Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Gastrointestinal (GI) bleeding in children can range from small amounts of blood in the stool, associated with milk protein allergy or anal fissure, to life-threatening hemorrhage, associated with portal hypertension or peptic ulcer disease. Severe bleeding is a true medical emergency and necessitates prompt diagnostic attention and appropriate management since overall mortality of children hospitalized in the United States with GI bleeding is approximately 2%. Hemodynamic stabilization of the patient with severe bleeding should always precede diagnostic studies . An accurate history and thorough physical examination usually allow the physician to categorize the problem as mild or severe and to direct evaluation at the appropriate pace.
Children with GI bleeding generally present with hematemesis, hematochezia, or melena, although the clinical manifestation can be as subtle as evidence of occult blood loss. An upper GI bleed is bleeding from the esophagus, stomach, or duodenum. Upper sources account for the majority of GI bleeds in children. If the site of bleeding is distal to the ligament of Treitz, it is a lower GI bleed . Blood passed per rectum can originate from either an upper or lower GI source. Occult bleeding may occur from disorders at numerous sites.
Vomited blood can be either red or the color of coffee grounds. Hematemesis is most commonly associated with an upper GI bleed, although swallowed blood produces the same clinical picture. Bright red hematemesis suggests active bleeding that has not had prolonged contact with gastric secretions. When gastric secretions interact with the blood, the blood will darken in color as the iron oxidizes and leads to dark red or “coffee ground” emesis.
The presence of hematochezia (bright red blood) is generally associated with colonic bleeding, although it may result from a brisk upper bleed. Maroon stools from the rectum are generally associated with a lower GI bleed. The presence of melena—passage of black, tarry stools—generally results from significant blood loss proximal to the ileocecal valve, with up to 90% originating proximal to the ligament of Treitz. The color results from bacterial breakdown of the hemoglobin. Up to 10–15% of upper GI bleeds present with melena in the absence of hematemesis. These patients are more likely to have a clinically significant bleed.
In contrast to overt GI bleeding as in hematemesis, hematochezia, or melena, occult GI bleeding is a positive fecal blood test when there is no visible blood loss.
Hemoptysis may occasionally be mistaken for hematemesis. Melena may be confused with menstrual bleeding. In addition, certain medications, supplements (such as iron), foods, and dyes may turn stool or emesis red or maroon color, mimicking blood. A thorough history including respiratory symptoms, menstrual history, medications, and diet history is important.
The first step is to determine whether the problem is actually GI bleeding. Many substances and non-GI sources may simulate GI bleeding ( Table 16.1 ). Occult blood testing consists of guaiac-based tests from the stool or emesis (gastric occult blood), which measure heme, and fecal immunochemical tests (FITs), which measure the globin portion of human hemoglobin. Recommendations for guaiac-based testing from manufacturers are to avoid red meat, citrus fruits and juices, supplemental vitamin C in excess of 250 mg/day for 3 days prior to testing, and antacids for at least 60 minutes prior to testing. Nonsteroidal antiinflammatory drugs (NSAIDs) should be avoided for 1 week prior to testing and aspirin exposure should be minimized; however, it is uncertain whether these products affect the reliability of the test. In addition, although iron preparations may blacken stools, they do not lead to false-positive results. Female patients should be told not to collect test samples for 3 days after or during a menstrual period. To avoid potential false-positive or false-negative results, stool should be collected from diapers or from disposable collection devices rather than directly from toilet water. Finally, an alkali denaturation test, also known as the Apt-Downey or Apt test, should be performed when a breast-fed infant vomits bright red blood or passes red bloody stools to distinguish whether it is maternal or fetal hemoglobin.
|
Once GI bleeding is confirmed, the evaluation, differential diagnosis, and therapeutic interventions will depend on the age of the patient, severity of bleeding, and whether the bleed is coming from the upper or the lower GI tract ( Tables 16.2, 16.3, 16.4, and 16.5 ). A nasogastric (NG) tube may be placed in the appropriate patient when the source of bleeding is not clear. Bloody aspirate from the stomach is confirmation of upper GI bleeding. The tube may then be used to lavage the stomach with warm saline. If aspirated saline clears after repeated lavage, the bleeding has likely stopped or is from a different source.
| Infants | Ill-appearing | Stress ulcer |
| Hemorrhagic gastritis | ||
| Sepsis with DIC | ||
| Vitamin K deficiency | ||
| Infection—CMV, herpes, parasites, fungal | ||
| Trauma | ||
| Well-appearing | Milk protein sensitivity | |
| Mallory-Weiss tear | ||
| Prolapse gastropathy | ||
| Reflux esophagitis | ||
| Reactive gastritis | ||
| Anatomic anomalies (duplication) ∗ | ||
| Vascular anomalies (hemangioma/vascular malformation) ∗ | ||
| Children | Ill-appearing | Esophageal varices |
| Stress ulcer | ||
| Sepsis with DIC | ||
| Hemobilia | ||
| Well-appearing | Esophagitis including pill ulceration (alendronate, tetracycline, quinidine, potassium chloride, aspirin, NSAIDs) | |
| Reflux esophagitis | ||
Gastritis
|
||
| Ulcer from foreign body | ||
| Mallory-Weiss tear | ||
| Prolapse gastropathy | ||
Vascular malformation ∗
|
||
| Anatomic anomalies (duplication) ∗ | ||
| Infection—CMV, herpes, parasites, fungal |
∗ Patient is usually well-appearing but may deteriorate due to high rate of bleeding.
| Infants | Ill-appearing | Infectious— Salmonella , Shigella , Escherichia coli O157:H7, Campylobacter species, Yersinia species, Entamoeba histolytica, CMV |
| Ischemia—volvulus or necrotizing enterocolitis | ||
| Sepsis with DIC | ||
| Vitamin K deficiency | ||
| Hirschsprung enterocolitis | ||
| Intussusception | ||
| Trauma | ||
| Well-appearing | Anal fissure | |
| Milk protein sensitivity/eosinophilic proctocolitis | ||
| Lymphonodular hyperplasia | ||
| Vascular anomalies (hemangioma/vascular malformation) ∗ | ||
| Anatomic anomalies | ||
| Children | Ill-appearing | Infectious—above plus Clostridium difficile |
| Intussusception | ||
| Meckel diverticulum | ||
| Inflammatory bowel disease | ||
| Ischemia | ||
| Typhlitis | ||
| Henoch-Schönlein purpura | ||
| Trauma | ||
| Well-appearing | Anal fissure | |
| Milk and other protein sensitivity | ||
| Juvenile polyp | ||
Medication
|
||
| Lymphonodular hyperplasia | ||
| Hemorrhoid (in chronic liver disease) | ||
| Vascular anomalies (hemangioma/vascular malformation) ∗ | ||
| Anatomic anomalies |
∗ Patient is usually well-appearing but may deteriorate due to high rate of bleeding.
| Inflammatory Causes |
|
|
|
|
|
|
|
|
| Vascular Causes |
|
|
|
|
| Drugs |
|
| Extragastrointestinal Causes |
|
|
|
| Infectious Causes |
|
|
|
|
|
| Tumors and Neoplastic Causes |
|
|
|
|
|
| Artificial Causes |
|
|
|
| Miscellaneous Causes |
|
|
|
| Hematemesis/Melena |
|
| Hematochezia |
|
Neonates who did not receive prophylactic vitamin K are at risk for hemorrhagic disease of the newborn (see Chapter 51 ) and additional perinatal factors may place them at risk for sepsis or other stress that could lead to gastritis. Infants who require intensive care may have trauma from an NG tube, and infants with neonatal umbilical vein catheterization or neonatal omphalitis are at risk for portal vein thrombosis and resultant later onset of esophageal varices. In older children, a recent history of vomiting, regurgitation, or abdominal pain suggests a mucosal lesion. Forceful, repeated vomiting may result in a Mallory-Weiss tear or prolapse gastropathy. Reactive gastritis can be due to medications such as NSAIDs as well as alcohol or ingestion of caustic substances. Providers must ask about recent bleeding such as epistaxis or dental procedures, which could lead to hematemesis without a GI source of bleeding.
Information regarding chronic pulmonary disease, renal disease, bleeding disorders such as hemophilia, platelet dysfunction or von Willebrand disease, and liver disease, including a history of jaundice, should be obtained in all children. Patients with cystic fibrosis are at risk not only for the development of esophageal varices caused by biliary cirrhosis but also for coagulopathies from vitamin K deficiency. They may also have hemoptysis, which can be misinterpreted as hematemesis. In patients with renal disease, uremia will cause platelet dysfunction, which may manifest as a GI bleed. The family history should address the presence of bleeding disorders, peptic ulcer disease, and possible Helicobacter pylori exposure. Other genetic disorders may be elicited in the family history such as VMCM (venous malformations, multiple cutaneous and mucosal, OMIM 600195 ), hereditary hemorrhagic telangiectasia, Peutz-Jeghers syndrome, and blue rubber bleb nevus syndrome that cause variable GI bleeding.
Immediate attention must be given to signs of hypovolemia, anemia, or shock. An orthostatic change, such as a pulse rate increase of 20 beats/min or a drop in systolic blood pressure of more than 10 mm Hg when the patient changes from supine to standing, is a sensitive index of significant volume depletion. Blood pressure may remain normal up to the point of circulatory collapse in children and a normal blood pressure should not be reassuring in the setting of other signs of hypovolemia such as tachycardia or delayed capillary refill.
In addition to close attention to changes in vital signs, a physical exam with emphasis on potential sources of bleeding is essential ( Table 16.6 ). The oropharynx and nasal canals should be examined for lesions as the cause of bleeding. Palpation to evaluate organomegaly should begin at the iliac crests so as not to miss a hugely enlarged liver or spleen. A prominent venous pattern on the abdomen ( Fig. 16.1 ), splenomegaly, and ascites may suggest portal hypertension. Tenderness and guarding indicate a significant inflammatory process.
| Exam Finding | Associated Disorder |
|---|---|
| Splenomegaly Caput medusae |
Portal hypertension and esophageal varices |
| Palmar erythema Spider angioma Jaundice Ascites |
Liver disease |
| Hemangioma | Hemangioma in gastrointestinal tract |
| Port-wine stain | Vascular malformation in gastrointestinal tract |
| Palpable purpura | Henoch-Schönlein purpura or other vasculitis |
| Hyperpigmented lesions of the oral or anal mucosa | Peutz-Jeghers syndrome (gastrointestinal polyps) |
| Lip, oral mucosal telangiectasias | Hereditary hemorrhagic telangiectasia |
| Oral ulcers Perianal fistula Perianal skin tag Erythema nodosum Pyoderma gangrenosum |
Inflammatory bowel disease |

In addition to assessing for pallor, cutaneous lesions may help determine the underlying cause of bleeding. Petechiae can indicate disseminated intravascular coagulation, hypersplenism, or another bleeding abnormality. Hyperpigmented lesions of the oral or anal mucosa may indicate Peutz-Jeghers disease ( Fig. 16.2 ). Cutaneous telangiectasia and hemangiomas may indicate such diseases as Osler-Weber-Rendu syndrome (a.k.a. hereditary hemorrhagic telangiectasia) ( Fig. 16.3 ) and ataxia-telangiectasia, or they may simply suggest a predisposition for vascular malformations. However, only about 2% of individuals with cutaneous vascular lesions will also have GI involvement. Blue cutaneous nodules suggest blue rubber bleb nevus syndrome ( Fig. 16.4 ). Palmar erythema, spider angioma, or jaundice suggests underlying liver disease. Scleral icterus may be subtle but can be the first sign of liver disease and may be more easily appreciated than jaundice in darker-skinned individuals.



In infants, esophagitis, gastritis, and ulcers are the most common causes of upper GI bleeding. Esophagitis may be associated with dysphagia, irritability, and arching with feeds (see Chapter 15 ). Milk protein sensitivity should be considered as well, although it more often presents with blood in stool. Trauma or infection (such as cytomegalovirus, herpes simplex, parasites, or fungal) can cause mucosal irritation presenting as hematemesis. Anatomic abnormalities including duplication cysts or vascular abnormalities may also lead to hematemesis or melena in infants.
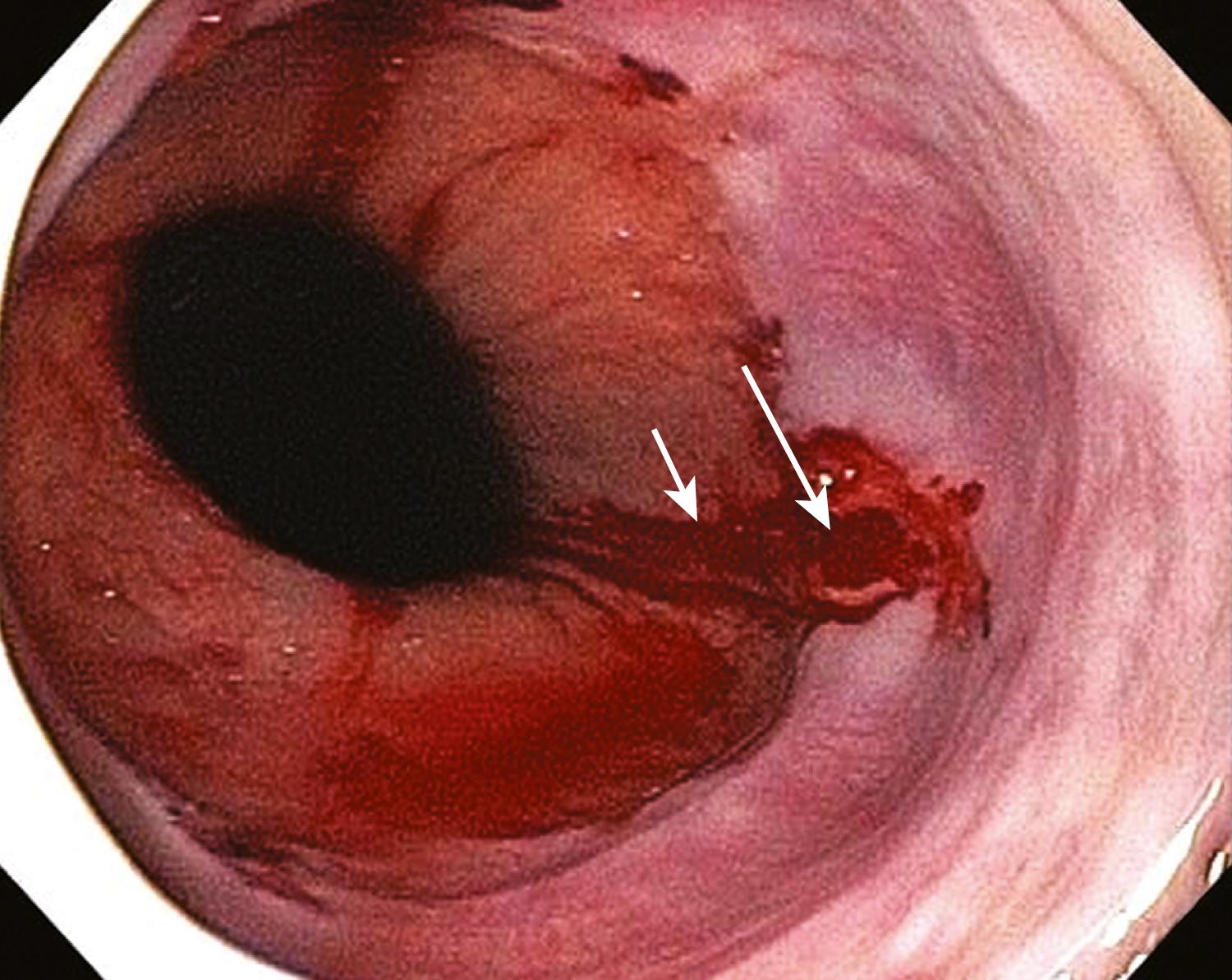
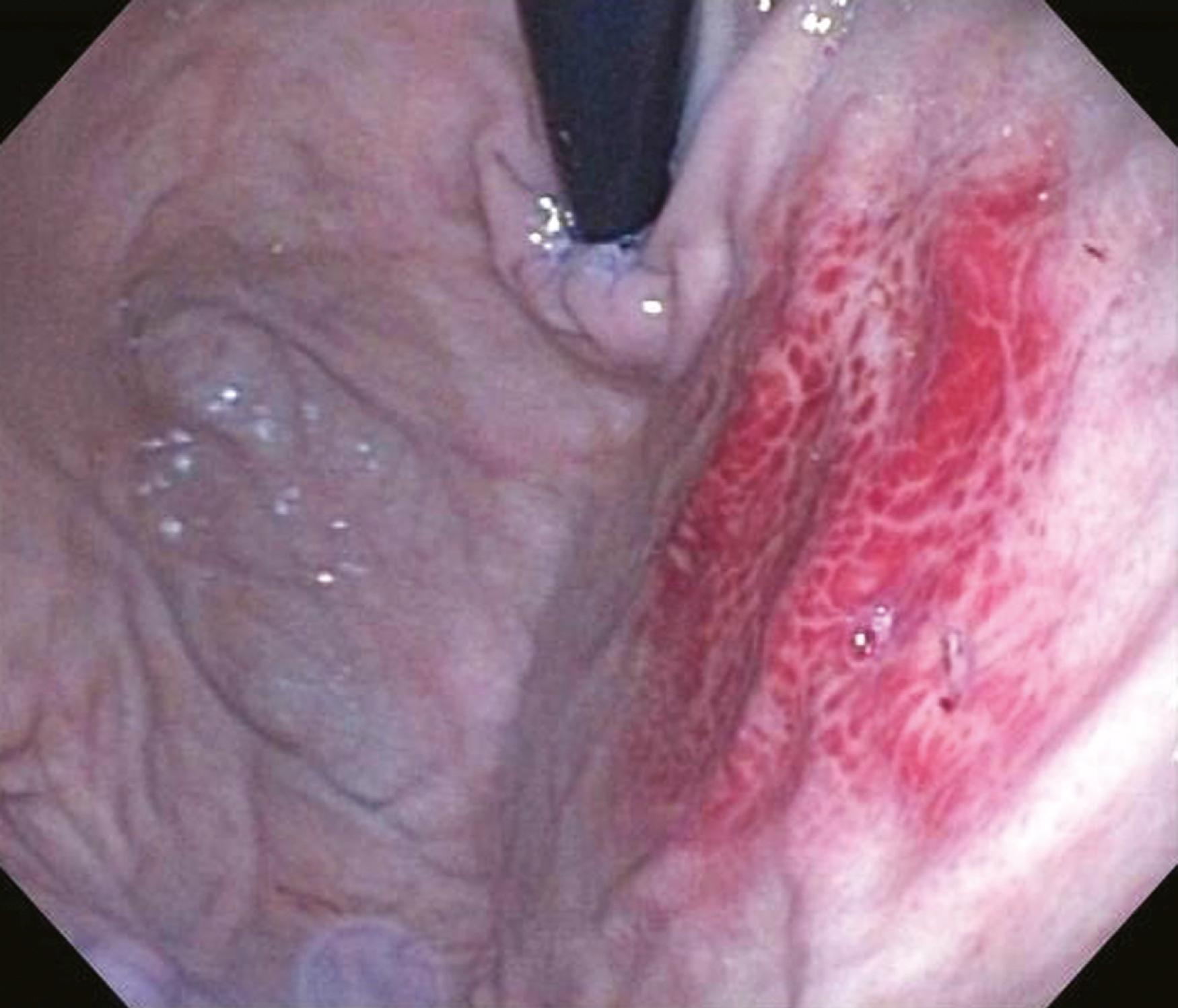
In older children, mucosal lesions remain common causes of bleeding. Mallory-Weiss tears are associated with repeated forceful vomiting from a variety of causes (e.g., acute gastroenteritis) ( Fig. 16.5 ). The forcefulness of the vomiting causes a tear in the distal esophagus at the level of the lower esophageal sphincter. The history is generally one of frequent nonbloody vomiting that then becomes hematemesis. Prolapse gastropathy, caused by prolapse of gastric mucosa into the distal esophagus, can similarly occur after forceful vomiting and lead to hematemesis ( Fig. 16.6 ). Reactive gastritis secondary to medication (NSAIDs) or infection ( H. pylori ) is also a common cause of upper GI bleeding. Children with known or unknown liver disease can develop esophageal varices that may lead to large-volume hematemesis and melena (or hematochezia if bleeding is brisk). Ulcers, although rare, can also lead to significant blood loss and may be related to H. pylori infection, stress such as surgery or burns, and foreign body ingestion, specifically button batteries, which can lead to significant bleeding.
Chronicity of bleeding is essential to ascertain because infectious colitis may cause acute bloody diarrhea, while inflammatory bowel disease generally presents with a more prolonged history (see Chapter 14 ). Presence or absence of pain can also help distinguish between causes of bleeding. Severe, acute abdominal pain is often present in patients with vascular compromise, such as in intussusception, midgut volvulus, and bowel ischemia (e.g., Henoch-Schönlein purpura), while painless rectal bleeding suggests a Meckel diverticulum, polyp, or angiodysplasia. Growth failure is suggestive of inflammatory bowel disease, specifically Crohn disease; constipation points to the possibility of an anal fissure (see Chapter 19 ) or Hirschsprung disease with enterocolitis. Information regarding travel (either by the patient or by visitors), sick contacts, daycare exposure, camping, and antibiotic exposure may reveal potential infectious causes. Family history of polyps or colon cancer is important given the inherited polyposis syndromes, as is a family history of inflammatory bowel disease.
Physical exam in any patient with GI bleeding must begin with assessment of hemodynamic status. In addition to a general exam, for patients with hematochezia, a rectal exam is important to evaluate for fissures as well as skin tags and fistulas, which may be seen in Crohn disease ( Fig. 16.7 ). Local intense tenderness, fever, and erythema of the perianal area may suggest group A β-hemolytic streptococcus infection. Infants and toddlers may have a palpable right lower quadrant abdominal mass, which suggests intussusception. Skin examination may show purpura, which, although not always present initially, is seen in Henoch-Schönlein purpura; it may also be seen in hemolytic uremic syndrome. Erythema nodosum or pyoderma gangrenosum is present in approximately 3% of children with inflammatory bowel disease and may correlate with disease severity.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here