Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Additional content is available online at Elsevier eBooks for Practicing Clinicians
Additional content is available online at Elsevier eBooks for Practicing Clinicians
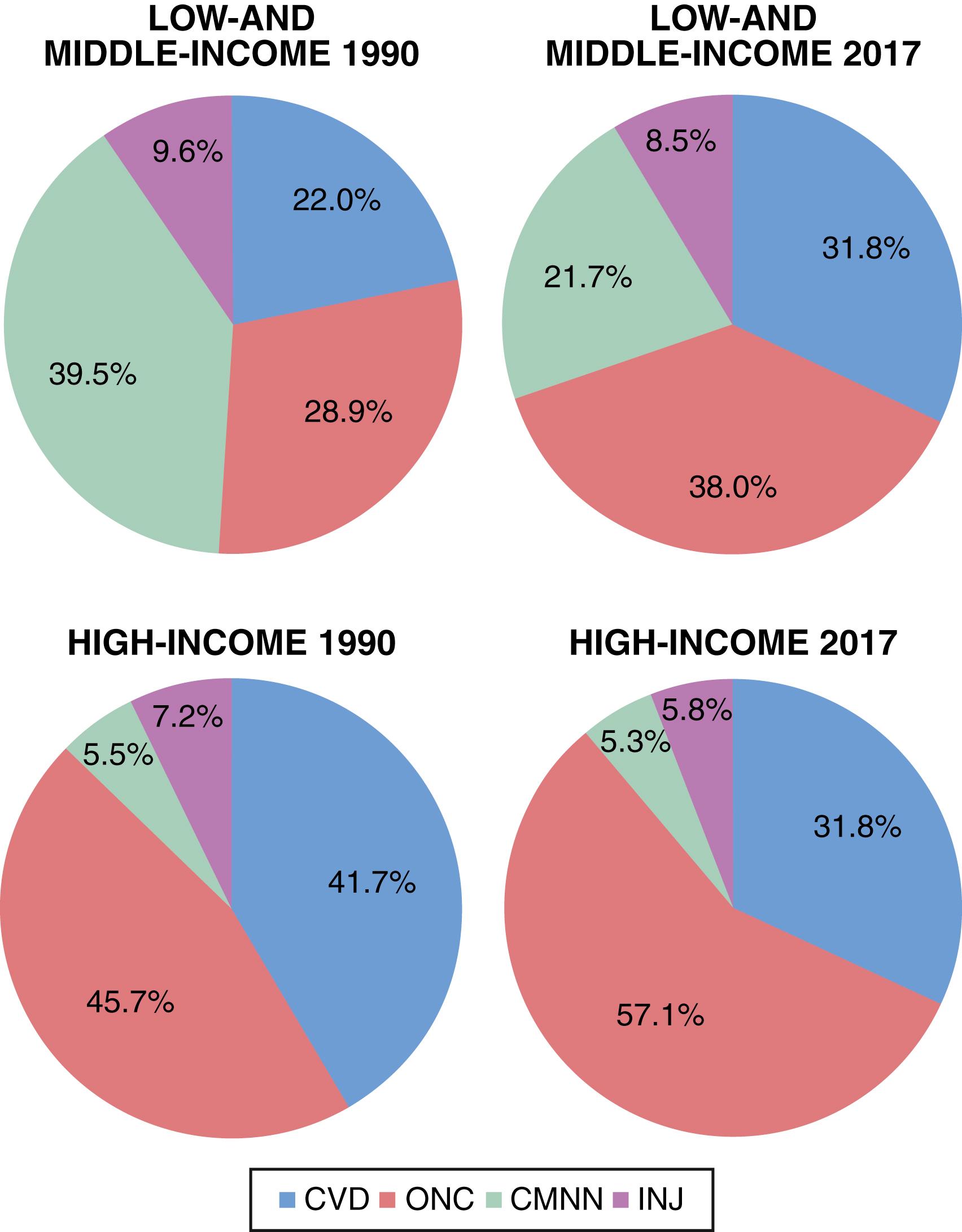
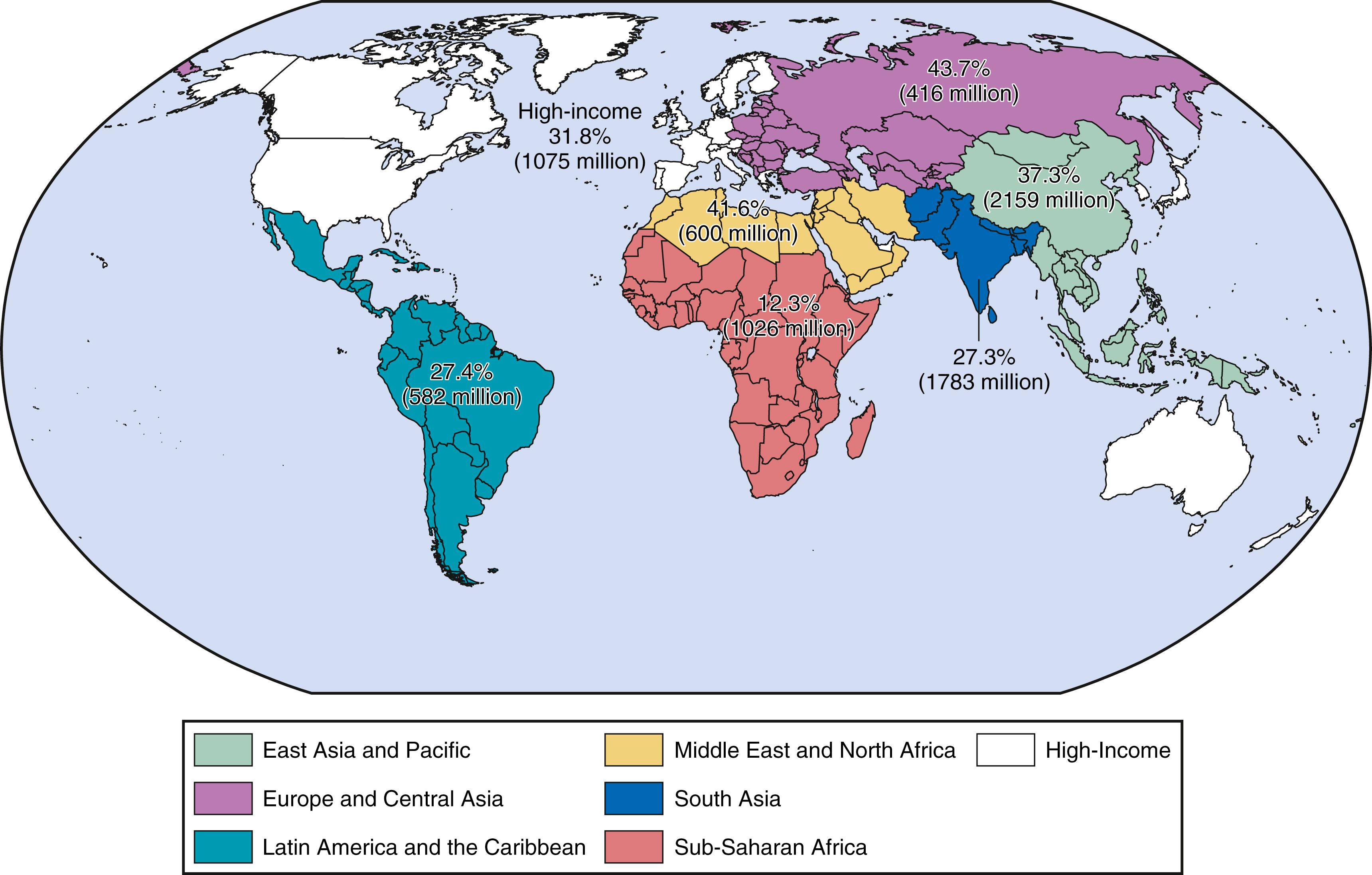
Between 1990 and 2017, deaths from cardiovascular disease (CVD) increased from 26% to 32% of all deaths globally, a reflection of the rapid epidemiologic transition, particularly in low- and middle-income countries (LMICs). Although the net percentage of deaths caused by CVD overall has increased, this reflects a rise in LMICs and a decline in high-income countries (HICs) ( Fig. 2.1 ). CVD now causes most deaths in all low- and middle-income regions, with the exception of sub-Saharan Africa, where it is the second leading cause of death overall, and the leading cause in those 50 years and older. In absolute numbers, five times as many CVD deaths occurred in the low- and middle-income regions combined than in the High-Income region in 2017 (14.8 million to 3 million). Within the six World Bank–defined low- and middle-income regions, the CVD burden differs vastly ( Fig. 2.2 ), with CVD deaths accounting for as much as 43.7% of all deaths in Europe and Central Asia and as little as 12.3% in sub-Saharan Africa. Cardiovascular disease accounts for 31.8% of deaths in HICs.
The overall increase in the global burden of CVD and the distinct regional patterns result in part from the “epidemiologic transition,” which includes four basic stages ( Table 2.1 ): Pestilence and Famine, Receding Pandemics, Degenerative and Man-Made Diseases, and Delayed Degenerative Diseases. , Movement through these stages has dramatically shifted the causes of death over the last two centuries, from infectious diseases and malnutrition in the first stage to CVD and cancer in the third and fourth stages. Although the transition through the stage of Pestilence and Famine has occurred much later in LMICs, it has also occurred more rapidly, driven largely by the transfer of low-cost agricultural technologies, the overall globalization of world economies, and public health advances.
| Stage | Description | Typical Proportion Of Deaths Caused By Cvd (%) | Predominant Types Of Cvd |
|---|---|---|---|
| Pestilence and famine | Predominance of malnutrition and infectious diseases as causes of death; high rates of infant and child mortality; low mean life expectancy. | <10 | Rheumatic heart disease, cardiomyopathies caused by infection and malnutrition |
| Receding pandemics | Improvements in nutrition and public health lead to decrease in rates of deaths caused by malnutrition and infection; precipitous decline in infant and child mortality rates. | 10–35 | Rheumatic valvular disease, hypertension, CHD, stroke |
| Degenerative and man-made diseases | Increased fat and caloric intake and decreased physical activity lead to emergency of hypertension and atherosclerosis; with increased life expectancy, mortality from chronic, noncommunicable diseases exceeds mortality from malnutrition and infectious diseases. | 35–65 | CHD, stroke |
| Delayed degenerative diseases | CVDs and cancer are the major causes of morbidity and mortality; better treatment and prevention efforts help avoid deaths among those with disease and delay primary events. Age-adjusted CVD mortality declines; CVD affects older and older individuals. | 40–50 | CHD, stroke, congestive heart failure |
| Inactivity and obesity | Increasing prevalence of obesity and diabetes; some slowing of CVD mortality rates in women. | 38 |
Humans evolved during the stage of Pestilence and Famine and have lived with epidemics and hunger for most of recorded history. Before 1900, infectious diseases and malnutrition constituted the most common causes of death in virtually every part of the world, with tuberculosis, pneumonia, and diarrheal diseases accounting for a majority of deaths. These conditions, along with high infant and child mortality rates, resulted in a mean life expectancy of approximately 30 years.
Per capita income and life expectancy increased during the stage of Receding Pandemics as the emergence of public health systems, cleaner water supplies, and improved food production and distribution combined to reduce deaths from infectious disease and malnutrition. Improvements in medical education and with other public health changes, contribute to dramatic declines in infectious disease mortality rates. Rheumatic valvular disease, hypertension, and cerebrovascular accident (stroke) cause most CVD. Coronary heart disease (CHD) often occurs at a lower prevalence rate than stroke, and CVD accounts for 10% to 35% of deaths.
During the stage of Degenerative and Man-Made Diseases, continued improvements in economic circumstances, combined with urbanization and radical changes in the nature of work-related activities, led to dramatic changes in diet, activity levels, and behaviors such as smoking. For example, in the United States, deaths from infectious diseases decreased to less than 50 per 100,000 people per year, and life expectancy increased to almost 70 years. The increased availability of foods high in calories, coupled with decreased physical activity, contribute to an increase in atherosclerosis. In this stage, CHD and stroke predominate, and between 35% and 65% of all deaths are related to CVD. Typically, the ratio of CHD to stroke is 2:1 to 3:1.
In the stage of Delayed Degenerative Diseases, CVD and cancer remain the major causes of morbidity and mortality, but CVD age-adjusted mortality rates decline by almost half, accounting for 25% to 40% of all deaths. Two significant advances have contributed to the decline in CVD mortality rates: new therapeutic approaches and prevention measures targeted at people with or at risk for CVD. ,
Treatments once considered advanced including the establishment of emergency medical systems, coronary care units, and the widespread use of new diagnostic and therapeutic technologies such as echocardiography, cardiac catheterization, percutaneous coronary intervention (PCI), bypass surgery, and implantation of pacemakers and defibrillators have now become the standard of care. Advances in drug development have also yielded major benefits on both acute and chronic outcomes. Efforts to improve the acute management of myocardial infarction (MI) led to the application of lifesaving interventions such as beta-adrenergic blocking agents (beta blockers), PCI, thrombolytics, statins, and angiotensin-converting enzyme (ACE) inhibitors (see Chapter 37, Chapter 38 ). Advances in both heart failure and diabetes management have led to new angiotensin-receptor neprilysin inhibitors, SGLT2 inhibitors, and GLP-1 agonists which reduce cardiovascular events. The widespread use of an “old” drug, aspirin, has also reduced the risk of dying of acute or secondary coronary events. Low-cost pharmacologic treatment for hypertension (see Chapter 26 ) and the development of highly effective cholesterol-lowering drugs such as statins have also made major contributions to both primary and secondary prevention by reducing CVD-related deaths (see Chapter 27 ).
In concert with these advances, public health campaigns have conveyed that certain behaviors increase the risk of CVD and that lifestyle modifications can reduce risk. In this regard, smoking cessation furnishes a model of success. In the United States, for example, 57% of men smoked cigarettes in 1955; in 2018, 15.6% of men smoked. The prevalence of smoking among U.S. women has fallen from 34% in 1965 to 13.7% in 2018. Campaigns from the 1970s dramatically improved the detection and treatment of hypertension in the United States. This intervention likely had an immediate and profound effect on stroke rates and a subtler effect on CHD rates. Public health messages concerning saturated fat and cholesterol had a similar impact on fat consumption and cholesterol levels. Population mean cholesterol levels also declined, from 220 mg/dL in the early 1960s to 191 mg/dL by 2016, with a simultaneous decrease in the prevalence of elevated low-density lipoprotein (LDL) cholesterol.
Troubling trends in certain risk behaviors and risk factors may foreshadow a new phase of epidemiologic transition, the stage of Inactivity and Obesity (see Chapter 31, Chapter 50 ). In many parts of the industrialized world, physical activity continues to decline while total caloric intake increases at alarming rates, resulting in an epidemic of overweight and obesity. Consequently, the rates of type 2 diabetes, hypertension, and lipid abnormalities associated with obesity are rising, a particularly evident trend in children. These changes are occurring while measurable improvements in other risk behaviors and risk factors, such as smoking, have slowed. If these trends continue, age-adjusted CVD mortality rates, which have declined over the past several decades in HICs, could plateau, as they have for young women in the United States, or even increase in the coming years. This trend pertains particularly to age-adjusted stroke death rates. This concerning increase in obesity also applies to LMICs.
Fortunately, recent trends in the first decade of the present century suggest a tapering in the increase in obesity rates among adults, although the rates remain alarmingly high at almost 42.4%. Furthermore, continued progress in the development and application of therapeutic advances and other secular changes appear to have offset the effects from the changes in obesity and diabetes; cholesterol levels, for example, continue to decline. Overall, in this decade, age-adjusted mortality has continued to decline at about 3% per year, from a rate of 341 per 100,000 population in 2000 to 223 per 100,000 in 2013.
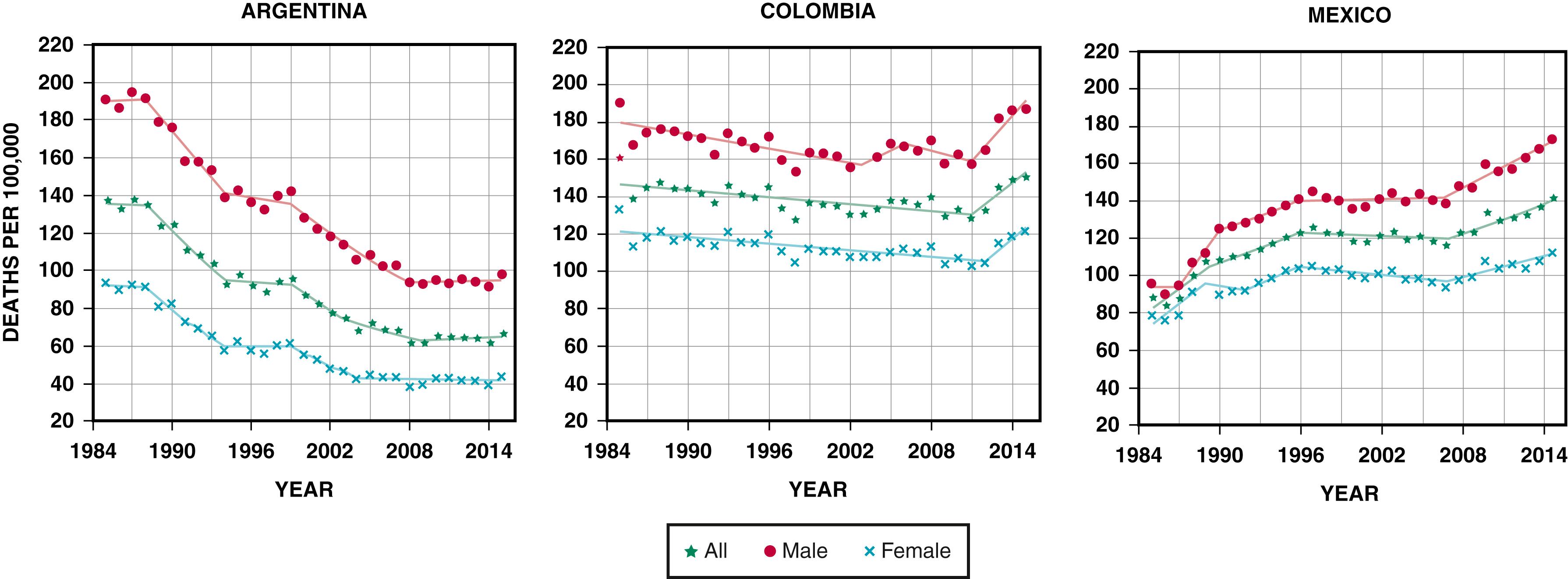
The HICs have followed different patterns of the CVD transition, which differ in both the peak of death rate from CHD and the time of transition. Three patterns emerge that rely on data from countries with an established death certification system. Countries in Latin America appear to follow the three different patterns as well ( Fig. 2.3 ). One pattern, followed by the United States and Canada, showed a rapid rise and peak in the 1960s and 1970s, followed by a relatively rapid decline through the end of the 2000s. The peak was 300 to 700 CHD deaths per 100,000 population, with current rates between 100 and 200 per 100,000. This pattern also occurred in the Scandinavian countries, the United Kingdom, Ireland, Australia, and New Zealand. In Latin America, Argentina has followed this pattern with a rapid decline from 1985 to 2016 with a CHD-related death rate of 70 per 100,000 at the end of the time period. A second pattern showed a peak in the same period in CHD-related deaths of 100 to 300 per 100,000. Countries such as Portugal, Spain, Italy, France, Greece, and Japan followed this pattern. Some countries did not have the same rapid decline in rate. In central European countries (Austria, Belgium, and Germany), the decline was slower compared to northern European countries (Finland, Sweden, Denmark, and Norway), but had lower peaks of 300 to 350 per 100,000 in the 1960s and 1970s. Colombia appears to follow this pattern with relatively flat to declining levels at 150 deaths per 100,000, with a small decline from 2010 to 2015. Some countries appear to display a third pattern of continued rise (particularly many components of the former Soviet Union), and others have yet to see any significant increase, such as many countries in sub-Saharan Africa (excluding South Africa). Mexico appears to follow this pattern with rates nearly doubling from 80 to 160 per 100,000 from 1985 to 2015. Whether other LMICs will follow a “classic” pattern of significant increases then rapid declines in rates (as happened in North America, Australia, and northwestern European HICs), a more gradual rise and fall (as in southern and central European countries), or some other pattern, will depend in part on cultural differences, secular trends, and responses at the country level with regard to both public health and treatment infrastructures.
Three phenomena impact the various metrics of disease burden. First, population growth increases the overall number of deaths caused by CVD globally. Second, a trend in general aging of the population has shifted the proportion of deaths caused by CVD in most regions as a result of better control of many communicable diseases that manifest at early stages. Third, prevention of CVD and treatment for those with CVD have both improved, which reduces age-adjusted mortality rates. We rely on data from the Global Burden of Disease (GBD) study data from 2017. Although extensive, data from GBD 2017 have limitations. The availability and reliability of data on the cause of death, especially in LMICs without standardized protocols, are uncertain.
Globally, CVD-related deaths increased by 49% between 1990 and 2017. The increase in overall CVD-related deaths results from both increases in CHD and stroke-related deaths. CHD was the leading cause of death in 2017, accounting for 16% of all deaths worldwide. The second-ranking cause of death was stroke, at 11%. An estimated 15.1 million people died from CHD and stroke, which together accounted for more than a quarter of all deaths worldwide in 2017.
Although still substantial, deaths from communicable, neonatal, and maternal diseases are decreasing worldwide, with a 32.5% decrease between 1990 and 2017. Deaths from noncommunicable diseases increased by 53% in the same period. In 2017, CHD accounted for the largest portion of global years of life lost (YLLs) and the second highest of DALYs. Stroke was the third-ranking contributor to both global YLLs and DALYs. On the other hand, in 1990, communicable diseases accounted for the largest portion of both YLLs and DALYs.
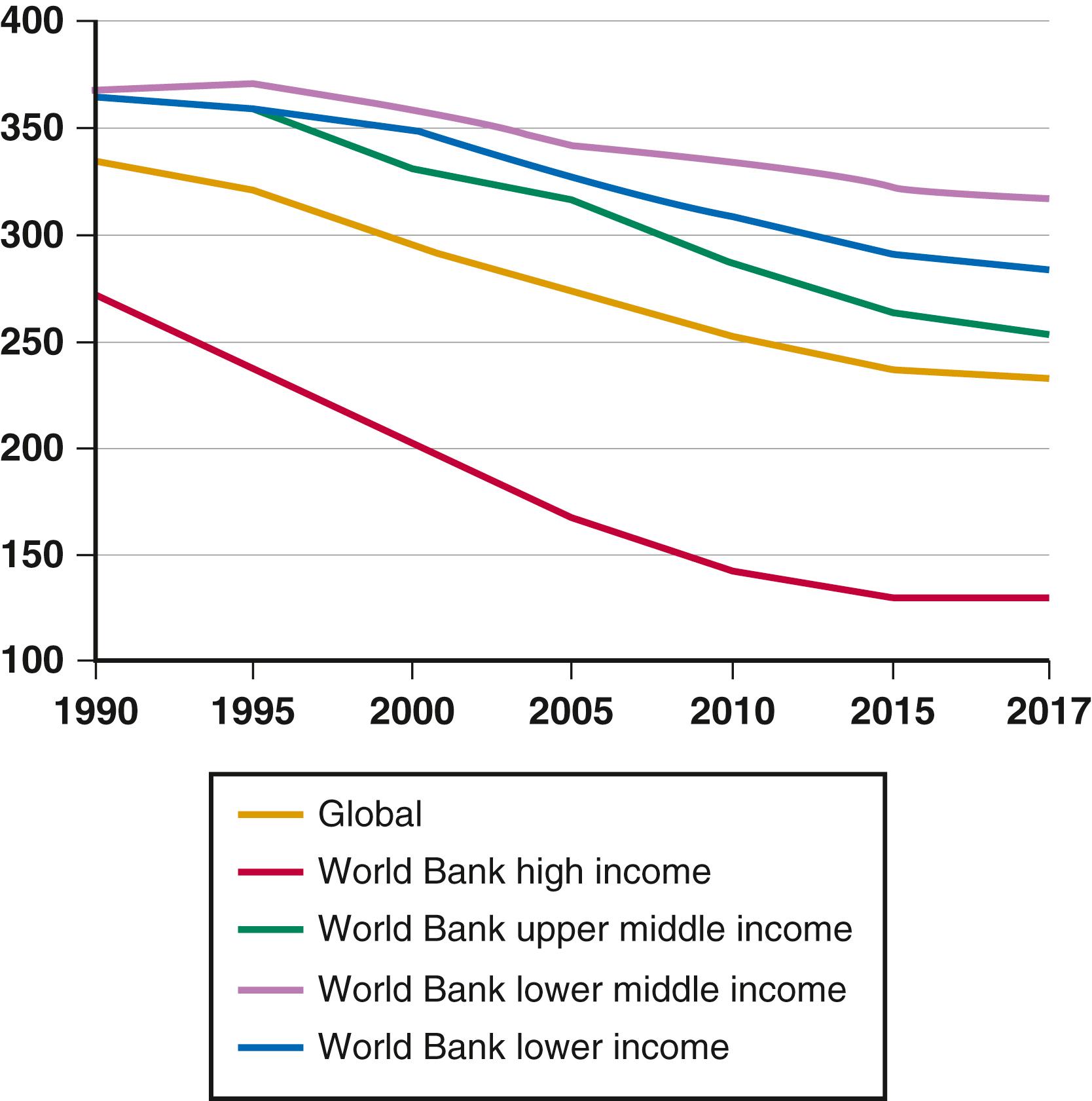
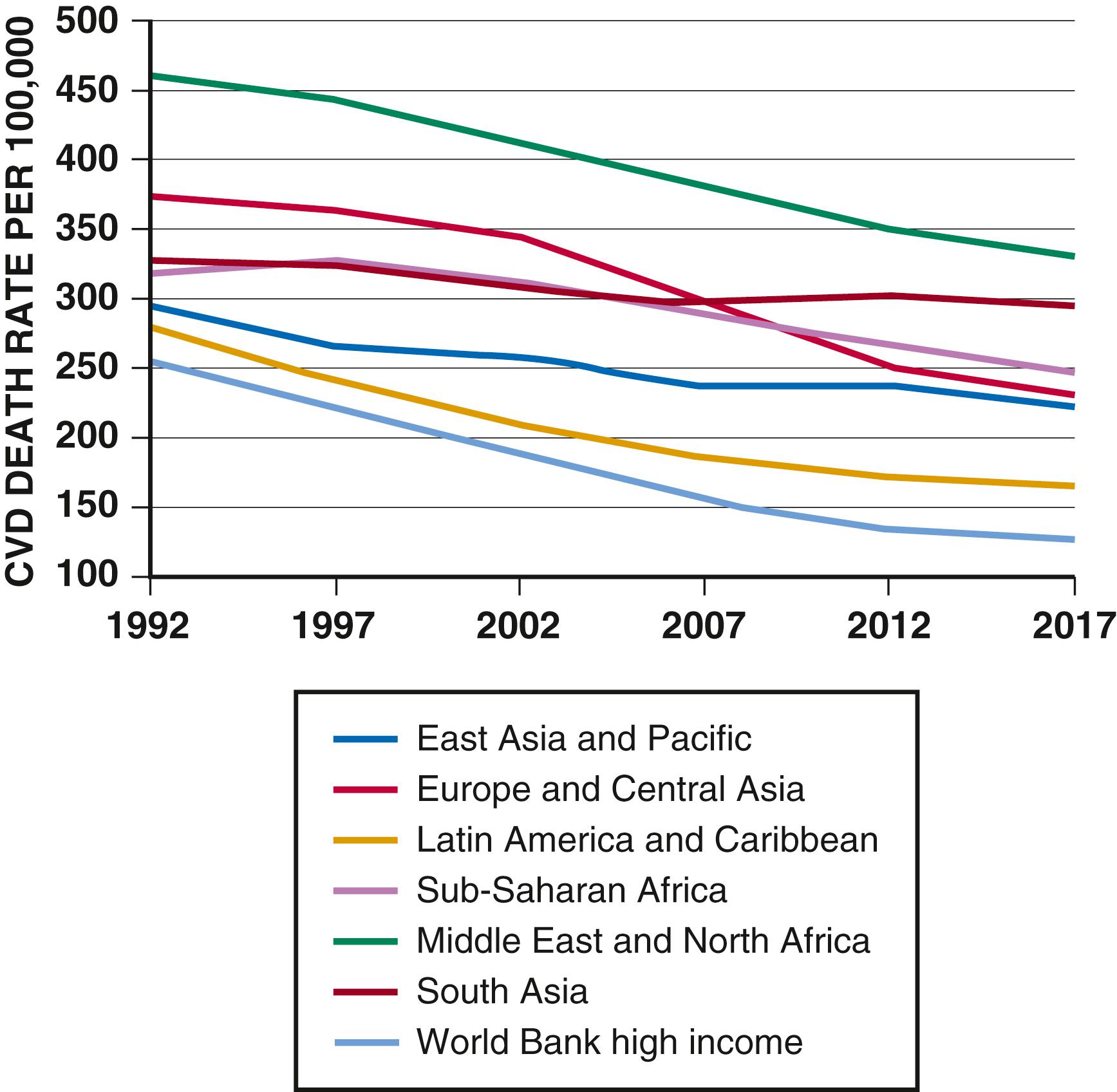
Despite the increase in overall CVD-related deaths, the age-adjusted death rates decreased by 30.4% in the same period, from 335 to 233 per 100,000 population, suggesting significant delays in the age of occurrence and/or improvements in case-fatality rates. Unfortunately, not all countries share in the reductions. Examination of regional trends is helpful in estimating global trends in the burden of disease, particularly CVD. Because 85% of the world’s population lives in LMICs, these countries largely drive global CVD rates. These estimates depend on modeling mortality rates in areas where established death certification–based vital registration systems do not cover the entire country. Even as age-adjusted rates have been falling globally, the pattern is different when assessed by income ( Fig. 2.4 ) or by region ( Fig. 2.5 ).
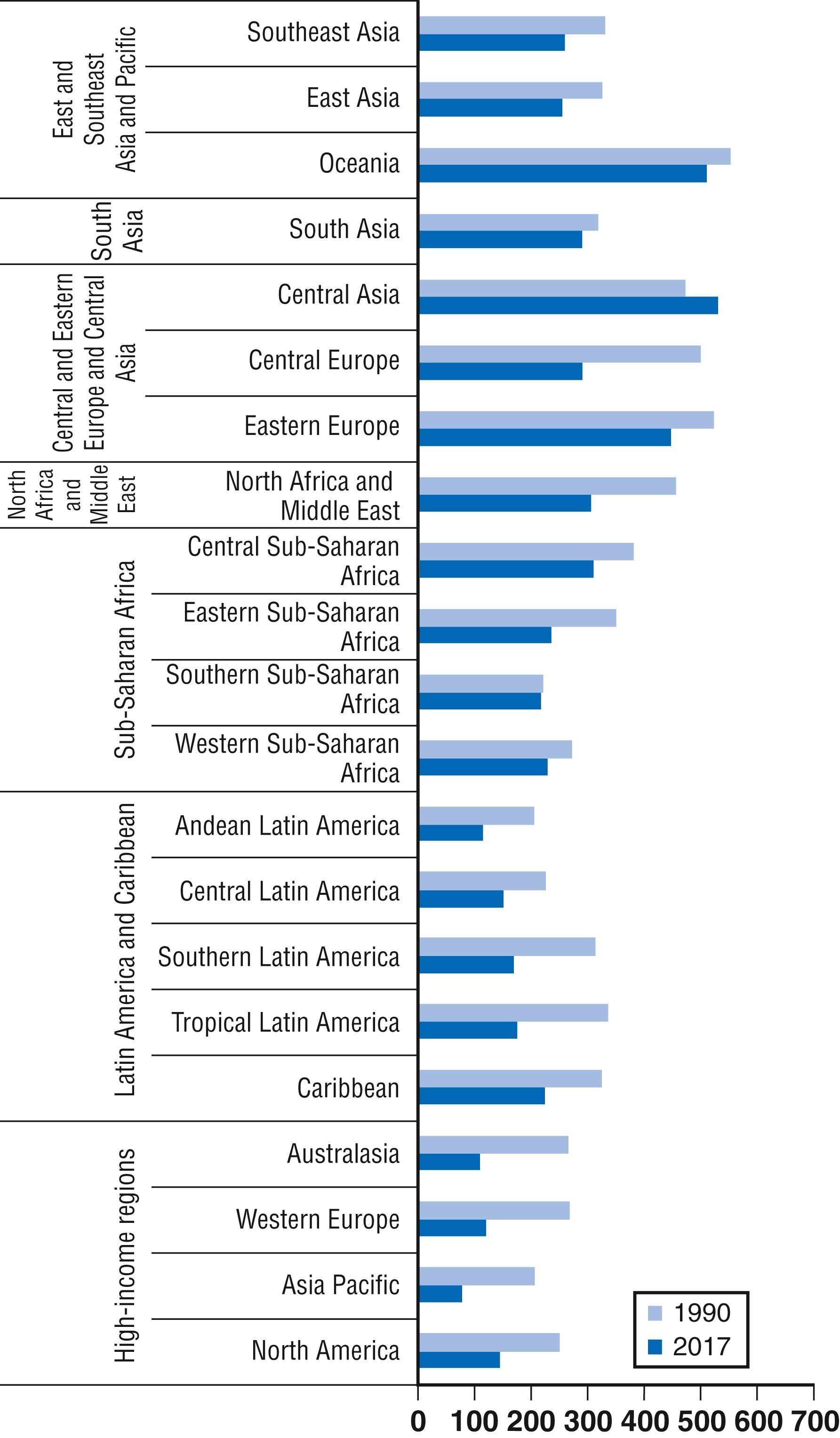
The magnitude of the peak of the CVD epidemic, and whether the peak has arrived at all, has a great range. Here we describe and highlight trends in the seven regions of the world as defined by the GBD project, which includes HICs as one grouping and divides the remaining LMICs into six geographic regions, further divided by sub-regions: the High-Income, East Asia and Oceania, Central and Eastern Europe and Central Asia, Latin America and Caribbean, Middle East and North Africa, and sub-Saharan Africa regions. All these regions had declines in age-adjusted CVD mortality rates from 1990 to 2017. South Asia had only a slight decrease in its age-adjusted CVD mortality rates.
Much of the variation is related to income, which is one proxy for the stages of the epidemiologic transition. Looking at age-adjusted CVD-related death rates by World Bank, the high-income regions had different trends over the last two and a half decades. In the low-income region, the death rate has decreased from 364 to 285 per 100,000 between 1990 and 2017. The Lower Middle-Income region saw a small increase (368 to 371 per 100,000) between 1990 and 1995, followed by a fall to 317 per 100,000 in 2017. The upper middle-income region saw a 30% decline, from 365 to 254 per 100,000 between 1990 and 2017. The high-income region had a 53% decline, from 272 to 128 CVD deaths per 100,000.
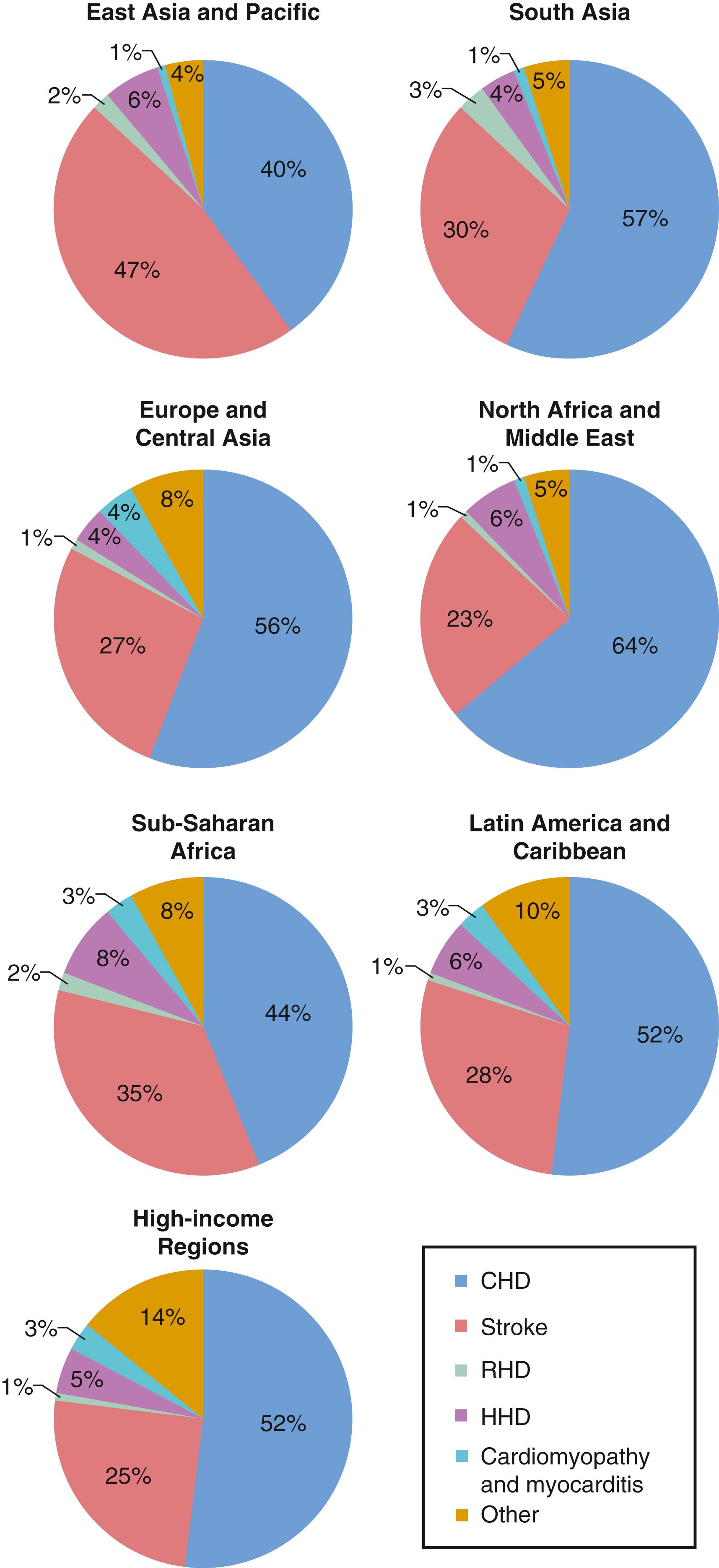
The LMICs have a high degree of heterogeneity with respect to the phase of the epidemiologic transition. First, LMIC sub-regions differ by age-adjusted CVD death rates ( Fig. 2.6 ). Next, low- and middle-income sub-regions are unique, as illustrated by the different CVD disease rates by cause in each region ( Fig. 2.7 ). Lastly, in the East Asia and Oceania region, stroke still exceeds CHD as a cause of CVD-related death. Hypertensive heart disease is the largest single contributor among remaining causes of CVD morbidity and mortality, and sub-Saharan Africa remains the region with the largest contribution from this cause.
Variability in disease prevalence among various regions likely results from multiple factors. First, the countries are in various phases of the epidemiologic transition described earlier. Second, the regions may have cultural and genetic differences that lead to varying levels of CVD risk. For example, per capita consumption of dairy products (and thus consumption of saturated fat) is much higher in India than in China, although it is rising in both countries. Third, certain additional competing pressures exist in some regions, such as war or infectious diseases (HIV/AIDS) in sub-Saharan Africa.
Because CHD affects a younger population in LMICs, the number of deaths is increased in the working population. For some LMICs, the severity of the epidemiologic transition has appeared to follow a reverse social gradient, with members of lower socioeconomic groups having the greatest rates of CHD and the highest levels of various risk factors. Unfortunately, reductions in risk factors do not follow the same trend. Compared with people in the upper and middle socioeconomic strata, those in the lowest stratum are less likely to acquire and apply information on risk factors and behavior modifications or to have access to advanced treatment. Consequently, CVD mortality rates decline later among those of lower socioeconomic status.
In 2017, CVD accounted for almost 32% of all deaths in high-income regions, and more than half of these deaths were due to CHD (see Fig. 2.7 ). The movement of most HICs through the epidemiologic transition, with rising levels of risk factors and CVD death rates until the 1970s and then declines in both over the next 40 years, is similar to what occurred in the United States. CHD is the dominant form, with death rates per 100,000 twice as high as stroke rates. In Portugal however, stroke rates for women exceed CHD rates.
Age-adjusted mortality for CVD declined in all HICs. This age-adjusted decline results largely from preventive interventions that allow people to avert the disease, treatments to prevent death during an acute manifestation of the disease (particularly stroke or MI), and interventions that prolong survival once CVD manifests. Thus the average age at death from CVD continues to increase, and as a result, CVD affects a larger retired population.
Of the five sub-regions, Western Europe, with an overall CVD mortality rate of 313 per 100,000 in 2017, and Southern Latin America, with an age-standardized rate of 172 per 100,000, had the highest mortality rates, whereas Australasia and Southern Latin America tied for the lowest overall (222/100,000) rate, and high-income Asia Pacific had the lowest age-adjusted rate (80/100,000). As mentioned, high-income regions have higher mortality rates for CHD than for stroke. Japan is unique among HICs; as its communicable disease rates fell in the early 20th century, its stroke rates increased drastically. CHD rates, however, did not rise as sharply in Japan as in other industrialized nations and have remained lower than in any other industrialized country. Overall, CVD rates have dropped to 60% in Japan since the 1960s, largely because of a decrease in age-adjusted stroke rates. Japanese men and women currently have the highest life expectancy in the world: 87.3 years for women and 81.3 years for men. The difference between Japan and other industrialized countries may stem in part from genetic factors, although the traditional Japanese fish- and plant-based, low-fat diet and resultant low cholesterol levels may have also contributed. Nevertheless, as in many other countries, dietary habits in Japan are undergoing substantial changes. Since the late 1950s, cholesterol levels have progressively increased in both urban and rural populations. Although the prevalence of CVD risk factors is increasing in the Japanese population, the incidence of coronary artery disease remains low and even declined. This situation could change, however, because there seems to be a long lag phase before dietary changes manifest as CHD events.
The East Asia and Pacific (EAP) region is the most populated low- and middle-income region in the world, with 2.2 billion people; approximately 56% of the region is urban. The gross national income (GNI) per capita is $7601, ranging from $12,060 and $10,590 in Nauru and Malaysia to $1310 in Myanmar. In 2017, total health expenditure was 4.9% of total gross domestic product (GDP), or $344 per capita. The region is divided into three distinct sub-regions: Southeast Asia, East Asia, and Oceania. China is by far the most populated country, representing 65% of the region. Life expectancy has risen quickly across the EAP region in past decades, up to an average of 75 years. In China the increase has been dramatic: from 37 years in the mid-1950s to 77 years in 2018. This increase associates with a large rural to urban migration pattern, rapid urban modernization, aging of the population, decreased birth rates, major dietary changes, increasing tobacco use, and a transition to work requiring low levels of physical activity.
CVD caused more than 6.3 million deaths in the EAP region in 2017, accounting for 37% of all deaths in the region. Almost half of these deaths resulted from stroke, whereas 40% were caused by CHD (see Fig. 2.7 ). CVD death rates differ significantly between sub-regions, most notably in Southeast Asia. Age-adjusted CVD mortality rates were highest in Oceania, at 517 per 100,000 in 2017, even though the overall mortality for CVD was 253 per 100,000, suggesting that many premature deaths from CVD occurred in Oceania.
Stroke and CHD are the lead causes of death in all three sub-regions. Whereas stroke and CHD rates increased in both East Asia and Southeast Asia between 1990 and 2017, stroke rates decreased slightly in Oceania, from 87 to 83 per 100,000. China is straddling the second and third stages of a Japanese-like epidemiologic transition. Men in China age 50 to 69 have stroke death rates of 232 per 100,000, versus CHD death rates of 168 per 100,000.
Of the three sub-regions that constitute this region (Central Asia, Central Europe, and Eastern Europe), Eastern Europe is the most populated. Russia alone accounts for 35% of the region’s 416 million inhabitants. Sixty-seven percent of the population in the region is urban, with an average life expectancy of 73.7 years. The average GNI per capita for the region ranges from $1010 in Tajikistan to $24,500 in Slovenia. Russia has a GNI of $10,230. On average, the region spends 5.2% of its total GDP on public and private health care. Health expenditure per capita ranges from $58 per capita in Tajikistan to $1920 in Slovenia. Russia spends about $586 per capita, or 5.3% of its GDP.
The highest rates of CVD mortality, both overall and age-adjusted, have occurred in this region for the entire span of the GBD project. Overall CVD mortality rates are 747 per 100,000 in Eastern Europe, 569 per 100,000 in Central Europe, and 359 per 100,000 in Central Asia. Overall rates are similar to or exceed those seen in the United States in the 1960s, when CVD peaked. CHD is generally more common than stroke, which suggests that the countries that constitute Eastern Europe and Central Asia remain largely in the third phase of the epidemiologic transition. As expected in this phase, people who develop and die of CVD have a lower average age than those in HICs. In 2017, CVD accounted for 54% of all deaths in the region, 56% of which resulted from CHD and 27% from stroke.
A country-level analysis reveals important differences in CHD profiles within the Central and Eastern Europe and Central Asia region (see Fig. 2.3 ). Since the dissolution of the Soviet Union, CVD rates have increased surprisingly in some of these countries, with overall rates of 956, 769, and 684 per 100,000 in Ukraine, Belarus, and Russia, respectively. Of note, deaths resulting from CHD in these countries affect not only older adults; the GBD study estimates that working-age populations (15 to 69 years) have a significant CHD burden. Almost one third of all deaths in persons age 45 to 49 years, for example, result from CVD. For people age 60 to 64 years, CVD accounts for almost half of all deaths, and 60% of CVD-related deaths are caused by CHD.
The Latin America and Caribbean (LAM) region comprises Andean Latin America, Central Latin America, Tropical Latin America, and the Caribbean. The region has a total population of 582 million, 80% of which is urban. Brazil, the region’s most populous country, represents about one third of the population (36%), with Colombia, Mexico, Peru, and Venezuela making up another 41%. The Caribbean nations account for 8% of the population in the region. Life expectancy in the LAM region is approximately 75 years but varies greatly. In 2018, for example, Haiti and Chile had life expectancies of 64 years and 80 years, respectively. Average GNI per capita in the region is about $8696 (purchasing power parity [PPP] of $15,944). The region spends an average of 8.0% of its GDP on health care. This level of spending translates into health care expenditures that range from $62 per capita in Haiti to $1772 per capita in The Bahamas.
The LAM region bears a substantial CVD burden. In 2017, CVD caused 27% of all deaths in the region. As in HICs, CHD dominates among circulatory diseases (see Fig. 2.7 ). Mortality rates vary significantly by sub-region. The Caribbean has the highest age-standardized mortality rates for CHD and stroke: 115 deaths per 100,000 and 69 per 100,000, respectively. Andean Latin America had the lowest: 61 and 34 deaths per 100,000, respectively. As with other global trends, overall mortality for the region increased slightly between 1990 and 2017, but age-adjusted mortality declined significantly. Between 1990 and 2017, age-adjusted CVD death rates nearly halved in Tropical Latin America while decreases of 44%, 33%, and 31% occurred in Andean Latin America, Central Latin America, and the Caribbean, respectively. Together, CHD (15%), stroke (5.9%), and hypertensive heart disease (1.6%) accounted for almost one quarter of all deaths in Central Latin America in 2017. Age-adjusted overall CVD, CHD, and stroke mortality rates decreased in this sub-region between 1990 and 2017, but to a lesser extent than for global changes. The lower reductions in the LAM region may result from rapid lifestyle changes: unfavorable dietary changes, increased smoking, increased obesity, and less exercise.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here