Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Gynecologic specimens are removed for a wide variety of both benign and malignant lesions.
In addition to age, clinical history is often necessary or helpful for the interpretation of specimens from the uterus ( Table 19.1 ).
| HISTORY RELEVANT TO ALL SPECIMENS | HISTORY RELEVANT FOR SPECIMENS FROM THE UTERUS |
| Organ/tissue resected or biopsied | Date of last menstrual period or if postmenopausal |
| Purpose of the procedure | Current or recent pregnancy. |
| Gross appearance of the organ/tissue/lesion sampled | Use of exogenous hormones (type and duration) or hormonal treatment (e.g., tamoxifen) |
| Any unusual features of the clinical presentation | Family history of breast or ovarian carcinoma (including BRCA1 or BRCA2 mutation and Li-Fraumeni syndrome), history of Lynch Syndrome (hereditary non-polyposis colorectal cancer syndrome or HNPCC syndrome) |
| Any unusual features of the gross appearance | |
| Prior surgery/biopsies - results | Abnormal bleeding |
| Prior malignancy | |
| Prior treatment (radiation therapy, chemotherapy, drug use that can change the histologic appearance of tissues) | |
| Compromised immune system |
The endometrium is biopsied to evaluate abnormal bleeding in pre and post-menopausal women, to monitor patients at high risk for endometrial carcinoma (e.g., women taking tamoxifen), and in the evaluation of infertility.
For patients with trophoblastic disease, important clinical information includes the week of the pregnancy, passage of tissue, prior history of hydatidiform mole (or any gestational trophoblastic disease), and the serum human chorionic gonadotropin level.
The specimen must be described in terms of appearance and composition (soft tissue, blood clot, and/or mucous). The aggregate dimension is provided in centimeters. The entire specimen is submitted for microscopic evaluation. Routine evaluation is the following in many institutions:
One level is examined for women < 45 years of age when the clinical setting is suspected luteal phase defect, increased bleeding to suspected polyps, or endometritis.
Three levels are examined for women ≥ 45 years of age or for women of any age with a history or clinical question of atypical endometrial hyperplasia (endometrial intraepithelial neoplasia = EIN) or carcinoma.
Laparascopic minimally invasive surgery with morcellation of the uterus was developed to remove fibroids and to avoid open surgery. However, after power morcellation, some women without a history of malignancy subsequently presented with metastatic leiomyosarcoma or uterine carcinoma in the peritoneal cavity, presumably related to the prior procedure, resulting in the death of some patients. According to the Food and Drug Association (FDA), unsuspected uterine sarcoma may be present in as many as 1 of 225 to 1 of 580 women considered for this procedure. The FDA recommended against the use of morcellators in 2014 and reaffirmed this recommendation in 2017. In 2020, The FDA updated their recommendations to state that this technique should only be performed with a tissue containment system, legally marketed in the United States for use during laparoscopic power morcellation, and that these procedures should only be performed in appropriately selected patients (fda.gov/medical-devices/safety-communications; accessed July 23, 2021). The technique should not be used for patients with known or suspected malignancy or patients with suspected fibroids who are post-menopausal or >50 years of age, or who are candidates for removal of tissue (en bloc) through the vagina or via a mini-laparotomy incision.
In carefully selected women clinically thought to have benign disease, the incidence of malignancy ranges from 0.02% to 3%, but in the majority of studies is <1%. Malignancies have included endometrial carcinoma, leiomyosarcoma, endometrial stromal sarcoma, mixed mullerian mesodermal tumor, and others.
The uterus, with or without the fallopian tubes, is fragmented and removed through a small incision. In the original technique, there was no containment and the fragments could become dispersed in the peritoneal cavity. The procedure is now modified by morcellating the uterus within a bag placed into the abdomen and then removed. However, more experience will be needed to determine if containment methods completely eliminate the risk of spreading disease.
If the specimen is morcellated by hand, there will be multiple irregular fragments of tissue. If a power morcellator is used, the specimen consists of multiple roughly cylindrical fragments of tissue. The prosector must look for all possible components of the specimen (endometrial surface, serosal surface, uterine wall, fibroids, cervical mucosa, fallopian tubes) and record whether they are grossly apparent or absent. Because it can be difficult to recognize all of these elements, extensive sampling may be prudent. The endometrial surface may be difficult to identify as damage by the morcellator to tissue from the uterine wall may result in softening and mimic an endometerial lining.
Any abnormal appearing tissue should be sampled as well as representative samples of each recognizable tissue type. How extensively normal appearing tissue should be sampled has not been studied. In two studies, surgeons introduced blue dye into the uterus preoperatively which aided in this identification endometrium. , However, this technique is not commonly utilized. It has been recommended that if the initial sections show atypical endometrial hyperplasia/endometrial intraepithelial neoplasia (EIN) or endometrial carcinoma, that the entire endometrial lining and adjacent myometrium be submitted. If cancer is detected, it may not be possible to provide a stage due to the fragmentation.
Weigh the specimen, measure the fragments in aggregate, and estimate the number of fragments.
Grossly identify fragments with structures that are expected to be in the specimen:
Serosal surface with myometrium
Endometrium with myometrium
Myometrium and fibroids
Cervix
Tube and fimbriae
Representative sections of each type of normal tissue as well as any abnormal tissue are submitted in 10 to 12 cassettes. If the cervix can be oriented, the anterior portion is inked blue and the posterior portion inked black. The paracervical soft tissue is inked blue if the cervix cannot be oriented.
If the initial sections show atypia or malignancy, additional sampling should be considered.
Received fresh, labeled with the patient’s name, medical record number, and “Uterus and cervix” are multiple fragments of pink-tan, rubbery, morcellated soft tissue (133.0 g; 9.4 × 7.5 × 5.2 cm). The specimen cannot be oriented due to fragmentation. Multiple fragments display overlying areas of smooth and glistening serosal surface. There is an intact, amputated cervix displaying pink-white, smooth, and glistening exocervix (3.5 × 3.3 cm), with a slit-like cervical os (1.2 cm in length). The paracervical soft tissue is inked blue. The intact portion of endocervical canal (2.5 cm in length) displays tan-pink, herringbone mucosa. There are multiple fragments that display pink red, smooth, glistening endometrial surface (0.1 cm in average thickness). On sectioning, soft tissue ranges from pink-tan and trabecular to tan-white and whorling. There are no areas of necrosis, hemorrhage, calcification, or cystic degeneration grossly noted. No fallopian tubes or ovaries are included. Representative sections are submitted for microscopic evaluation.
Micro A1-A2: Cervix, one fragment each.
Micro A3-A4: Lower uterine segment, one fragment each.
Micro A5-A6: Endometrium, multiple fragments each.
Micro A7-A10: Tan-white, whorling to pink-tan, trabecular soft tissue, 2 fragments each. A11-A12: Myometrium and serosal surface
The type of hysterectomy (total or radical) and the disease (benign or malignant) determines the method for processing the specimen. Total abdominal hysterectomy and bilateral salpingo-oophorectomy are often referred to as TAH-BSO. Specimens fall into three categories:
Total hysterectomies for benign conditions (e.g., prolapse, fibroids, or complications post-partum).
Total hysterectomies for malignant conditions (e.g., endometrial carcinoma).
Radical hysterectomies for malignant conditions (e.g., cervical carcinoma) that include vaginal cuff, parametrium, and regional lymph nodes.
Gravid hysterectomies are performed for emergency situations involving severe post-partum hemorrhage that cannot be controlled medically (due to placenta accreta spectrum, uterine atony, or other causes). These specimens are unusual and may have medico-legal implications.
The uterus should be oriented to identify the anterior wall and the posterior wall by using anatomic landmarks ( Fig. 19.1 ). If the adnexa are attached, proceeding anterior to posterior are the round ligament, the fallopian tube, the ovary, and finally the ovarian ligament.
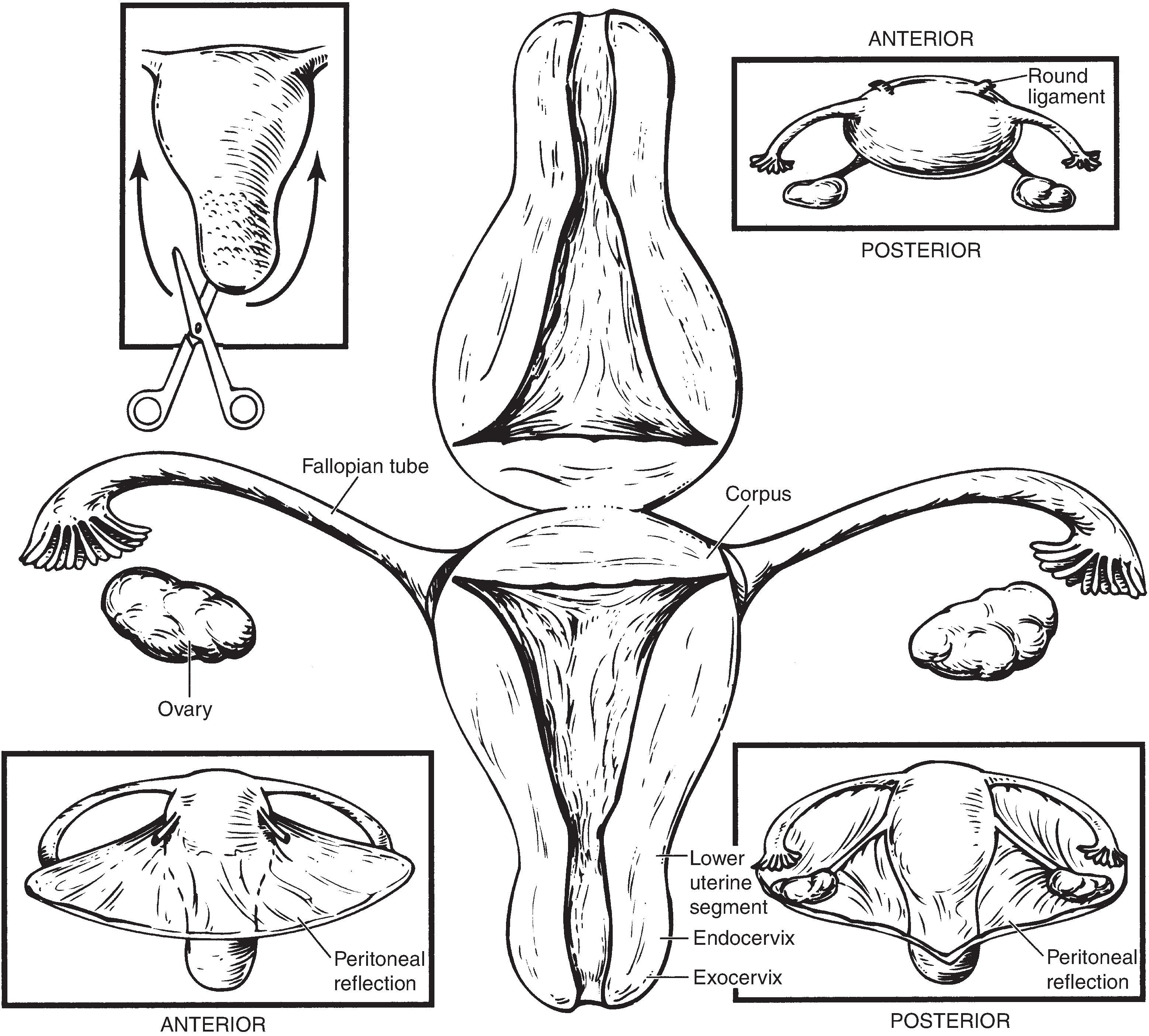
The peritoneal reflection is lower on the posterior surface and often comes to a point. It is higher and blunter on the anterior surface where the bladder has been dissected away, often leaving a loose flap of serosal surface at the reflection. Scars can also be identified within the lower uterine segments of patients who have had prior cesarean sections. These can also be helpful landmarks on difficutl to orient cases.
If a specimen cannot be oriented, designate the two sides “A” and “B” when submitting sections. Arbitrary blue and black ink colors can be used to identify the paracervical magins.
Weigh the specimen. The weight of the specimen is used to determine the Current Procedural Terminology (CPT) code for reimbursement (CPT 58570 if ≤250 grams and CPT 58572 if >250 grams) and must be recorded by candidates applying for certification by the American Board of Obstetrics and Gynecology
Orient the specimen as to anterior and posterior. Ink the anterior paracervical margin block and the posterior paracervical margin black.
Examine the serosal surface for adhesions, endometriosis, tumor implants, or inflammation and describe.
Record the overall dimensions of the uterus (three dimensions), tubes (length and diameter), and ovaries (three dimensions).
Record the dimensions of the exocervix (two dimensions) and the diameter and shape (round or slit-like) of the external os. Describe the appearance (smooth, white, glistening) and any lesions of the cervix (ulcerated, irregular, granular). In cases of uterine prolapse, a vaginal cuff may be present and should be described.
Specimens received as supracervical hysterectomies should be documented grossly, and prior to opening the uterus, the anterior portion of the anterior site should be inked blue and the posterior inked black. If the supracervical hysterectomy cannot be oriented, the amputation site can be inked arbitrarily with blue and black ink with the sides designated “A” and “B” when submitted sections.
Open the uterus along the lateral margins from the external os to the cornu with scissors. Never use a scalpel. A probe placed within the os is helpful to guide the scissors. Transverse (horizontal) incisions are made through the entire mucosa to, but not through, the serosa. The mucosa should not be abraded by touching and should not be rinsed with water. If cleaning is needed, use sterile saline.
Describe the endometrial cavity and lining including size (cornu to cornu, fundus to endocervical canal), distortion (by leiomyomas), color (tan, hemorrhagic), thickness, and any lesions. If lesions are present describe location (anterior or posterior wall), size, color, consistency, and depth of penetration into myometrium.
Describe the endocervix including size (length and width), color, normal herringbone pattern, and any lesions. Describe the ectocervix (color) and note the presence of any lesions. If a lesion is present, describe the clock position and size (length parallel to the canal, radial dimention, and thickness).
Describe the myometrium including average thickness, normal trabeculated pattern, or adenomyosis (coarse trabeculations or cystic hemorrhagic areas). If leiomyomas are present describe number, size (or range in size if many), location (subserosal, mural, submucosal, anterior or posterior), color, presence of hemorrhage or necrosis, or calcification, or variation in pattern.
Describe each fallopian tube (see separate section for instructions on sampling).
Describe each ovary (see separate section for instructions on sampling).
Hysterectomies for benign disease can have sections taken from unfixed tissue and the remainder of the specimen can be saved in formalin. If the specimen is to be fixed before sectioning, the uterus should be opened and placed in fixative within an hour, if possible, to ensure adequate fixation.
For certain high risk patients, the entire endometrial surface should be examined (including the lower uterine segment), even in the absence of any gross lesion, as small and/or grossly inconspicuous carcinomas may be present. Examples of high risk patients include the following:
Biopsy proven endometrial intraepithelial neoplasia (EIN) or repeated biopsies raising suspicion for EIN.
A concurrent ovarian endometrioid carcinoma.
A concurrent estrogen-producing tumor (e.g., a granulosa cell tumor).
Known germline mutations causing Lynch syndrome (HNPCC syndrome) or PTEN (Cowden syndrome).
If the patient has a BRCA1 or BRCA2 mutation, the entire endometrium (but not the entire endo-myometrium) should be submitted if feasible . The fallopian tubes should be examined using the SEE-FIM protocol (see under “Fallopian Tube”) and entirely submitted along with the ovaries.
| Cervix | Anterior and posterior cervix taken to include both exo and endocervix and the transformation zone. |
| Lower uterine segment | One transmural section from each of the anterior and posterior sides. |
| Endometrium and myometrium | One endometrial full thickness section from the anterior and one from the posterior walls. If the myometrium is very thick, include only a portion of wall. Sample any lesions (e.g., polyps). If grossly normal leiomyomata are present, section through each one and sample with up to four cassettes with two fragments each. More sections are taken if there are areas of necrosis, hemorrhage, or areas of unusual appearance. |
| If the hysterectomy is supracervical, take a section perpendicular to the resection margin (after inking) to determine at what level (endocervix or lower uterine segment) the resection was performed. If all endometrium is not removed, the patient may be at risk for developing carcinoma and decisions concerning hormonal treatment could be affected. | |
| Serosa | If serosa is not included in the sections of endometrium, submit a separate section. |
| Fallopian tubes | Submit right and left tubes in separate designated cassettes. |
| Amputate the fimbria and serially section the remainder of the tube to examine for lesions and patency. Submit the entire fimbria radially sectioned, as well as representative sections of mid-proximal tube in all benign cases (including hysterectomies for leiomyomata). | |
| If the patient has current or prior uterine or pelvic epithelial malignancy, or has a positive family history of breast or ovarian cancer, or the procedure was a risk-reducing salpingo-oophorectomy, use the SEE-FIM protocol to completely submit the fimbriae and tubes (see under “Fallopian Tube”). | |
| Ovary | Serially section the ovaries transversely to the long axis and submit one representative section from each grossly normal ovary including the capsule. This section can be submitted with the fallopian tube in the same cassette. |
| Note: If the woman has a personal or family history of breast carcinoma or ovarian carcinoma, the adnexal structures should be ENTIRELY submitted, including soft tissue. |
The specimen is received fresh labeled with the patient’s name, medical record number, and “uterus, cervix, fallopian tubes and ovaries” and consists of a (125.0 g) hysterectomy specimen including uterus (9.5 × 5.2 × 3.4 cm), bilateral ovaries (right: 3.0 × 1.8 × 0.8 cm, left: 3.2 × 1.6 × 1.0 cm), and bilateral fimbriated fallopian tubes (right: 8.8 cm in length x 0.5 cm in diameter, left: 9.4 cm in length x 0.5 cm in diameter). The serosal surface is tan-pink, smooth and glistening, with no fibrous adhesions noted. The exocervix (3.5 × 3.4 cm) is pink-white, smooth and glistening, with a circular os (0.6 cm in diameter). The anterior paracervical tissue is inked blue and the posterior inked black. The endocervical canal (3.0 cm in length) is tan and glistening, with a herringbone mucosa. The endometrial cavity (3.2 cm cornu to cornu x 5.0 cm in length) is lined by a tan-pink, smooth endometrium (0.2 cm in average thickness). The myometrium is pink-white and trabecular (average thickness 1.8 cm). There are three intermural, well-circumscribed nodules (ranging from 0.8-3.7 cm in greatest dimension). On sectioning, the cut surface of the nodules is tan-white and whorling, with no areas of necrosis, hemorrhage, calcification, or cystic degeneration noted.
The right ovary is tan-white and cerebriform. Sectioning reveals a tan-pink, dense stroma with a single smooth- walled simple cyst (1.1 cm in greatest dimension). The right fallopian tube is pink-purple, smooth, and patent, with no lesions identified. The left ovary is tan-white and cerebriform. Sectioning reveals a tan-pink, dense stroma with no lesions identified. The left fallopian tube is pink-purple, smooth, and patent, with no lesions identified. Representative sections are submitted for microscopic evaluation.
Micro A1: Anterior cervix, one fragment.
Micro A2: Posterior cervix, one fragment.
Micro A3: Anterior lower uterine segment, one fragment.
Micro A4: Posterior lower uterine segment, one fragment.
Micro A5: Anterior endomyometrium with serosa, one fragment.
Micro A6: Posterior endomyometrium with serosa, one fragment.
Micro A7-A9: Intermural nodules, 2 fragments each.
Micro A10: Right ovary, including cyst, 2 fragments.
Micro A11: Right fimbriae entirely submitted with cross sections of fallopian tube, 6 fragments.
Micro A12: Left ovary, 2 fragments.
Micro A13: Left fimbriae entirely submitted with cross sections of fallopian tube, 6 fragments.
Weigh the specimen. Orient the specimen as to anterior and posterior walls.
Examine the serosal surface for adhesions, endometriosis, tumor implants, or inflammation and describe.
Find the hysterotomy location (low transverse, low verticle, “classical” = fundal and vertical) and record whether or not it is sutured.
Record the overall dimensions of the uterus (three dimensions), tubes (length and diameter), and ovaries (three dimensions).
If the cervix is present, record the dimensions of the exocervix (two dimensions) and the diameter and shape (round or slit-like) of the external os. If not, record the two dimensions of the cervical margin and the length of the cervical canal present in the specimen. The distal cervical margin is inked. Describe the appearance (smooth, white, glistening) and any lesions of the cervix (ulcerated, irregular, granular).
Photographs of all surfaces of the intact specimen are helpful.
Open the uterus along the lateral margins from the external os to the cornu with scissors. Never use a scalpel. It is useful to use a probe within the os to guide the scissors. Make transverse (horizontal) incisions through the entire mucosa to, but not through, the serosa. Do not abrade the mucosa or wash with water. If cleaning is needed, use sterile saline.
Describe the endometrial cavity and lining including size (cornu to cornu, fundus to endocervical canal), distortion (by leiomyomas), color (tan, hemorrhagic), thickness, and any lesions. If lesions are present describe location (anterior or posterior wall), size, color, consistency, and depth of penetration into myometrium.
Examine the lining for the placental implantation site and any retained placenta or membranes.
Describe the endocervix including size (length and width), color, normal herringbone pattern, and any lesions.
Describe the myometrium for normal trabeculated pattern or adenomyosis (coarse trabeculations or cystic hemorrhagic areas). Describe the thickness of the wall at the area of implantation (including placental thickness and remaining myometrial thickness), as well as the thickness of the normal uninvolved myometrium. If leiomyomas are present describe number, size (or range in size if many), location (subserosal, mural, submucosal, anterior or posterior), color, presence of hemorrhage or necrosis, or calcification, or variation in pattern.
Photograph the opened specimen and cross sections.
Fix in formalin overnight. Take sections the following day of the implantation site (4 to 6 blocks, including 2 blocks of deepest exent with serosal surface), cervix (one section anterior and one section posterior), or cervical canal and cervical resection margin (if the hysterectomy is supracervical), normal endomyometrium (one section anterior and one section posterior), and any other gross findings. More sections of implantation site may be necessary in complex cases. If the placenta is included, process as described in the section on placentas.
The specimen is received fresh labeled with the patient’s name, medical record number,and “gravid uterus with fallopian tubes,” and consists of a (810.0 g) hysterectomy specimen (25.5 × 21.0 × 7.5 cm) with bilateral fimbriated fallopian tubes (right; 15.5 cm in length, 0.9 cm in diameter, left; 15.2 cm in length, 1.0 cm in diameter). The serosal surface is tan-pink, smooth and glistening, with a fundic hysterotomy site (6.0 cm in length), closed with tan surgical sutures. The exocervix (4.5 × 3.8 cm) is pink-white, smooth and glistening, with a slit-like os (1.5 cm in length). The anterior paracervical tissue is inked blue and the posterior inked black. The endocervical canal (4.0 cm in length) is tan-pink and glistening, with a herringbone mucosa. The endometrial cavity (15.3 cm cornu to cornu x 20.5 in length) is lined by a tan-pink, shaggy endometrium (0.3 cm in average thickness). There is an adherent placenta (19.0 × 14.5 × 2.3 cm) implanted on the posterior wall of the cavity at the fundus, 2.5 cm from the previously noted hysterotomy site. The umbilical cord is gray-white (7.5 cm in length, 1.5 cm in diameter) with a normal insertion and left cord twist. The membranes are red-tan and translucent, inserting 100% marginally. On sectioning, the area of greatest extent of placental implantation displays placenta 2.3 cm in thickness, with myometrium 1.0 cm in thickness. The myometrium is pink-white and trabecular (average uninvolved thickness measuring 1.8 cm). The surface of the fallopian tubes is red-purple, smooth, and congested. Both fallopian tubes are grossly patent. There are no ovaries included. Gross photographs are taken. Representative sections are submitted for microscopic evaluation.
Micro A1: Anterior cervix, one fragment.
Micro A2: Posterior cervix, one fragment.
Micro A3: Anterior lower uterine segment, one fragment.
Micro A4: Posterior lower uterine segment, one fragment.
Micro A5-A8: Posterior wall placental implantation, with deepest extent in A5-A6, one fragment each.
Micro A9: Anterior uninvolved endomyometrium plus serosa, one fragment.
Micro A10: Posterior uninvolved endomyometrium plus serosa, one fragment.
Micro A11: Umbilical cord and membrane roll, 3 fragments.
Micro A12: Right fallopian tube fimbriae entirely submitted with cross sections of fallopian tube, 6 fragments.
Micro A13: Left fallopian tube fimbriae entirely submitted with cross sections of fallopian tube, 6 fragments.
Micro A14: Hysterotomy site, one fragment.
( Fig. 19.2 )
Weigh the specimen. Orient the specimen according to anterior and posterior walls. State whether the specimen is received intact or was previously opened.
Examine the serosal surface carefully for adhesions, serosal implants, or direct invasion by tumor. The vaginal reflection at the cervix should be examined for tumor implants.
Ink the parametrial surgical resection margin (disrupted areas). Ink the vaginal/cervical margin in blue for anterior and black for posterior.
Intact grossly normal serosal surfaces need not be inked. Do not ink surfaces exposed by cutting into the specimen.
If the serosal surface is abnormal (e.g., tumor has penetrated to through the uterine wall) this area may be inked to help confirm serosal involvement.
Open the uterus with scissors along the lateral margins from external os to cornu. Avoid cutting through areas suspicious for involvement by tumor. Also avoid opening the uterus by inserting forceps into the cavity and slicing with a blade through the middle of the forceps. This practice is advocated by some, but it can disrupt the tumor and introduce artifacts into the uterine wall (gaps, dislodged tumor into vessels, etc). A single clean cut when opening the uterus is helpful so that the true surgical margins and the serosal surface will be apparent. Do not abrade the mucosa by touching or rinsing with water. If cleaning is needed, use sterile saline.
Make serial transverse (horizontal) incisions from the mucosal surface to, but not through, the serosal surface at approximately 0.5 cm intervals. It is helpful to use a large blade in order to make clean cuts (i.e., not scissors or a scalpel). Leave all tissues attached to maintain orientation.
Describe the endometrial cavity including any irregularities or piling up of the mucosal surface, location of lesions (e.g., anterior or posterior wall), the portion of the endometrial surface involved, and gross invasion (depth). Gross invasion is appreciated as an effacement of the normal myometrial texture but may be difficult to appreciate grossly. For mesenchymal tumors, describe the location (mural and/or exophytic) including smooth vs irregular interfaces with normal tissues, and the texture of the tumor, as well as areas of necrosis and hemorrhage.
Give the size of all lesions. Photos are helpful.
Pin on a wax block and fix overnight in formalin. Paper towels (not gauze) should be placed between transverse sections to wick the formalin and ensure adequate fixation.
Sections are taken the following day. Search for all parametrial lymph nodes and note their location. Usually lymph nodes are not present.
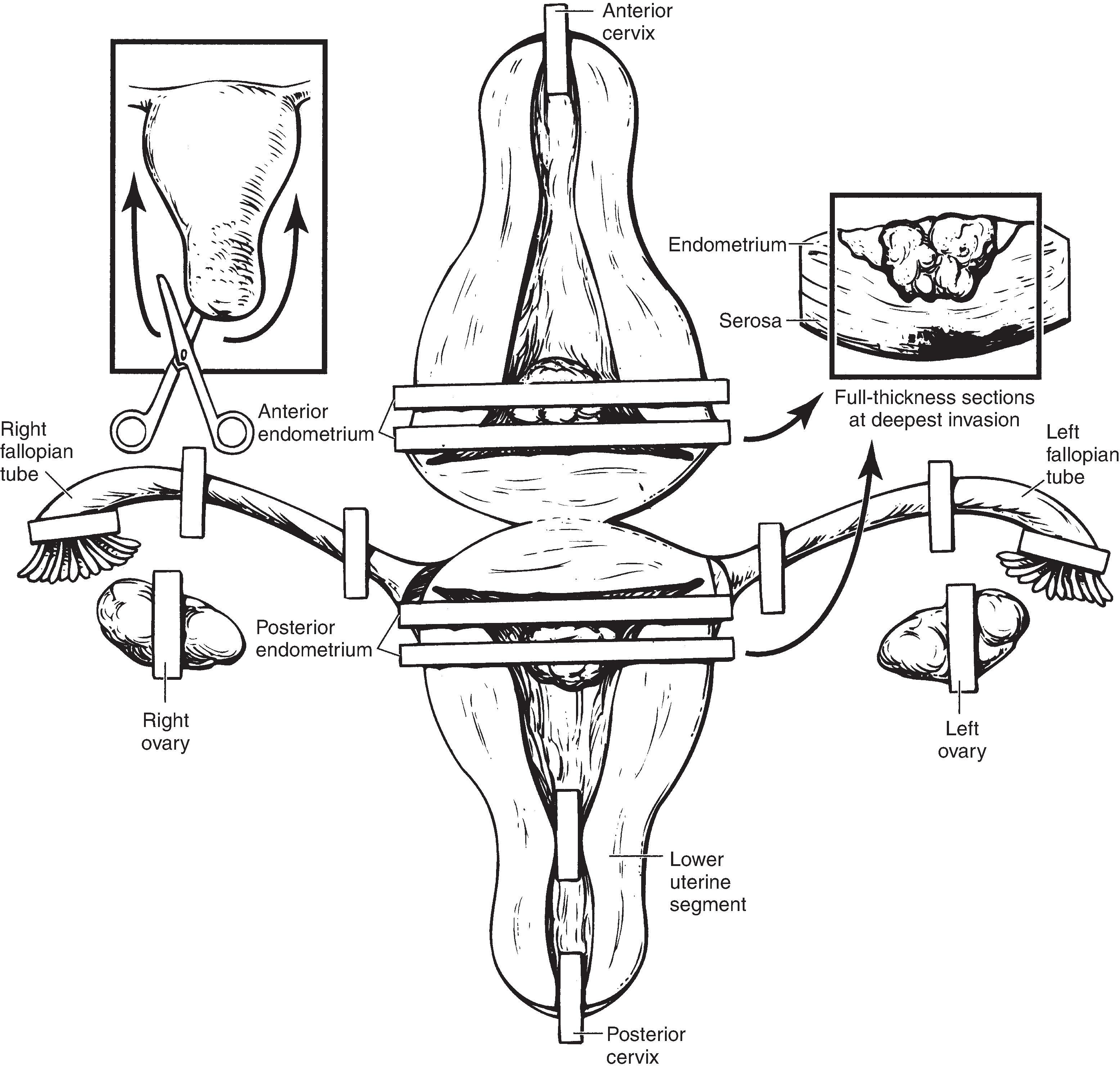
| Tumor | Transmural sections demonstrating depth of invasion to the inked margin. In most cases two anterior and two posterior full thickness sections are adequate. If residual normal endometrial surface is present within the cavity, include it in the sections of tumor. Seeing the normal endomyometrial interface in the section greatly helps in the assessment of myometrial invasion by the tumor. If the tumor is in the LUS or near the cervix, the entire vaginal margin (inked) is divided into clock face quadrants and submitted and extra slides of the LUS and LUS/endocervical junction are also submitted. If no gross lesions are identified, or only EIN is suspected, submit the ENTIRE endometrium including the lower uterine segment. All sections do not need to be full thickness but all should include the endomyometrial interface to assess for invasion. |
| Note: The edges of transmural sections are trimmed to remove areas of myometrium without overlying endometrium ( Fig. 19.2 ). The surrounding normal endometrium should be kept in the specimen. | |
| For mesenchymal tumors (i.e., leiomyosarcomas or endometrial stromal sarcomas), submit one section per cm of tumor. Be sure to include the interface with the surrounding myometrium, as well as endometrium, serosa, cervix, parameterial tissues, and fallopian tubes if the tumor is in close proximity to those structures. Also include the transition between viable tumor and areas of possible necrosis or hemorrhage. | |
| Cervix | Anterior and posterior sections of cervix are taken to include both exo and endocervix and the transformation zone. |
| For endometrial carcinomas that grossly involve the cervix, the cervix should be entirely submitted in a clockwise fashion similar to primary cervical carcinomas in order to evaluate the distance to radial and paracerivcal resection margins. | |
| Lower uterine segment | Two transmural longitudinal sections (one posterior and one anterior). See under “tumor” if the tumor is near the LUS. |
| Fallopian tubes | Submit the entire tube using the SEE-FIM protocol (see under “Fallopian Tube”). The cassettes containing the fimbriae must be indicated in the cassette key. |
| Ovary | Submit the entire ovaries (sections taken transverse to the longitudinal axis) including capsule and adnexal soft tissue. |
| Serosa | If serosa is not included in the sections of endometrium, submit a separate section. |
| Parametrium | Submit any parametrial nodules or lymph nodes. If involved by tumor, submit margin sections. |
| Other lesions | Submit sections of any other lesions (e.g., polyps, leiomyomata). |
Received fresh labeled with the patient’s name, medical record number, and “uterus, cervix, fallopian tube and ovaries,” is a (140.5 g) hysterectomy specimen including uterus (8.7 × 6.0 × 4.3 cm), bilateral ovaries (right: 3.5 × 2.1 × 1.6 cm, left: 3.2 × 2.0 × 1.5 cm), and bilateral fimbriated fallopian tubes (right: 10.5 cm in length x 0.6 cm in diameter, left: 11.8 cm in length x 0.5 cm in diameter). The serosal surface is tan-pink, smooth and glistening, with no areas of disruptions or adhesions noted. The exocervix (4.0 × 3.8 cm) is pink-white, smooth and glistening, with a slit-like/patent os (2.0 cm in length). The anterior paracervical tissue is inked blue and the posterior inked black. The endocervical canal (3.5 cm in length) is tan and glistening, with a herringbone mucosa. The endometrial cavity (3.1 cm cornu to cornu x 5.1 cm in length) is lined by a tan-pink, shaggy endometrium (0.3 cm in average thickness). There is a focal area of tan-white, friable mass within the fundus along the posterior wall (2.3 × 2.0 × 0.7 cm). On sectioning, the mass extends 0.5 cm into the myometrium, 1.5 cm from the posterior serosal surface and 5.0 cm from the cervical os. The myometrium is pink-white and trabecular (average thickness 2.0 cm).
The right ovary is tan-white and cerebriform. Sectioning reveals a tan-pink, dense stroma with no lesions identified. The right fallopian tube is pink-purple, smooth and glistening. The right fallopian tube is not grossly patent, with a portion of tube absent from a prior tubal ligation. The left ovary is tan-white and cerebriform. Sectioning reveals a tan-pink, dense stroma with no lesions identified. The left fallopian tube is pink-purple, smooth, and glistening. The left fallopian tube is not grossly patent, with a portion of the tube absent from a prior tubal ligation.
Gross photographs are taken. The adnexal structures are entirely submitted with representative sections of uterus submitted for microscopic evaluation.
Micro A1: Anterior cervix, one fragment.
Micro A2: Posterior cervix, one fragment.
Micro A3: Anterior lower uterine segment, one fragment.
Micro A4: Posterior lower uterine segment, one fragment.
Micro A5-A6: Anterior endomyometrium with serosa, one fragment each.
Micro A7-A8: Posterior endomyometrium with serosa, including posterior fundic mass, with deepest extent in A8, one fragment each.
Micro A9-A10: Right ovary, entirely submitted, multiple fragments.
Micro A11: Right fimbriae, entirely submitted, 5 fragments.
Micro A12-A14: Right fallopian tube, entirely submitted, multiple fragments.
Micro A15: Right paraovarian soft tissue, entirely submitted, two fragments.
Micro A16-A17: Left ovary, entirely submitted, multiple fragments.
Micro A18: Left fimbriae, entirely submitted, 5 fragments.
Micro A19-A21: Left fallopian tube, entirely submitted, multiple fragments.
Micro A22: Left paraovarian soft tissue, two fragments.
( Fig. 19.3 )
Weigh the specimen. Orient the specimen according to anterior and posterior walls. State whether the specimen is received intact or was previously opened
Examine the serosal surface for adhesions, serosal tumor nodules, or direct invasion by tumor.
Ink the parametrial and cervical resection margins (disrupted areas) and the vaginal cuff margin.
Intact grossly normal serosal surfaces need not be inked. If desired, the anterior and posterior serosal surfaces may be inked in two different colors for orientation.
Do not spill ink onto the exocervix. Do not ink surfaces exposed by cutting into the specimen. The parametrial tissues should be measured in three dimensions and then amputed from the cervix (leaving a small amount attached to the wall). If there is tumor grossly extending into the parametrial tissues (by inspection or palpation), leave the inked parametrial tissue attached.
Amputate the cervix with the vaginal cuff. Open at the anterior surface (12:00). If lesions are present, describe them and measure them in the fresh state (prior to fixation and pinning). Each lesion should described as to clock face position, dimensions (length – parallel to canal, radial – perpendicular to canal, and thickness) and appearance (exophytic, flat, or ulcerated). Pin the cervix onto a wax board and fix in formalin overnight. This allows for maximum exposure to the mucosa to the fixative and makes serial sectioning of the cervix easier. Once fixed, slice the cervix parallel to the canal in a clockwise fashion at 0.5 cm intervals.
Open the uterine corpus with scissors along the lateral margins from external os to cornu. Avoid cutting through areas suspicious for involvement by tumor and avoid introducting a forceps into the cavity to open the specimen (see previous section). A single clean cut when opening the uterus is helpful so that the true surgical margins and the serosal surface will be apparent. Do not abrade the mucosa by touching or rinse with water. If cleaning in necessary, use sterile saline.
Make serial transverse incisions from the mucosal surface to, but not through, the serosal surface at approximately 0.5 cm intervals. It is helpful to use a large blade in order to make clean cuts (i.e., not scissors or a scalpel). Leave all tissues attached in order to maintain orientation.
Describe as for a nontumor hysterectomy but include location of lesions (e.g., exocervix vs endocervix, vs LUS, clock position), tumor dimensions as described above, and distance from margins. Fix overnight in formalin.
Carefully search for parametrial lymph nodes and note their location, side, and number. Lymph nodes are frequently received from the surgeons as separate specimens. If the parametrium is grossly involved by tumor, or such is suspected, keep the parametrium attached to be incorporated in the histologic sections of the cervix.
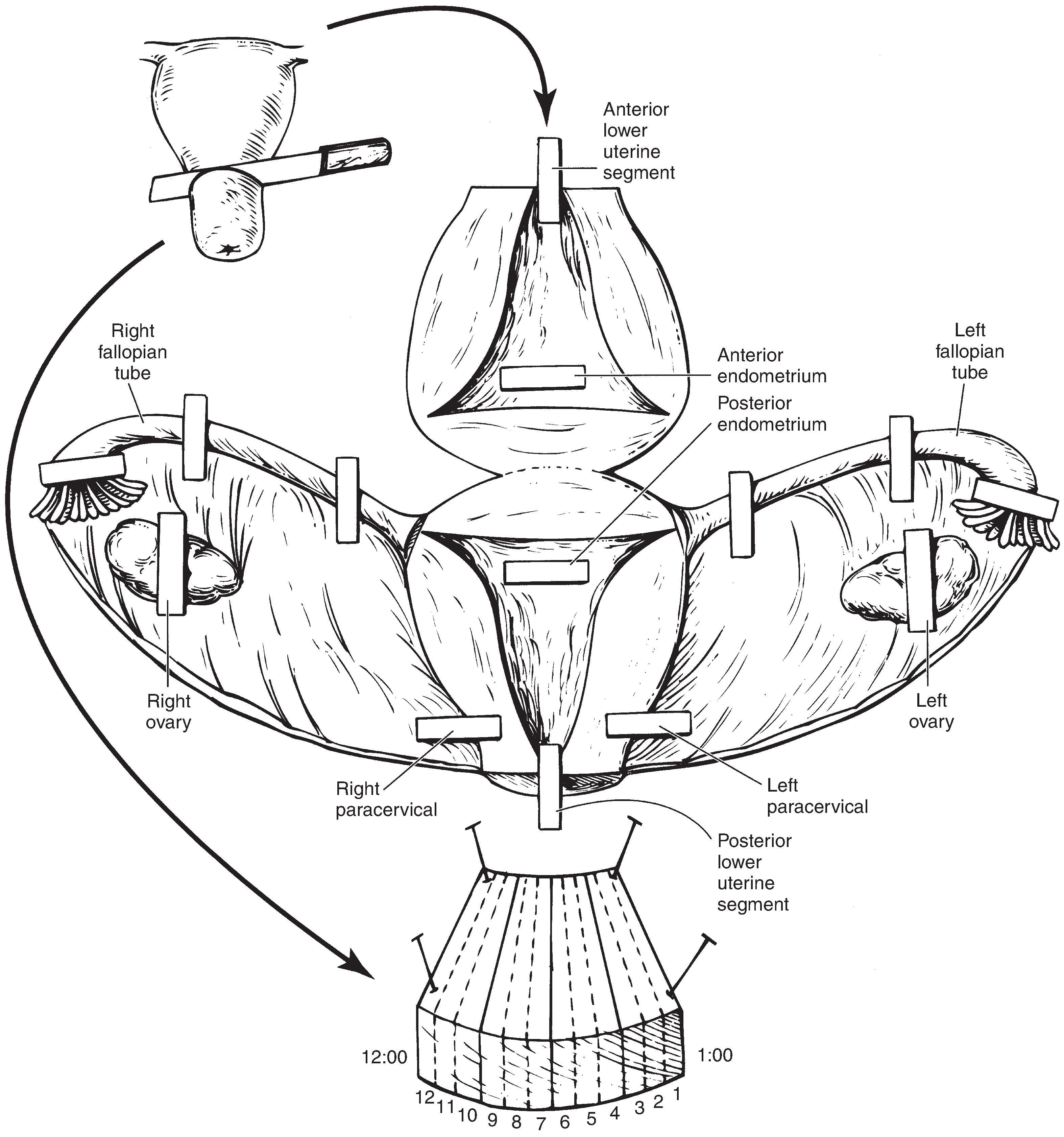
| Tumor (cervix) | If there is no visible tumor, or the tumor measures 2 cm or less, submit the entire cervix by clock positions (as described for cone biopsies – see below). The vaginal margin can be left on the cervix and included with these sections if small. If this margin is large, representative sections of vaginal cuff can be submitted using clock positions. If tumor is close or involves the vaginal margin, the entire margin should be submitted as clock positions. If the cervix is too long for the slices to fit in a single block, consider composite sections (bisect each slice and submit as proximal and distal halves). |
| If the tumor is >2 cm in size, representative sections of 1 section per cm can be submitted. Sections should include the deepest point of invasion, the greatest tumor thickness, and the relationship to all margins. | |
| If the tumor extends beyond the cervix into the parametria, uterine corpus, or serosa, sample these areas by showing contiguity between the tumor and the involved structure, as well as the inked margins. | |
| Lower uterine segment | Two transmural sections (one posterior and one anterior). See under “tumor” if the tumor is near the LUS. |
| Endometrium | Two full thickness sections (one anterior and one posterior). |
| Fallopian tubes | At a minimum, submit the entire fimbriae and a representative cross section of the tube. The cassettes containing the fimbriae must be clearly indicated in the cassette key. |
| Ovary | Submit at least 2 representative sections from each grossly normal ovary (taken transverse to the longitudinal axis) including capsule. |
| Serosa | If serosa is not included in the sections of endometrium, submit a separate section. |
| Parametrium | Submit any parametrial nodules or lymph nodes. Note number, location, and side. The parametrial tissues should be submitted entirely for histologic examination (they may be included as full thickness sections of the cervix). |
| Other lesions | Submit sections of any other lesions (e.g., polyps, leiomyomata). |
Received fresh labeled with the patient’s name, medical record number, and “Radical hysterectomy,” is an intact (120.5 g) hysterectomy specimen including uterus (7.8 × 5.6 × 4.0 cm), bilateral ovaries (right: 3.0 × 1.3 × 0.7 cm, left: 2.8 × 1.3 × 1.7 cm), and bilateral fimbriated fallopian tubes (right: 12.8 cm in length x 0.4 cm in diameter, left: 11.5 cm in length x 0.4 cm in diameter). The serosal surface is tan-pink, smooth and glistening, with no areas of fibrous adhesions noted. The cervix has attached vaginal cuff (2.2 cm in length, 3.0 cm in diameter). The anterior paracervical tissue is inked blue, the posterior paracervical tissue is inked black, and the parametrial margin is inked orange. The exocervix (3.5 × 3.5 cm) is pink-white with a circular os (0.6 cm in diameter). There is a focal tan-white, firm, centrally ulcerated mass (1.3 × 1.2 × 0.5 cm) along the posterior exocervix, within 0.8 cm of the edge of the exocervix at 6:00. On sectioning, the mass extends to a depth of 0.5 cm, involving the endocervical canal but not the lower uterine segment. The mass is 2.5 cm from the nearest posterior vaginal cuff margin (6:00) and 0.9 cm from the inked posterior paracervical margin. The remaining endocervical canal (3.0 cm in length) is tan and glistening, with a herringbone mucosa. The endometrial cavity (2.8 cm cornu to cornu x 4.2 cm in length) is lined by a tan-pink, smooth endometrium (0.1 cm in average thickness). The myometrium is pink-white and trabecular (average thickness 2.0 cm). There is a single well-circumscribed intermural nodule (1.5 cm in greatest dimension). On sectioning, the cut surface of the nodule is tan-white and whorling, with no areas of hemorrhage, necrosis, calcification, or cystic degeneration noted.
The right ovary is tan-white and smooth/cerebriform. Sectioning reveals a tan-pink, dense stroma with no lesions identified. The right fallopian tube is pink-purple, smooth, and patent, with no lesions identified. The left ovary is tan-white and cerebriform. Sectioning reveals a tan-pink, dense stroma with no lesions identified. The left fallopian tube is pink-purple, smooth, and patent, with no lesions identified. There is one pink-tan candidate lymph node located in the right parametrial soft tissue (0.8 cm in greatest dimension). There are two candidate lymph nodes located in the left parametrial soft tissue (both 0.5 cm in greatest dimension).
Gross photographs are taken. Representative sections are submitted for microscopic evaluation.
Micro A1-A3: Cervix from 12:00-3:00, entirely submitted, one fragment each.
Micro A4-A6: Cervix from 3:00-6:00, with mass in A6, entirely submitted, one fragment each.
Micro A7-A9: Cervix from 6:00-9:00, with mass in A7-A8, entirely submitted, one fragment each.
Micro A10-A12: Cervix from 9:00-12:00, entirely submitted, one fragment each.
Micro A13: Vaginal cuff margin 12:00, one fragment.
Micro A14: Vaginal cuff margin 3:00, one fragment.
Micro A15: Vaginal cuff margin 6:00, one fragment.
Micro A16: Vaginal cuff margin 9:00, one fragment.
Micro A17: Anterior lower uterine segment, one fragment.
Micro A18: Posterior lower uterine segment, nearest to mass, one fragment.
Micro A19: Anterior endomyometrium plus serosa, one fragment.
Micro A20: Posterior endomyometrium plus serosa, one fragment.
Micro A21: Intermural nodule, 2 fragments.
Micro A22: Right ovary, 2 fragments.
Micro A23: Right fimbriae entirely submitted with cross sections of fallopian tube, 6 fragments.
Micro A24: Left ovary, 2 fragments.
Micro A25: Left fimbriae entirely submitted with cross sections of fallopian tube, 6 fragments.
Micro A26: Right parametrium, one fragment.
Micro A27: Left parametrium, one fragment.
Micro A28: Right parametrial lymph node bisected, 2 fragments.
Micro A29: Left parametrial lymph nodes, differentially inked blue and black and bisected, 4 fragments.
Essure® devices are coils placed in the fallopian tubes via a catheter introduced into the vagina. The coils cause fibrosis resulting in blockage of the tubes. It is a nonsurgical alternative to tubal ligation. The coils measure approximately 3 cm x 0.4 cm. There is a tightly wound stainless steel inner coil and a more loosely wound outer nickel and titanium alloy coil.
The Food and Drug Association (FDA) approved the device in 2002. However, when complications including tubal perforation, bleeding, and failure to prevent pregnancy were reported, the FDA decided to restrict its use in 2018 ( https://www.fda.gov/medical-devices/essure-permanent-birth-control/fda-activities-related-essure - accessed July 23, 2021). The manufacturer halted sales in December of 2018.
Some women choose to have the devices removed. Before processing a specimen, it is important to determine if the procedure was specifically for removal of the Essure® coils. If so, the specimen may become part of a medicolegal proceeding and should be handled as a possible legal case.
In addition to standard processing procedures, the following procedures should be followed:
Weigh the specimen. Orient the specimen as to anterior and posterior. Take external measurements, per routine guidelines.
Photograph specimen anterior, posterior, and lateral views. Carefully examine for areas of serosal/tubal disruption and photograph as necessary.
Take specimen radiographs of anterior and posterior aspects.
Open the uterus along the lateral margins with scissors, per routine guidelines. Be careful on approach to uterine cornu.
Take a radiograph and gross photograph of the right and left cornu of the open specimen. Pin the specimen flat and allow to adequately fix in formalin.
After proper fixation, make a single longitudinal cut through the wall of each fallopian tube parallel to the plane of the Essure® device. Carefully retract the wall of the fallopian tube to expose the position of the device in relation to the fallopian tube lumen.
Take additional photographs and radiographs of exposed devices.
Measure the device length. Measure the distance of the device to the cornu and fimbriae. Provide documentation if the device is protruding into the endometrial cavity or through the fallopian tube wall and give the distance of the protrusion.
Note if the device is well-adhesed with dense fibrous tissue to the fallopian tubes. Note any signs of purulence, hemorrhage or infection.
Remove the Essure® coil intact if possible. These devices consist of a tightly wound inner coil and a more loosely wound outer coil. The end of the inner coil can be cut with scissors and then pulled out of the lumen from the other end. The outer coil fragments more easily. Remove the coils and place in a biopsy bag within a cassette with the case for safe keeping. All tissue submitted for histology should be free of metal fragments. Radiography can be used to check for remaining fragments.
These cases often are requested by the patient and needed for medico-legal reasons. If the patient requests for the specimen to be returned, mark the specimen container to make sure it is not discarded.
Serially section the fallopian tube perpendicular to the long axis and entirely submit the portion of the tube where the Essure® device was located.
Entirely submit the distal third of each fallopian tube, including fimbriae. Representatively submit cross- sections of the remainder of the mid and distal tube.
Submit sections of hysterectomy, per routine guidelines.
Received fresh labeled with the patient’s name, medical record number, and “Uterus and cervix,” is a (210.0 g) hysterectomy specimen (10.5 × 5.6 × 3.5 cm) with bilateral fimbriated fallopian tubes (right; 8.5 cm in length and 0.5 cm in diameter, left; 8.8 cm in length and 0.6 cm in diameter). The serosal surface is tan-pink, smooth and glistening with a focal area of serosal disruption and adhesion at the proximal base of the left fallopian tube (0.8 × 0.5 cm). The exocervix (3.2 × 3.2 cm) is pink-white, smooth and glistening, with a slit like os (1.2 cm in length). The anterior paracervical tissue is inked blue and the posterior inked black. The endocervical canal (3.1 cm in length) is tan-pink and glistening, with a herringbone mucosa. The endometrial cavity (2.8 cm cornu to cornu x 4.3 cm in length) is lined by a tan-pink endometrium (0.2 cm in average thickness). The myometrium is pink-white and unremarkable (average thickness measuring 1.8 cm). On opening of the fallopian tubes, there are metallic silver Essure® devices (each measuring 3.0 cm in length, 0.4 cm in diameter). The Essure® device within the right fallopian tube extends within 0.5 cm of the right cornu and 6.5 cm from the right fimbria. The Essure® device in the left fallopian tube extends within 1.0 cm of the left cornu through the fallopian tube wall, within the area of focal disruption previously noted within the serosa of the base of the left fallopian tube, and 6.8 cm from the left fimbria. Both fallopian tubes display dense fibrous tissue surrounding the areas of Essure® devices. No areas of purulence are noted. Gross photographs and radiographs are taken. Ovaries are not present.
Representative sections are submitted for microscopic evaluation.
Micro A1: Endometrium of dome, proximal to right coil, 3 fragments.
Micro A2: Right fallopian tube just proximal to coil, multiple fragments.
Micro A3: Right fallopian tube encasing coil, multiple fragments.
Micro A4: Right fallopian tube just distal to coil, multiple fragments.
Micro A5: Endometrium of dome, proximal to left coil, 3 fragments.
Micro A6: Left fallopian tube just proximal to coil, multiple fragments.
Micro A7: Left fallopian tube encasing coil, multiple fragments.
Micro A8: Left fallopian tube just distal to coil, multiple fragments.
Micro A9: Dome of uterus between the two coils, multiple fragments.
Micro A10: Anterior cervix, one fragment.
Micro A11: Posterior cervix, one fragment.
Micro A12: Anterior lower uterine segment, one fragment.
Micro A13: Posterior lower uterine segment, one fragment.
Micro A14: Anterior endomyometrium plus serosa, one fragment.
Micro A15: Posterior endomyometrium plus serosa, one fragment.
Micro A16: Right fallopian tube fimbriae entirely submitted, multiple fragments.
Micro A17: Mid right fallopian tube, multiple fragments.
Micro A18: Left fallopian tube fimbriae entirely submitted, multiple fragments.
Micro A19: Mid left fallopian tube, multiple fragments.
Leiomyomas: These tumors are firm whorled white to tan nodules present within myometrium, bulging into the endometrial lumen or protruding into the peritoneal cavity. Cystic degeneration and softening may be seen in the center of large leiomyomas. Hemorrhage and necrosis should not be seen (unless secondary to ischemic change).
Subserosal: immediately below the serosa, some are pedunculated and can appear to be peri-uterine masses
Intramural: within the myometrium
Submucosal: immediately below the endometrium
Leiomyosarcoma: Only 1 to 3 women out of 1,000 with a preoperative diagnosis of leiomyoma will prove to have a sarcoma. Most of these women are > 40 years old. The risk is increased if there is a history of a mass increasing in size. A leiomyosarcoma is usually the dominant lesion (or is often solitary) and is usually larger (> 10 cm) and softer than leiomyomas. The color may be gray/yellow rather than white. Areas of hemorrhage and necrosis (green) may be present. Invasion into the surrounding myometrium may be present. However some are grossly indistinguishable from leiomyomas and are circumscribed. Malignant lesions generally have complex karyotypes as compared to leiomyomas.
Stromal nodules/sarcomas: May be well circumscribed (nodules) or diffusely infiltrative (sarcomas). Lymphovascular invasion can often be seen as “worm like” masses within the myometrium or parametrium. About one third will invade into adjacent tissues. Necrosis and hemorrhage may be present in sarcomas.
Adenomyosis: Due to benign glands embedded within myometrium. The myometrium appears thickened with coarse trabeculations. Pinpoint hemorrhage may be present.
Endometrial polyps: Usually large broad based finger-like projections from the endometrial wall. The center is comprised of fibrous stroma and the surface is covered by endometrium.
Endometrial carcinoma: The endometrial lining may be heaped up but a red/tan friable appearance is more characteristic of carcinomas. The lesion may be best appreciated on cross section. Invasive carcinomas may efface the normal myometrial texture. Stromal invasion may be subtle or obscured by adenomyosis.
Malignant mixed mullerian tumor (carcinosarcoma): Usually a very large friable mass completely filling the endometrial cavity and extending through the cervical os. The myometrium is typically deeply invaded. Foci of bone or cartilage may be present.
Adenomatoid tumor: These tumors form a poorly circumscribed, soft to firm, gray, white or yellow mass within the myometrium, which may grossly mimic a leiomyoma. The majority are subserosal. Large tumors may extend into the endometrium.
Gestational trophoblastic tumors: Complete or partial hydatidiform moles are usually received as products of conception and are grossly recognized by the numerous dilated grape-like clear vesicles. Fetal parts may be present in partial hydatidiform moles. The tumor has the appearance of a hemorrhagic mass adherent to the wall of the uterus.
Gestational choriocarcinoma: These tumors arise from placental tissues from either a normal or abnormal pregnancy. It is a soft fleshy yellow white tumor, often with large areas of necrosis, and usually with extensive hemorrhage. The tumor invades into the myometrium and may extend out into the serosa. There is a separate AJCC staging system for these tumors.
Pathologic Diagnostic/Prognostic Features Sign-out Checklist for Endometrial Carcinomas
| Procedure(s) | Hysterectomy (radial, simple, supracervical), oophorectomy (right, left), salpingectomy (right, left), vaginal cuff resection, omentectomy, peritoneal biopsies, pelvic exenteration |
| Hysterectomy Type | Abdominal, vaginal (with or without laparoscopic-assistance or robotic assistance) |
| Lymph Node Sampling | Pelvic lymph nodes, para-aortic lymph nodes, sentinel lymph nodes |
| Specimen Integrity | Intact hysterectomy specimen (unopened or opened), morcellated |
| Tumor Site | Endometrium (anterior, posterior), fundus, lower uterine segment, endometrial polyp |
| Tumor Size | Greatest dimension (2 additional dimensions may be given) |
| Extent of surface area involved (< 4 cm versus > 4 cm) is correlated with higher stage disease. | |
| Histologic Type | Endometrioid carcinoma (and subtypes), mucinous adenocarcinoma, serous adenocarcinoma, clear cell adenocarcinoma, squamous cell carcinoma, undifferentiated carcinoma, other rare types. The WHO Classification is recommended. |
| Histologic Grade | Grade if applicable for tumor type |
| Myometrial Invasion | Report as depth of invasion and as percentage of myometrium involved (important cutoff is < 50% or ≥ 50%), myometrial thickness |
| Adenomyosis | Not present, present and not involved by carcinoma, present and involved by carcinoma |
| Uterine Serosa | Not involved by carcinoma, involved by carcinoma |
| Lower Uterine Segment | Not involved by carcinoma, involved by carcinoma (superficial and not invasive or myoinvasive) |
| Cervical Stroma | Not involved, invasion of cervix without stromal invasion, invasion of cervix with invasion |
| Extent of Involvement Other Organs | Involvement of fallopian tube (right or left), ovary (right or left), vagina, peritoneum, parametrium (right or left), omentum, bladder wall, bladder mucosa, colon or rectal wall, bowel mucosa, pelvic wall |
| Peritoneal Ascitic Fluid | Negative for malignancy, atypical or suspicious, malignant, nondiagnostic |
| Ectocervical/Vaginal Cuff Margin | Uninvolved by carcinoma (distance from carcinoma), involved by carcinoma |
| Parametrial/Paracervical Margin | Uninvolved by carcinoma (distance from carcinoma), involved by carcinoma |
| Lymphovascular Invasion | Not identified, present – focal, present - substantial |
| Regional Lymph Nodes | Number of nodes examined, number involved, location (right or left; pelvic or para-aortic), size of metastases (macrometastasis, micrometastasis, isolated tumor cells) |
| Additional Pathologic Findings | Atypical hyperplasia, endometrial intraepithelial neoplasia (EIN), atrophy, polyps |
| Ancillary Studies | In some cases, estrogen and progesterone studies may be requested. Testing for microsatellite instability or DNA mismatch repair gene products (MSH2, MSH6, PMS2, MLH1) is recommended to be performed in all cases of endometrial adenocarcinoma to screen for Lynch syndrome (hereditary nonpolyposis colon carcinoma or HNPCC). |
| Distant Metastasis | Reported if present. If distant metastasis is not present on pathologic examination, the M category is a clinical classification. |
| AJCC or FIGO Classification | Categories should be provided, when possible ( Table 19.2 , Table 19.3 , Table 19.4 ). |
| Information needed for AJCC and FIGO (8th edition) classification | ||
| Group | Features | Comments |
| T | Extent: confined to the corpus uteri, limited to endometrium with <50% myometrial invasion, invasion with ≥ 50% of myometrium, invasion into stromal connective tissue of the cervix, involvement of serosa, involvement of adnexa, involvement of vagina, involvement of parametrium, invasion into bladder mucosa, invasion into bowel mucosa | Carefully selected perpendicular sections are necessary to evaluate the depth of invasion. |
| N | Metastases present or absent | |
| Size: ≤ 0.02 cm (isolated tumor cells), > 0.02 cm to ≤ 0.2 cm, > 0.2 cm | ||
| Location: pelvic, para-aortic | ||
| M | Distant metastases | Usually determined clinically or with a separate biopsy of a metastatic site. |
| Information needed for AJCC and FIGO (8th edition) classification | ||
| Group | Features | Comments |
| T | Size: ≤ 5 cm, > 5 cm | Gross evaluation is necessary for the determination of tumor size. |
| Extent: limited to the uterus, involves adnexa, involves other pelvic tissues, involves abdominal tissues, involves bladder or rectum | ||
| Focality: one site, more than one site | ||
| N | Metastases present or absent | |
| Size: ≤ 0.02 cm (isolated tumor cells), > 0.02 cm | ||
| Size: isolated tumor cells, ≤ 0.02 cm, > 0.02 cm to ≤ 0.2 cm, | ||
| M | Distant metastases | Usually determined clinically or with a separate biopsy of a metastatic site. |
| Information needed for AJCC and FIGO (8th edition) classification | ||
| Group | Features | Comments |
| T | Extent: limited to the uterus, limited to endometrium/endocervix, invades to <50% of myometrium, invades to ≥ 50% of myometrium, extends beyond the uterus but within the pelvis, involves adnexa, involves other pelvic tissues, involves abdominal tissues, invades bladder or rectum | Carefully selected perpendicular sections are necessary to evaluate the depth of invasion. |
| Focality: one site, more than one site | ||
| N | Metastases present or absent | |
| Size: ≤ 0.02 cm (isolated tumor cells), > 0.02 cm | ||
| Location: pelvic, para-aortic | ||
| M | Distant metastases | Usually determined clinically or with a separate biopsy of a metastatic site. |
This checklist incorporates information from the CAP Cancer Committee protocols for reporting on cancer specimens (see www.cap.org/ ) as well as other resources. The specific details of reporting the elements may vary among institutions.
| Procedure | Dilation and curettage, hysterectomy (simple, supracervical, radical), pelvic exenteration |
| Hysterectomy Type | Abdominal, vaginal (with or without laparoscopic assistance or robotic assistance) |
| Specimen Integrity | Intact, open, morcellated |
| Tumor Site | Uterine corpus, cervix, other |
| Tumor Size | Greatest dimension (two additional dimensions may be given) |
| Important sizes for prognosis are <3 cm, 3 to 5 cm, and >5 cm | |
| Histologic Type | Hydatidiform mole (complete, partial, or invasive), choriocarcinoma, placental site trophoblastic tumor, epithelioid trophoblastic tumor, malignant trophoblastic tumor, type cannot be determined, other |
| Tumor/Organ Involvement | Tumor confined to uterus (pT1), tumor extends outside of uterus but is limited to genital structures (fallopian tube, ovary, vagina, cervix, broad ligament) (pT2), tumor extends to nongenital organs or structures |
| Myometrial invasion: present (% of thickness), absent Serosal surface: involved, not involved | |
| Margins | Uninvolved (distance to closest margin), involved (specify margin) |
| Lympovascular Invasion | Not identified, present |
| Fetal Tissue | Not identified, present (specify type) |
| Fetal Anomalies | Not applicable, cannot be determined, not identified, present (specify type) |
| Additional Pathologic Findings | Implantation site, leiomyoma, adenomyosis |
| AJCC or FIGO Classification | Categories should be provided, when possible. |
| Distant Metastasis | If present (give number and site of metastases). If distant metastasis is not present on pathologic examination, the M category is a clinical classification. |
| AJCC or FIGO Classification | T, N, and M classifications should be provided, when possible ( Table 19.5 ). cM0 is conferred after clinical assessment; there is no pM0 category. |
| Information needed for AJCC and FIGO (8th edition) classification | ||
| Group | Features | Comments |
| T | Extent: confined to uterus, extends to other genital structures (ovary, tube, vagina, broad ligaments) by direct extension or metastasis | |
| N | There is no N category | |
| M | Distant metastases | Usually determined clinically or with a separate biopsy of a metastatic site. |
This checklist incorporates information from the CAP Cancer Committee protocols for reporting on cancer specimens (see www.cap.org/ ) as well as other resources. The specific details of reporting the elements may vary among institutions.
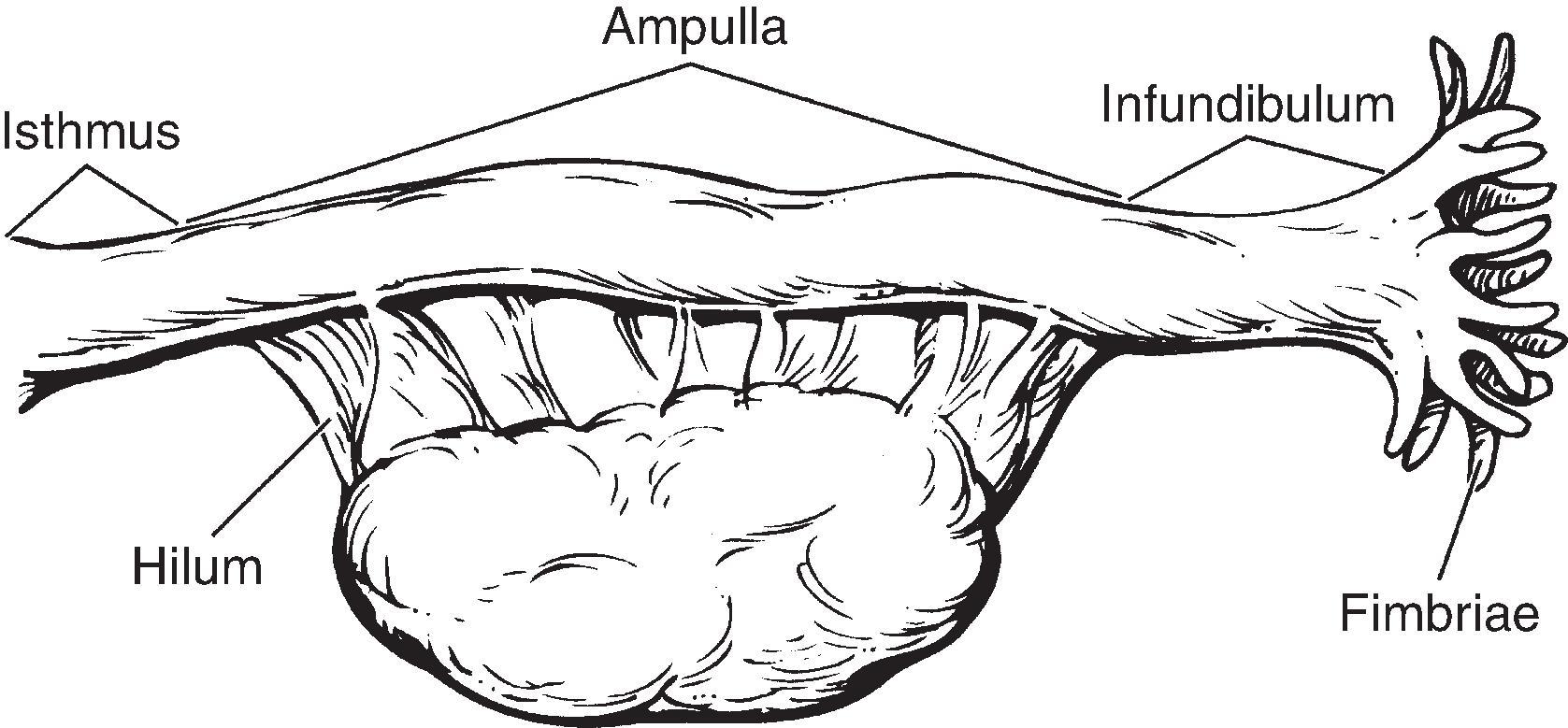
Ovaries are removed for evaluation of a mass, as part of a larger resection, or prophylactically in a patient with a personal or family history of breast cancer, ovarian cancer, or a germline BRCA mutation ( Fig. 19.4 ). Occasionally, biopsies are performed for incidental mass lesions (e.g., a corpus luteum of pregnancy during a Cesarean section) or for treatment (e.g., Stein-Leventhal syndrome).
In addition to age, clinically history is often necessary or helpful for the evaluation of ovarian specimens ( Table 19.6 ).
| HISTORY RELEVANT TO ALL SPECIMENS | HISTORY RELEVANT FOR OVARIAN SPECIMENS |
| Organ/tissue resected or biopsied | Current or recent pregnancy |
| Purpose of the procedure | Abnormal uterine bleeding |
| Gross appearance of the organ/tissue/lesion sampled | Personal or family history or ovarian or breast carcinoma and/or known germline mutation (e.g., BRCA1 or BRCA2 ) |
| Any unusual features of the clinical presentation | History of Stein-Leventhal syndrome |
| Any unusual features of the gross appearance | |
| Prior surgery/biopsies - results | |
| Prior malignancy | |
| Prior treatment (radiation therapy, chemotherapy, drug use that can change the histologic appearance of tissues) | |
| Compromised immune system |
Neoplasms generally have one of the three following appearances:
Simple cyst , thin-walled, without solid areas. Almost always benign. Most are follicular cysts (cystic follicles), corpus luteum cysts, or cystadenomas (epithelial-lined cysts). This is the most common type of cyst.
Complex cyst with or without a solid component. May be nonneoplastic (e.g., an endometriotic or “chocolate” cyst), a benign neoplasm (dermoid), a borderline tumor, or a malignant tumor.
Solid tumors. May be benign fibromas, Brenner tumors, Granulosa cell tumors, or carcinomas.
Record the overall dimensions of the ovary and describe the outer surface including color (white), surface (smooth or convoluted, adhesions, papillary projections), simple cysts (thin-walled without a solid component).
Avoid rubbing or abrading the outer surface in order to preserve the delicate (and very fragile) epithelial lining.
If any abnormality is present (e.g., cysts, papillary projections), ink the outer surface.
Serially section the ovary, parallel to the short axis.
Describe the ovary including color and presence of corpus luteum and corpora albicantia. If cysts are present describe number, size, unilocular vs multilocular, lining (smooth, irregular, papillary projections, velvety as in endometriotic cyst), thickness of wall, contents (fluid vs keratinaceous material and hair as in mature teratoma, serous vs mucinous, hemorrhagic), calcified areas or bone. If it is a large cyst, try to identify remaining ovary as a focal thickening of the wall.
The usual unremarkable ovary with only small simple cysts can be sampled with one section demonstrating any features noted above.
If the ovary was removed as a prophylactic procedure in a woman with a personal or family history of ovarian or breast carcinoma or has a known BRCA mutation, the entire specimen (ovary, fallopian tube, and adnexal soft tissue) is examined histologically. See under “Fallopian Tube” for processing tubes removed for prophylaxis.
Large thin-walled cysts can be rolled into a “jelly roll” and fixed in formalin overnight. Submit transverse sections of the roll. Try to submit a section of the residual ovary. Submit one section per cm.
If there is any suspicion of malignancy (e.g., mucinous cyst, complex cyst, papillary projections, solid areas) additional sections must be taken to document these areas and any extension into adjacent tissues (see below).
Received fresh labeled with the patient’s name, medical record number, and “right ovary,” is a (11.0 g) oophorectomy specimen (3.5 × 1.8 × 0.8 cm). The outer surface of the ovary is tan-white and cerebriform. On sectioning, cut surface displays a single simple cyst (0.6 cm in greatest dimension) filled with yellow serous fluid. The cyst wall is smooth with no papillary excrescences noted. No fallopian tube is included. Representative sections are submitted for microscopic evaluation.
Micro A1: Ovary, including cyst, 2 fragments.
Record the overall dimensions of the ovary and describe the outer surface including color (white), surface (smooth or convoluted, adhesions, papillary projections), simple (thin-walled without a solid component) cysts. Papillations or a “nubby” appearance on the surface of the ovary could indicate either invasion of a tumor through the capsule or a serosal implant.
Avoid rubbing or abrading the outer surface in order to preserve the surface epithelial lining. Small superficial tumors may be present.
Ink the outer surface, including all areas of irregularity.
Ovarian cysts are opened with great care as the cyst fluid may be under pressure. Wear goggles and appropriate personal protective equipment (PPE) when grossing. Open in a pan or on a generous number of surgical drapes to absorb all the fluid. Very large cysts may need to be opened in a sink. Make a small initial incision inferiorly (away from the face of the prosector) to allow the fluid to drain slowly.
Try to identify remaining ovarian tissue. It can sometimes be seen as a thickened portion of the wall readily visible on transillumination. Do not abrade the lining by excessive handling.
Describe the cyst including size, inner surface (smooth or with papillary areas or solid areas, velvety texture as in endometriotic cysts), wall thickness, contents (blood, serous fluid, mucinous fluid, keratinaceous and sebaceous material and hair as in mature teratoma), solid areas (color, texture, extension to serosal surface). If the fallopian tube is included, describe its relationship to the cyst. Describe the remaining ovary including color, corpus luteum, corpora albicantia.
Large thin-walled cysts can be rolled into a “jelly roll” and fixed in formalin overnight. Submit transverse sections of the roll. Sections of the cyst should be one per cm with up to two sections in the same block depending on their size. Indicate which sections contain ovarian surface and if a section includes the transition with the adnexal soft tissue.
If there is any suspicion of malignancy (e.g., mucinous cyst, complex cyst, papillary projections, solid areas) additional sections must be taken to document these areas and any extension into adjacent tissues.
For mucinous cysts, if the cyst is 10 cm or less, one section per cm should be taken, provided that all solid and cystic areas are included. If the mucinous cyst is >10 cm, sampling should be 2 sections per cm of greatest dimension. Malignant features can be focal in this type of neoplasm.
Submit a section of the residual normal ovary and a section with fallopian tube, if present.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here