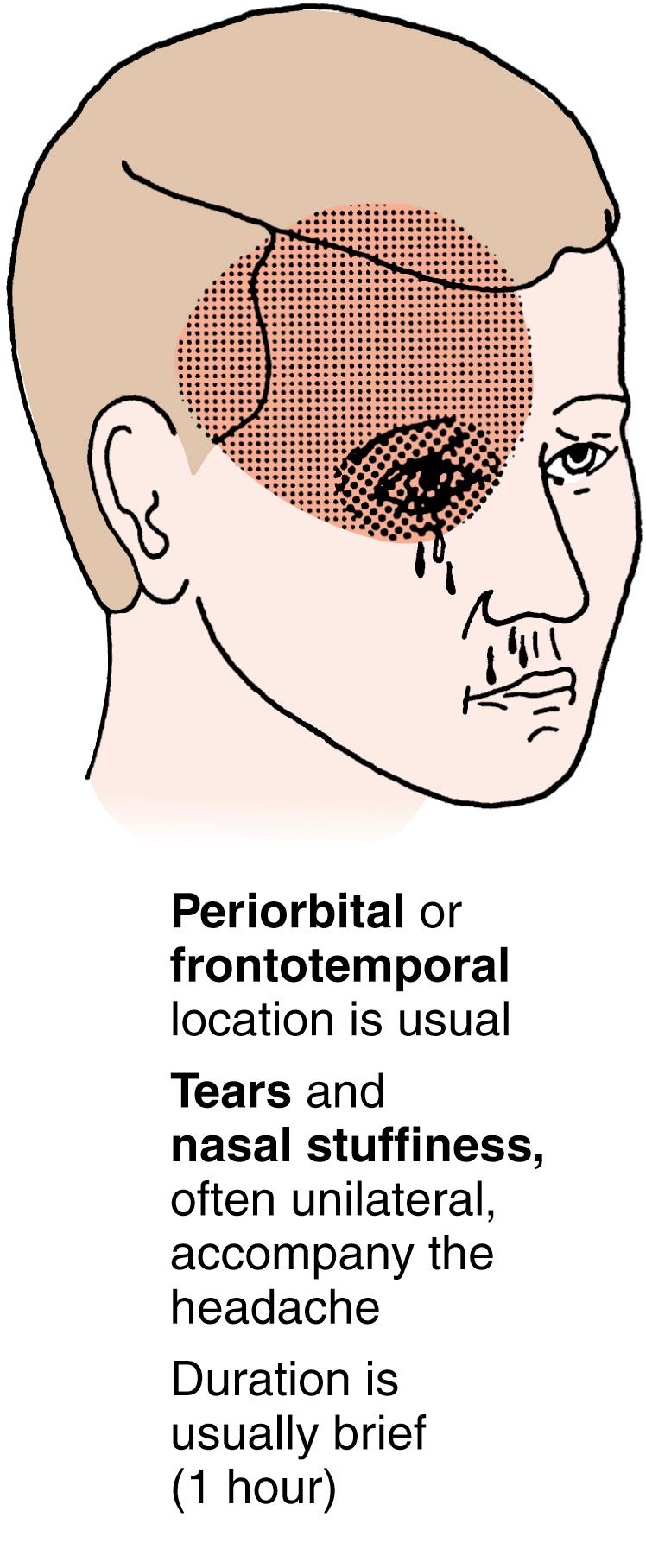
The laterality and location of the pain should be established (see Figs. 34.1, 34.2, and 34.3 ). If the pain is unilateral, it should be noted whether the pain is always on one side or if the side varies. The location may be restricted or more widely distributed; if the location varies from one episode to another, this should be noted as well. Unusual locations in pediatrics may include the occipital region. This location should raise index of suspicion for intracranial pathology if there are abnormal neurologic findings or the headache does not meet criteria for a primary headache disorder.
The timing, frequency, and duration of headaches should be described, as the temporal patterns of headaches are useful in creating a differential diagnosis, identifying the need for work-up, and classifying the type of headache. The temporal categories of headache include acute, acute recurrent, chronic nonprogressive, and chronic progressive ( Table 34.2 ).
|
|
|
|
The severity of a headache does not necessarily correlate with the seriousness of its etiology. Pain caused by brain tumors may initially be mild, whereas the pain of TTHs may be excruciating. Pain is subjective and may be influenced by age, culture, duration, and previous encounters with medical care, leading some patients to unintentionally minimize or exaggerate their pain; as such, pain alone should not be used to narrow the differential diagnosis. An exception to this principle is the thunderclap headache , in which the onset of pain is sudden, reaches maximum severity within seconds, and is often described by patients as the worst headache they have ever had. Such headaches may indicate subarachnoid hemorrhage, arterial dissection, or venous sinus thrombosis, among other causes ( Table 34.3 ). Numerical scales, or visual scales for younger children, are helpful for quantifying pain and determining the efficacy of treatment. In older patients, descriptive phrases, such as mild, moderate, severe, and excruciating , may suffice.
| Main Causes | Rare Causes |
|---|---|
| Vascular Disorders | |
| Subarachnoid hemorrhage Intracerebral hemorrhage Cerebral venous thrombosis Spontaneous intracranial hypotension Cervical artery dissection |
Pituitary apoplexy, arteritis, angiitis Unruptured vascular malformation, aneurysm Arterial hypertension Cerebral segmental vasoconstriction |
| Nonvascular Disorders | |
| Greater occipital neuralgia Intermittent hydrocephalus by colloid cyst |
|
| Infections | |
| Meningitis, encephalitis | Erve virus (European Nairovirus) Sinusitis |
| Primary Headache Disorders | |
| Migraine Primary thunderclap headache Primary exertional headache Primary cough headache |
Cluster headache Tension headache, new daily persistent headache |
Associated symptoms such as hemiparesis, ataxia, visual loss, diplopia, scotomata, vertigo, seizure-like activity, confusion, mood or behavioral changes, autonomic symptoms, and hemisensory occurrences may suggest neurologic dysfunction or a migraine-related aura. Any history of fevers, syncope, nausea, vomiting, and appetite changes should also be ascertained. Special note should be made if the pain awakens the patient from sleep, is present upon awakening in the morning, or worsens when recumbent; these findings may indicate increased intracranial pressure. Events associated with the onset or aggravation of headaches, such as trauma, intake of particular foods, or physical exertion, may provide insight into the etiology of headaches, as well as potential triggers to avoid.
Alleviation via rest or positional changes should be noted, as should the response of the headaches to medications. A thorough medication history is essential for diagnosing analgesic overuse headaches and headaches caused by medication side effects. The use of over-the-counter medication and prescription medications, including medications that have not been prescribed for the patient, should be delineated, as well as the use of any supplements or traditional remedies. Both primary and secondary headaches may respond to medications and such a response is not diagnostic of any specific headache disorder. For example, relief of an acute headache by triptans is not diagnostic of migraine, as triptans may also be effective for other causes of headache.
In patients with recurring headaches, the history may be clarified by keeping a headache diary , which can additionally determine headache patterns, identify triggers, aid diagnosis, and assess the efficacy of therapy ( Table 34.4 ). A headache diary may also assist in determining the degree of disability caused by the headache. Disability evaluation may be augmented by school attendance and performance records. Headaches that improve with the onset of the summer school holiday may suggest that a child is struggling academically or is being bullied at school. In younger children, where detailed personal descriptions of pain may be more difficult to obtain and record in a diary, videos of the headache episodes may aid diagnosis.
|
∗ If more than one type of headache exists, the types should be defined and labeled, and separate data should be recorded for each type.
† Foods are believed to be less associated with triggering migraines than previously.
The past medical history may reveal a risk for potentially serious causes of secondary headaches that require prompt evaluation, such as sickle cell disease, thyroid disorders, parathyroid dysfunction, malignancy, hypercoagulability, hypertension, immunodeficiency, congenital heart disease, autoimmune disorders, and arteriovenous malformations. Allergic rhinitis and other atopic disorders are also associated with headaches. Infantile colic, benign paroxysmal torticollis, cyclic vomiting syndrome, and benign paroxysmal vertigo are considered episodic syndromes that may be associated with migraine and may precede the development of typical migraine symptoms later in life. In females, a menstrual history should be obtained, including details of the cycle and the timing of headaches with respect to the menstrual cycle. A history of secondary amenorrhea could suggest pituitary or other central nervous system neoplasms.
The family history should be probed for any genetic predisposition to migraines, aneurysms, other vascular malformations, early-onset strokes, or brain neoplasms. A negative family history for primary headaches should cause the clinician to be more cautious in assigning the diagnosis of a primary headache disorder. Social history should investigate for psychosocial factors that may influence or be influenced by headaches, such as school performance, the relationships between family members, recent changes in social structure, and substance abuse in the patient or the family. The provider should also screen for indications of neglect or abuse. Detailed psychologic evaluation with screening for symptoms of depression and anxiety may be indicated.
Some historical components are classic features of primary headaches, while others are concerning for secondary headaches ( Table 34.5 ). Throughout the history, the clinician should constantly assess for warning signs of serious and sometimes life-threatening causes of secondary headache. The identification of any of these red-flag symptoms should cause concern and lead promptly to further investigation.
|
Abnormalities in the examination may provide clues to the underlying etiology of secondary headaches, and red flags may identify specific diagnoses of concern ( Table 34.6 ). Vital signs assessment may reveal elevated blood pressure, which may be the cause of headache, signal increased intracranial pressure, or herald an underlying renal abnormality. Fever may be a sign of an infectious or inflammatory process. Growth parameters, including height, weight, body mass index, and head circumference, should be obtained. Poor weight gain may indicate an underlying chronic illness associated with headaches, such as celiac disease, respiratory disorders, neurofibromatosis type 1, or neglect. Obesity should alert the clinician to assess for symptoms of obstructive sleep apnea or idiopathic intracranial hypertension (IIH). Enlarged head circumference associated with signs of headache or other evidence of increased intracranial pressure warrants alarm.
|
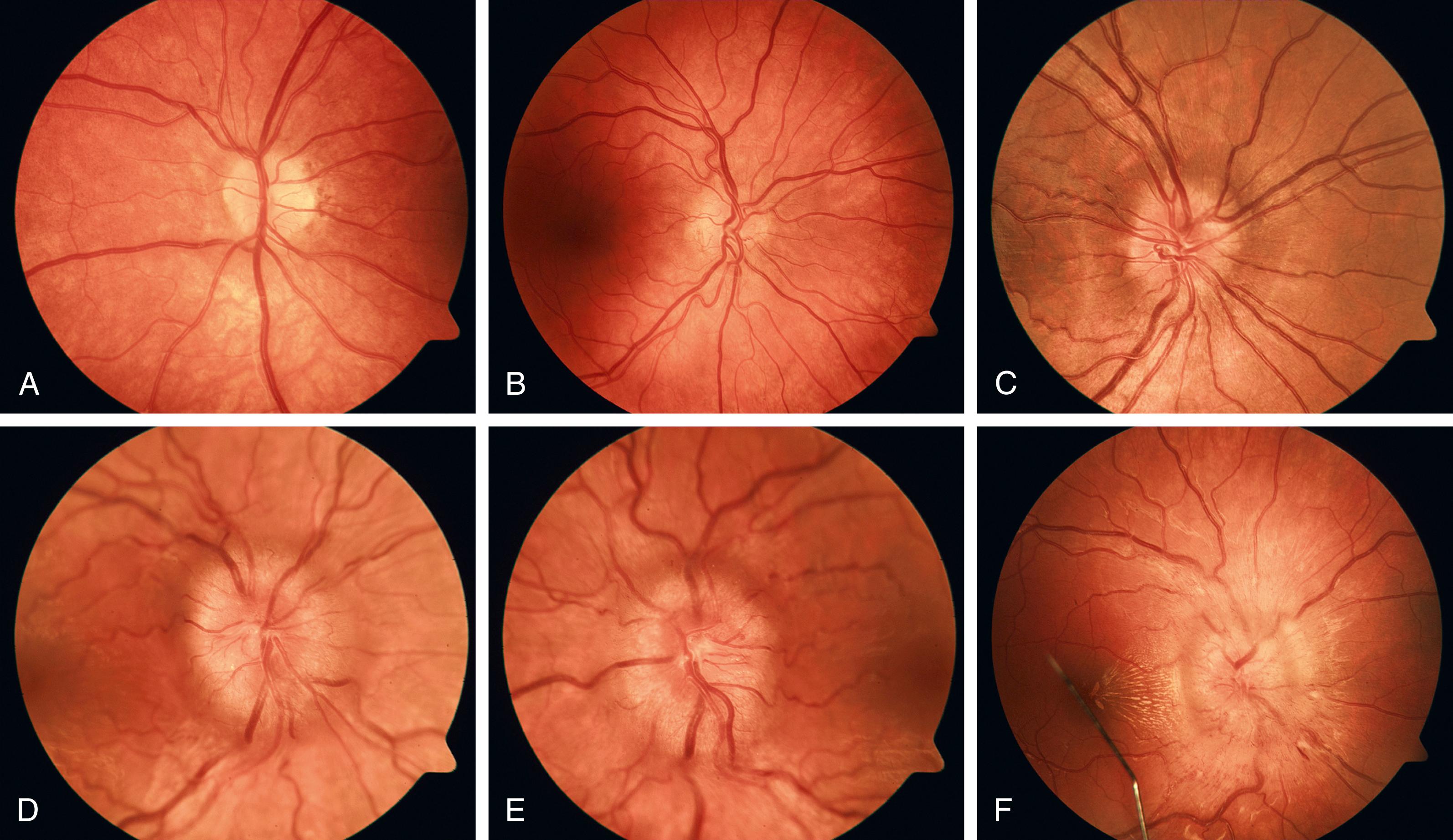
The general examination starts with assessment of mental status and overall level of distress. The head and neck examination should assess specifically for nasal congestion, sinus tenderness, and signs of allergic rhinitis, such as boggy nasal turbinates. Frontal bone tenderness could be an early sign of Pott puffy tumor, a complication of frontal sinusitis. Tenderness over the mandibular condyle in children with dental malocclusion, or jaw crepitus in patients with arthritis, may indicate temporomandibular joint dysfunction as a cause of headache. Thorough lymphatic, respiratory, cardiac, and abdominal examinations should also be completed. Genitourinary examination should include pubertal stage, as headaches may be associated with endocrine disorders. Skin should be evaluated for petechiae, atopic or vasculitis findings, and lesions associated with neurocutaneous syndromes such as neurofibromatosis or tuberous sclerosis. Signs of trauma should be noted. Neurologic examination should be detailed and include assessments of mental status, cranial nerves, auditory function, sensation, motor strength, reflexes, gait, coordination, and speech. Whenever possible, a thorough ophthalmologic examination should be undertaken, including visual acuity testing and a funduscopic evaluation for papilledema ( Fig. 34.4 ). In a young child, much of the neurologic examination is completed through observation or engaging the child in play to elicit findings. A complete ophthalmologic evaluation may be limited by lack of cooperation or comprehension. If the clinician is unable to complete or interpret the neurologic and ophthalmologic assessments, the support of a neurologist and an ophthalmologist may be required. If the results of examination suggest a structural brain lesion or increased intracranial pressure, neuroimaging is warranted ( Table 34.7 ). However, many causes of headache, including some serious diseases early in their course, do not present with abnormal findings on physical examination or have fluctuating abnormal findings ( Table 34.8 ). A single normal physical examination does not exclude pathology; thus, periodic reassessments are essential if headache persists.
| Headache | Pain Profile | Neurologic Sign |
|---|---|---|
| Complicated migraine | AR | Hemiparesis, aphasia, paresthesia, hemianopia |
| Migraine with brainstem aura | AR | Dysarthria, vertigo, tinnitus, hypoacusis, diplopia, ataxia, decreased level of consciousness |
| Acute confusional migraine | AR | Alteration in migraine sensorium, stupor, agitation, fugue state |
| Vasculitis | CP, AR | Seizure, changes in sensorium |
| Brain neoplasm or mass | CP | Papilledema, focal deficit |
| Hydrocephalus | CP, AR | Papilledema, bilateral sixth nerve palsies, increased motor tone, impaired upward gaze and Parinaud syndrome |
| Idiopathic intracranial hypertension | CP | Papilledema, constricted visual fields, enlarged blind spot |
| Subarachnoid hemorrhage, ruptured aneurysm | A | Changes in sensorium, focal neurologic signs, meningismus |
| Subdural or epidural hemorrhage | CP | Focal neurologic signs, papilledema, changes in sensorium |
| Sagittal sinus thrombosis | A | Papilledema, focal neurologic deficits, changes in sensorium, seizures |
| Meningitis, encephalitis | A | Focal neurologic deficits, changes in sensorium, seizures |
| Optic neuritis | A | Papillitis, decreased visual acuity, afferent pupillary defect |
| Headache Disorder | Pain Profile |
|---|---|
| Tension-type headache | CN, AR |
| Migraine without aura | AR, CN |
| Cluster headache | AR |
| Hypertension, uncomplicated | AR, CN |
| Fever | A |
| Anoxia | A |
| Medication overuse | CN |
| Caffeine withdrawal | A, AR |
| Early hydrocephalus or brain mass | CP |
| Cough headache, uncomplicated | AR |
| Meningitis, uncomplicated | A |
| Sinusitis, dental or pharyngeal abscess | AR |
| Temporomandibular joint syndrome | CN |
| Postconcussive syndrome | CN |
| Conversion disorder | CN |
Most children do not require neuroimaging for headaches, and it is rarely indicated in children with recurrent headaches and a normal neurologic and ophthalmologic exam. Neuroimaging should be considered when the headache history or symptomatic progression is incompatible with a primary headache disorder or if there is no family history of primary headache disorder. Furthermore, neuroimaging in the assessment of headaches in children is indicated when the following features are present: abnormal neurologic exam or historical findings; new onset of afebrile seizures or alteration in seizure type or frequency; new severe headache; change in frequency or severity of headaches; headache consistent with increased intracranial pressure; association of headache with cough or bending over; concerning past medical history components, including trauma or presence of a ventriculoperitoneal shunt; and age younger than 6 years ( Table 34.9 ). In specific cases, neuroimaging may be considered when there is history of a brain tumor in the family, fear by the patient or the parents of underlying pathology, or inability to obtain an accurate physical examination due to lack of patient cooperation.
|
MRI and CT are the neuroimaging modalities to consider ( Table 34.10 ). CT remains the most sensitive and rapid method for detecting acute intracranial bleeding and is preferred in emergency situations or when MRI is contraindicated or unavailable. MRI is otherwise the preferred imaging modality, offering superior visualization of soft tissue contrast and gray-to-white matter differentiation without exposing the patient to the ionizing radiation associated with CT scanning. While gadolinium contrast for MRI is considered safe, it is not usually necessary. An MRI contrast study should be considered when there is concern for infection or if the noncontrast study is abnormal. MRI may involve the need for sedation, particularly in younger children. Normal neuroimaging and a single normal neurologic examination should not give complete reassurance. Follow-up assessment of ongoing symptoms or for changes in the physical examination remains necessary.
| Advantages of MRI |
|
| Advantages of CT |
|
Routine blood work is not indicated when history suggests a primary headache disorder and physical and neurologic examinations are normal. Findings in the history, physical examination, or neuroimaging that dictate directed laboratory evaluation are listed in Table 34.11 .
| Laboratory Test | Possible Cause of Headache |
|---|---|
| CBC | Infection (elevated white blood cell count); bleeding diathesis (thrombocytopenia); anemia |
| CSF examination with opening pressure | Infection, vasculitis, pseudotumor cerebri, subarachnoid hemorrhage after CT is normal |
| Toxicology assays | Substance abuse, possible toxin exposure, carbon monoxide |
| Hypercoagulation panel | Unexplained venous sinus thrombosis |
| ESR, ANA, ANCA | Vasculitis |
| Genetic tests | Familial hemiplegic migraine, MELAS, CADASIL, CARASIL |
| EEG | Seizure disorder |
| Electrolytes, ECG, UA | Hypertension, renal disease |
| VP shunt radiographic series | Malfunctioning VP shunt |
| Blood glucose | Hypoglycemia or hyperglycemia |
| Serum calcium | Hyperparathyroidism |
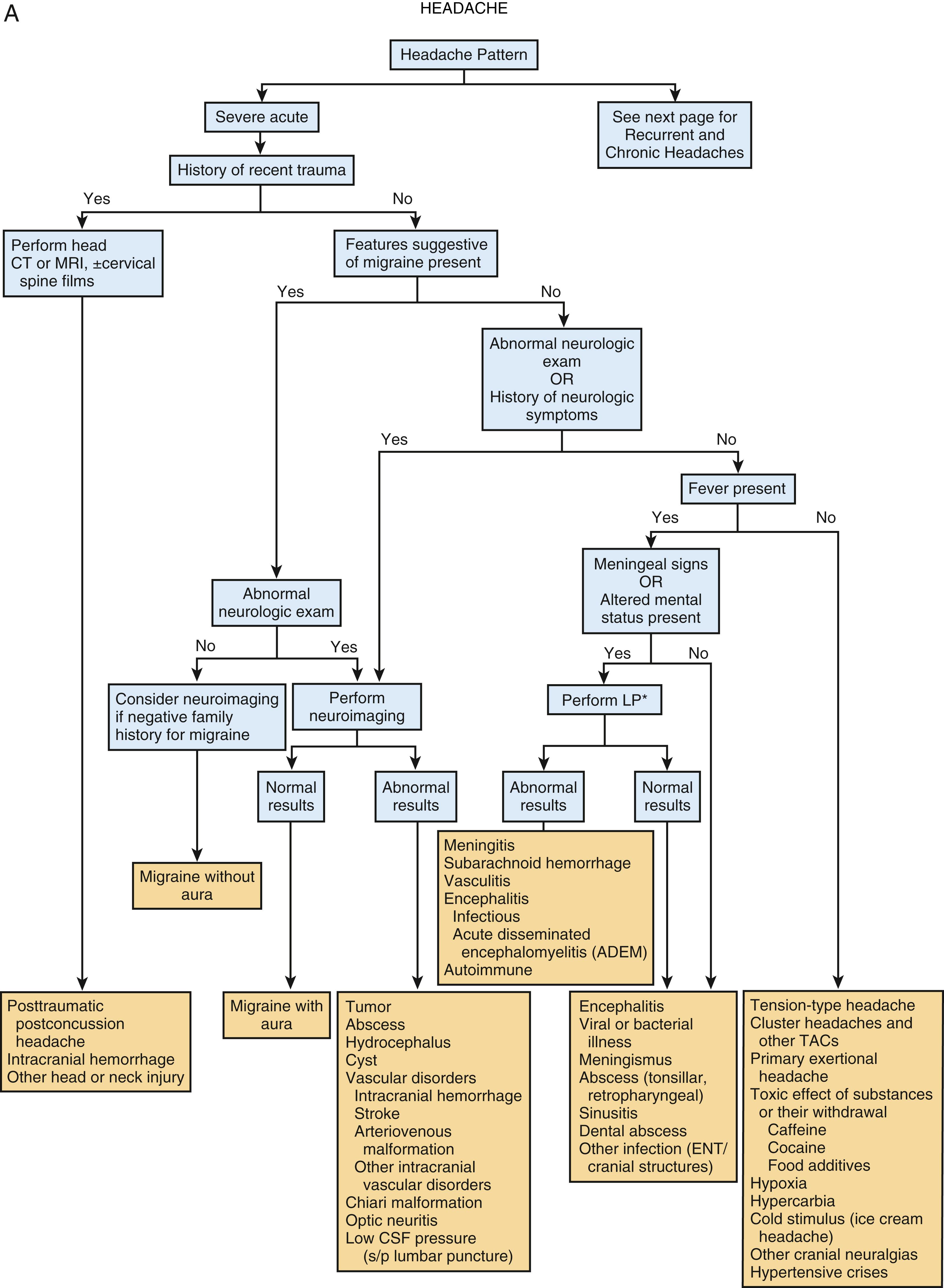
Headaches are classified broadly as primary or secondary. The acuity or chronicity of the headache helps to guide the development of the differential diagnosis ( Fig. 34.5 ).
There are three categories of primary headaches: TTH, migraine headache, and the TACs. TTH and migraine are the most common headache types in children and adolescents.
TTHs are common in pediatrics with a broad prevalence range reported. These headaches have a typical pattern. Patients awaken feeling well, with pain beginning gradually and escalating throughout the day. Pain is constant, squeezing, nonpulsatile, and located in a band extending from the front of the head, across the temples, and toward the occiput or neck. Photophobia and phonophobia may accompany these headaches but are not a constant feature; patients with TTH typically do not experience both photophobia and phonophobia in the context of a single episode. Unlike migraine headaches, routine physical activity does not tend to influence the severity of the headache. In patients with long-standing pain, the headaches may assume characteristics of migraines; indeed, TTHs often accompany other headache disorders.
TTHs are classified by the International Classification of Headache Disorders-3 (ICHD-3) as either episodic or chronic. Both episodic and chronic TTHs are further classified as having associated pericranial tenderness or as lacking such tenderness. This tenderness is typically present between headaches and increases during episodes. Episodic tension-type headache (acute recurrent) is categorized as either infrequent or frequent. Infrequent episodic TTH is defined as 10 or more episodes total, occurring less than once per month on average. Frequent episodic TTH is defined as 10 or more episodes total, occurring on 1–14 days per month on average for over 3 months. Individual episodes of either may last from 30 minutes to as long as a week and have at least two of the following features: (1) bilateral location, (2) pressing or tightening (nonpulsating) quality, (3) mild or moderate intensity, and (4) not aggravated by routine physical activity such as walking or climbing stairs. Nausea or vomiting must be absent; if present, migraine should be considered. Either photophobia or phonophobia may be present; if both are present simultaneously, migraine should be considered. Chronic tension-type headaches are defined as headaches occurring at least 15 days a month for over 3 months, with features otherwise similar to episodic TTHs.
Psychosocial history may uncover the cause of the headache. Adjustment disorders and depression may be either the underlying causes or reactions to chronic pain. Sleep disturbances, school absences, and chronic analgesic use are common. In some highly motivated and successful children, the headaches may be a reaction to the stress associated with achievement. In this instance, school attendance is usually perfect, and the patient continues to achieve in all realms. However, some patients with chronic TTH may lack a contributory psychosocial history, and the severe subtypes of TTH are now thought to have a neurobiologic foundation.
Patients with TTHs have normal neurologic and physical findings, except for possible tenderness along the affected muscles. These muscles often feel tight, and palpation may trigger the pain. Laboratory tests are not required in the evaluation of TTHs.
The diagnosis of migraine headache is typically based on the historical description of episodes. Migraine and migraine variants occur in early childhood but with an unknown prevalence, as diagnostic criteria for migraine are often insufficient in young children and infants ( Table 34.12 ). Several features distinguish migraine in children from adult migraine. In children, the headaches are shorter, ranging from 2 to 72 hours, and pain tends to be frontotemporal rather than unilateral. Vomiting and abdominal pain are more common in children than in adults, and while photophobia and phonophobia may be present in children, they may need to be deduced by behavior changes rather than by child report. Thus, 5- to 10-year-old children may present with bilateral frontal headaches and associated abdominal pain, nausea, vomiting, photophobia, phonophobia, and a desire to sleep. Unilateral temporal headache location develops in late adolescence, with onset of aura typically in middle school. A family history of migraines is common, with reports of up to 90% of pediatric patients having a first- or second-degree relative with recurrent headaches.
|
The prevalence of migraine headaches increases with age throughout childhood and is higher in females following the onset of puberty. While the diagnosis of migraine is typically made later in childhood, a careful retrospective history of infancy and early childhood events may reveal early episodic symptoms consistent with migraine, including pallor, vomiting, fussiness, and sleepiness occurring outside the context of concurrent illnesses. Furthermore, benign paroxysmal torticollis, cyclic vomiting syndrome, and benign paroxysmal vertigo are episodic syndromes that may be associated with the diagnosis of migraines later in life.
Certain exposures trigger migraine attacks in susceptible patients. Precipitants include hunger, dehydration, heat or weather changes, exertion, sleep deprivation or irregularity, substance exposures or withdrawal, and psychologic triggers. Food triggers are now thought to be less common than previously believed. In postmenarchal females, migraines may cluster around particular phases of the menstrual cycle.
Migraines are categorized based on the presence or absence of an associated aura. Migraine without aura is the most common migraine phenotype in pediatric patients.
Criteria assist in the diagnosis of migraine without aura and are based on the number and duration of episodes, as well as symptoms and associated findings ( Table 34.13 ). Children may have shorter-duration headaches. The pain onset is typically gradual and is dull and constant. At times, though, the pain of an episode may be sudden and severe, prompting concern for a thunderclap headache. More typically, pain increases in severity over the course of an individual episode and becomes throbbing. As the headache proceeds, the pain may generalize to the entire cranium. Intense nausea often accompanies migraines, with occasional vomiting. Skin pallor is a common finding. Nasal congestion and tearing may be present. Because most patients are sensitive to motion, light, and noise during a migraine attack, they search for a dark and quiet place to sleep. The patient usually awakens within hours feeling fatigued but pain free.
|
In migraine with aura, the headache is preceded by sensory signs or symptoms termed an aura , which is caused by vasoconstriction and diminished blood flow to the affected region of the brain ( Table 34.14 ). In migraine with typical aura ( Table 34.15 ), the aura is visual and may consist of blurred vision, spreading scintillating scotomata, flashing lights, zigzag lines, and hemianopia. These features typically last less than 60 minutes. Less classic visual disturbances may occur in children. Sensory auras are less common than visual auras and may consist of numbness or tingling.
Visual
|
Basilar
|
Other
|
∗ Migrating paresthesia: hand to arm to face to lips to tongue.
|
Aura should not be confused with a prodrome, which may include anxiety, fatigue, hunger, thirst, nausea or depression. A prodrome may last many hours before a migraine, while an aura usually lasts less than 60 minutes.
Further types of migraine with aura are classified by the specific aura symptoms.
Migraine with brainstem aura ( Table 34.16 ), previously known as basilar artery migraine , has aura limited to brainstem symptoms such as dysarthria and ataxia. In some patients, the headache may be a minor component of the syndrome. Visual changes may also occur and may include vivid visual images. Vertigo and tinnitus are less common symptoms. Diplopia, vertigo, and vomiting should prompt evaluation for a posterior fossa abnormality, such as a mass or a vascular malformation.
|
Hemiplegic migraine has an aura that consists of motor weakness and visual, sensory, and/or speech/language symptoms that are fully reversible. Both familial and sporadic forms have been described. The familial hemiplegic migraine is an autosomal dominant disorder with genetic variants described in three separate genes: CACNA1A , ATP1A2 , and SCN1A .
Retinal migraine involves monocular visual disturbances that are fully reversible. This migraine subtype is extremely rare, and other causes of the vision disturbance should be investigated prior to designating this diagnosis (see Chapter 43 ).
The episodic syndromes that may be associated with migraines , previously termed childhood periodic syndromes, are a group of potentially related symptoms that occur with increased frequency in children with migraine. The hallmark of these symptoms is the recurrent episodic nature of the events. These include gastrointestinal-related symptoms (recurrent gastrointestinal disturbance, cyclic vomiting syndrome, and abdominal migraine), benign paroxysmal vertigo, and benign paroxysmal torticollis.
Acute confusional migraine and Alice in Wonderland syndrome are headache conditions that occur primarily in children. Acute confusional migraine, which can be triggered by minor head trauma or have no precipitating event, usually converts to typical migraine with age. Episodes consist of alteration in consciousness, which may include lethargy, agitation, and dysphagia. Attacks last a few hours, with the child eventually falling asleep. The child awakens without memory of the incident. Alice in Wonderland syndrome is characterized by perceptual disturbances in which the sense of proportion or distance, particularly with respect to the body, is distorted. While in adults this syndrome is associated with migraine episodes, Epstein-Barr virus infection seems to be the most common trigger in children. Migraine mimics are noted in Table 34.17 .
|
Status migrainosus is defined as a migraine headache that lasts over 72 hours with debilitating pain or associated symptoms. Diagnosis is based on a propensity for previous prolonged migraine attacks. Some patients have an aura that lasts longer than 1 week, termed persistent aura without infarction . Conversely, when an aura symptom persists for greater than an hour and neuroimaging demonstrates associated ischemic infarction , migrainous infarction is diagnosed. Patients can also have migraine aura-triggered seizures that occur during or within 1 hour of a migraine with aura.
Trigeminal autonomic cephalgia is rare in children under 7 years of age but has been reported in a child as young as 3 months. Onset typically occurs during adolescence or adulthood. Cluster headaches and paroxysmal hemicranias are types of TAC (see Table 34.1 ).
Cluster headaches are characterized by episodes of pain interspersed between long periods of remission ( Table 34.18 ). Prevalence in childhood is estimated to be between 0.03% and 0.1%; the disorder is more common in males. Pain is unilateral and localized to the orbital, supraorbital, and/or temporal region. The pain begins suddenly and rapidly increases to an excruciating level. Cluster headaches may be as short as 15 minutes or may last as long as 3 hours; episodes tend to be shorter and less frequent in children. Associated findings include ipsilateral conjunctival injection and/or lacrimation, nasal symptoms, eyelid edema, sweating, miosis, and/or ptosis. Children may have less prominent autonomic features than adults and are most likely to experience lacrimation, conjunctival injection, and nasal discharge. A patient may find it impossible to rest and become agitated and restless during an attack, which is in contrast to migraines, during which the patient becomes quiet and withdraws to a dark, cool room for sleep. However, restlessness may not be as severe or characterizable in children, so observation of behavior is very important.
|
∗ During part, but less than half, of the active time course of cluster headache, attacks may be less severe and/or of shorter or longer duration.
† During part, but less than half, of the active time course of cluster headache, attacks may be less frequent.
Cluster headache is categorized as either episodic or chronic. Episodic cluster headaches occur in a series that may last for a week to months, separated by remission periods of months to years, whereas chronic cluster headaches are defined as occurring for at least 1 year without such a remission period or with remission periods that last <3 months. Cluster headaches are more common in individuals who smoke tobacco.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here