Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In general, there is little in the way of patient preparation for a renal scan, although patients should be well hydrated. Patients should refrain from taking furosemide, which is sometimes given during the scan to help evaluate for obstruction. Angiotensin converting enzyme (ACE) inhibitors should also be avoided because they can alter the kidney's ability to regulate perfusion. However, captopril, an ACE inhibitor, may be given during the study to help assess for renovascular disease. The scan itself usually takes approximately 30 minutes and begins with the intravenous injection of a radiotracer followed by imaging in the posterior projection for native kidneys and the anterior projection for renal transplants.
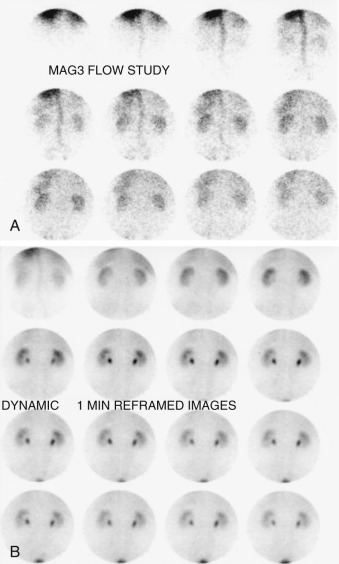
Renal scans are usually performed with one of two technetium-99m ( 99m Tc) compounds: diethylenetriamine pentaacetic acid (DTPA) or mercaptoacetyltriglycine (MAG3). The perfusion component of the study, measured during the first minute after injection of the radiotracer, should reveal renal perfusion within several seconds of aortic activity. Renal blood flow should be symmetric and greater than that in the spleen and liver (each kidney receives approximately 10% of cardiac output compared with <5% for the liver and spleen). Cortical images are then obtained usually every minute for approximately 25 minutes. Cortical uptake should be symmetric with no focal defects. Radiotracer activity should be observed entering the collecting system by 5 minutes (the cortical transit time, i.e., how long it takes for urine to appear in the collecting system). Urine should flow freely into the bladder without retention or obstruction ( Figure 81-1 ).
Most causes involve mass effect from a lesion such as a cyst, abscess, or tumor (benign or malignant) that has altered renal morphologic features. Scarring in the kidney from chronic pyelonephritis or chronic ureteral reflux can also lead to focally decreased renal flow. Other causes include renal infarction or a renal hematoma associated with trauma or surgery. Such abnormalities can be either unifocal or multifocal and can be more thoroughly evaluated with structural imaging techniques such as ultrasonography (US), computed tomography (CT), or magnetic resonance imaging (MRI).
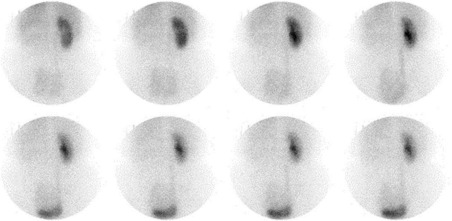
A common cause of a unilaterally enlarged kidney is compensatory hypertrophy for an absent or poorly functioning contralateral kidney ( Figure 81-2 ). Hydronephrosis can also result in an enlarged kidney and may affect one or both kidneys. Patients with polycystic renal disease may also have kidneys that appear enlarged, often with multiple cold defects seen due to cysts. Renal vein thrombosis can also result in ipsilateral enlargement of a kidney related to the engorgement of blood.
Dysplastic kidney.
Postinflammatory atrophy.
Postobstructive atrophy.
Renal artery stenosis.
Radiation nephritis.
Correlation with clinical history and structural imaging techniques can help to differentiate the underlying etiology. Bilaterally small kidneys are usually a manifestation of end-stage renal disease, which can be caused by many underlying etiologies.
Nonvisualization of a kidney on a renal scan can be seen with prior nephrectomy, renal agenesis, post-traumatic or postsurgical injury to the kidney's vascular supply, or other vascular or obstructive processes. Vascular disorders that result in nonvisualization of a kidney include renal artery occlusion and renal vein occlusion. Neoplastic disease can also impair renal function or perfusion, resulting in nonvisualization. Finally, chronic obstruction, such as from ureteropelvic junction (UPJ) obstruction, can eventually result in absent flow and function in a kidney (see Figure 81-2 ).
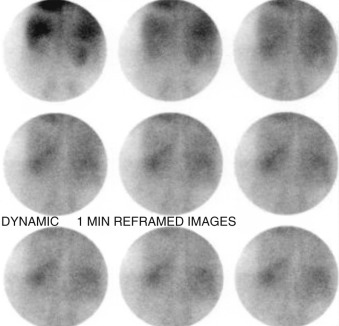
Processes affecting both kidneys are often more systemic in nature. Glomerulonephritis can cause decreased flow in both kidneys. Acute or chronic renal failure also results in decreased flow and function in both kidneys. There can always be bilateral vascular or obstructive processes, and these should also be considered. Finally, technical factors, such as injecting the wrong radiotracer or acquiring images at the wrong photopeak, can be considered if the kidneys are not visualized ( Figure 81-3 ).
A renal scan in a patient with renal artery stenosis often appears normal because the renin-angiotensin system causes a vasoconstriction of the efferent arterioles, which helps maintain the pressure across the glomeruli, preserving renal function. A renal scan performed after the administration of captopril or other ACE inhibitor reveals abnormal flow and function because the regulatory mechanism of angiotensin is blocked by the ACE inhibitor. A scan using 99m Tc DTPA after captopril should show evidence of diminished flow and function in a kidney with renal artery stenosis compared with a renal scan without captopril. Generally, the overall sensitivity and specificity of this test are approximately 90% and 95%, respectively. With the advent of magnetic resonance angiography (MRA), there has been considerably less use of captopril renal scintigraphy, but it is still sometimes helpful to evaluate the functional significance of partially stenotic renal arteries.
A renal scan within 1 day of surgical transplantation can be very useful for detecting overall flow in the transplanted kidney to ensure that the transplant renal artery is patent. The renal scan can also be used to help evaluate the extent of acute tubular necrosis (ATN), which occurs in virtually every transplant, although it is much more common and severe in cadaveric transplants compared with living-related transplants ( Figure 81-4 ). ATN is typically diagnosed on a renal scan when there is normal renal flow but diminished cortical transit of the radiotracer (the normal cortical transit time is usually less than 5 minutes). The degree of ATN can be evaluated based on the delay in cortical transit, with severe ATN showing no significant cortical function. A renal scan can also help with the evaluation of hyperacute rejection, which would appear as near-absent perfusion of the renal transplant. Renal scans can also provide information regarding possible obstruction or leaks of urine (most often occurring within several days after transplantation).
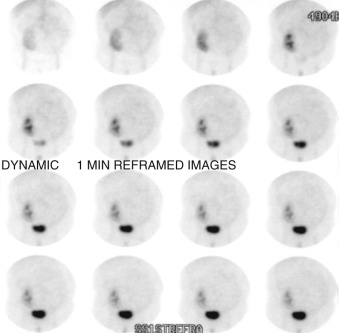
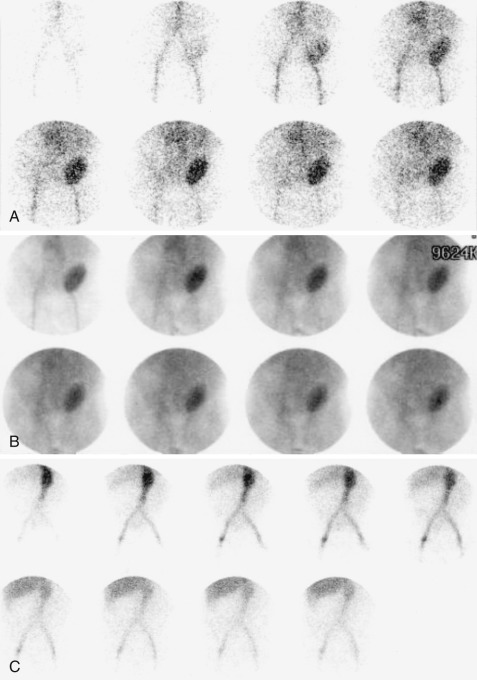
Clinically, ATN occurs almost immediately after transplantation whereas chronic rejection generally occurs over several days to several weeks or longer after transplantation. ATN can occur later, although it is usually associated with some specific event that damages the transplant and usually takes several weeks or months to resolve after transplantation. Renal scan findings are often different for ATN and rejection. ATN shows normal or only slightly diminished perfusion of the kidney with a delayed cortical transit time, whereas rejection is usually associated with diminished flow with mildly impaired cortical function. In severe rejection, flow and function are both markedly reduced. In both cases, when minimal or no urine is produced, it is impossible to exclude a leak or urinary tract obstruction as the underlying etiology, because both of these entities require some radioactive urine to be excreted into the urothelial system. It is also possible to have superimposed ATN and rejection, particularly when a renal scan reveals diminished flow and function. A clinician may have to treat such patients for both conditions ( Figure 81-5 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here