Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Fractures account for 10–15% of all childhood injuries. The anatomic, biomechanical, and physiologic differences in children account for unique fracture patterns and management. Fracture terminology helps describe fractures ( Table 198.1 ).
| Complete | The bone fragments separate completely |
| Incomplete | The bone fragments are still partially joined |
| Linear | Referring to a fracture line that is parallel to the bone’s long axis |
| Transverse | Referring to a fracture line that is at a right angle to the bone’s long axis |
| Oblique | Referring to a fracture line that is diagonal to the bone’s long axis |
| Spiral | Referring to a twisting fracture |
| Comminution | A fracture that results in several fragments |
| Compaction | The bone fragments are driven into each other |
| Angulation | The fragments of bone are at an angle to each other |
| Rotation | The fragments spun (rotated) on each other when the bone broke |
| Shortening | The fractured ends of the bones overlap |
| Open | A fracture in which the bone has pierced the skin |
The pediatric skeleton has a higher proportion of cartilage and a thicker, stronger, and more active periosteum capable of producing a larger callus more rapidly than in an adult. The thick periosteum may decrease the rate of displaced fractures and stabilize fractures after reduction. Because of the higher proportion of cartilage, the skeletally immature patient can withstand more force before deformation or fracture than adult bone. As children mature into adolescence, the rate of healing slows and approaches that of adults.
Buckle or torus fractures occur after compression of the bone; the bony cortex does not truly break. These fractures will typically occur in the metaphysis and are stable fractures that heal in approximately 4 weeks with immobilization. A common example is a fall onto an outstretched arm causing a buckle fracture in the distal radius; removable wrist splints have been effective for management of these fractures.
Complete fractures occur when both sides of bony cortex are fractured. This is the most common fracture and may be classified as comminuted, oblique, transverse, or spiral, depending on the direction of the fracture line.
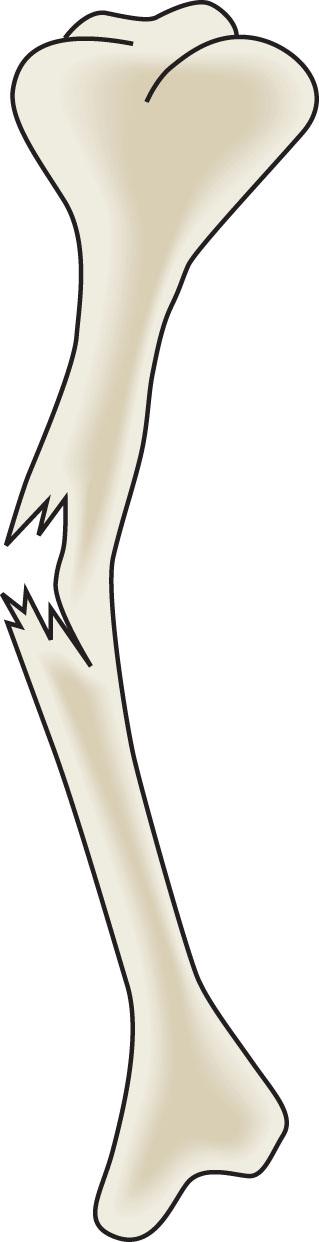
Greenstick fractures occur when a bone is angulated beyond the limits of plastic deformation. The bone fails on the tension side and sustains a bend deformity on the compression side. The force is insufficient to cause a complete fracture ( Fig. 198.1 ).
Bowing fractures demonstrate no fracture line evident on radiographs, but the bone is bent beyond its limit of plastic deformation. This is not a true fracture but will heal with periosteal reaction.
Fractures involving the growth plate constitute about 20% of all fractures in the skeletally immature patient. These fractures are twice as common in males. The peak incidence is 13–14 years in males and 11–12 years in females. The distal radius, distal tibia, and distal fibula are the most common locations.
Ligaments frequently insert onto epiphyses. Thus, traumatic forces to an extremity may be transmitted to the physis, which is not as biomechanically strong as the metaphysis; it may fracture with mechanisms of injury that may cause sprains in the adult. The growth plate is most susceptible to torsional and angular forces.
Physeal fractures are described using Salter-Harris classification , which allows for prognostic information regarding premature closure of the growth plate and poor functional outcomes. The higher the type number, the more likely the patient will have complications. There are five main groups ( Fig. 198.2 ):
Type I: transverse fracture through the physis; growth disturbance is unusual
Type II: fracture through a portion of the physis and metaphysis; most common type of Salter-Harris fracture (75%)
Type III: fracture through a portion of the physis and epiphysis into the joint that may result in complication because of intraarticular component and because of disruption of the growing or hypertrophic zone of the physis
Type IV: fracture through the metaphysis, physis, and epiphysis with a high risk of complication
Type V: a crush injury to the physis with a poor functional prognosis
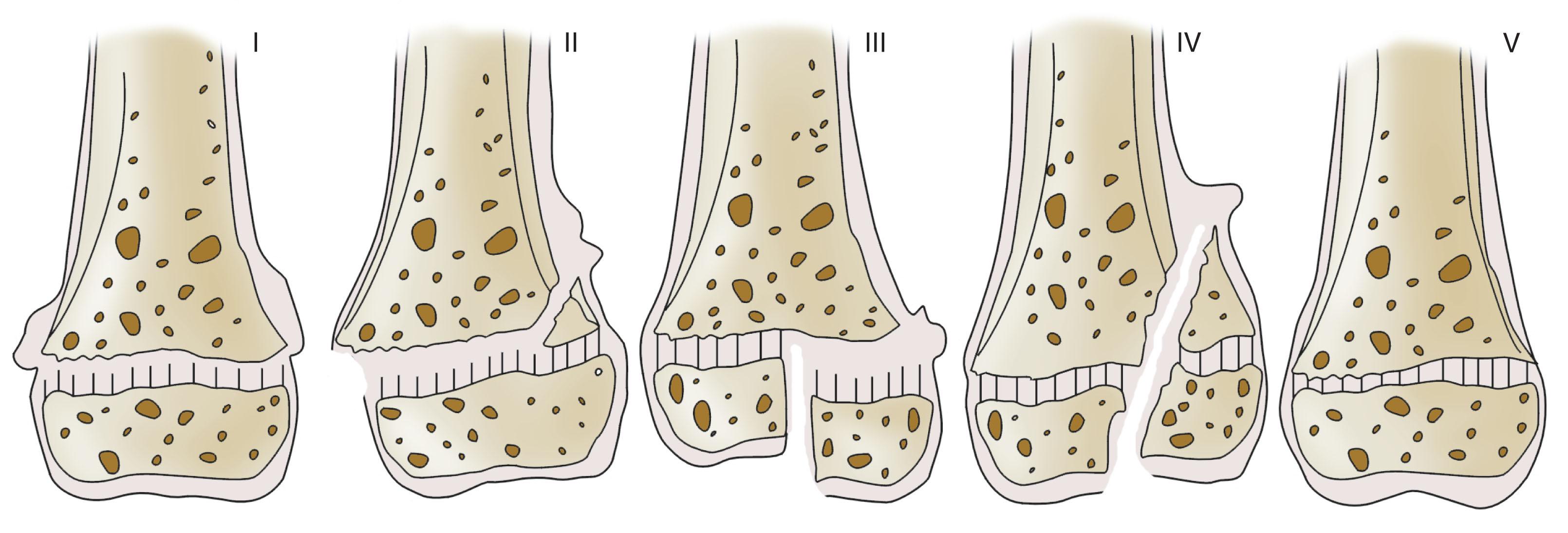
Types I and II fractures can often be managed by closed reduction and do not require perfect alignment. A major exception is the type II fracture of the distal femur, which is associated with a poor outcome unless proper anatomic alignment is obtained. Types III and IV fractures require anatomic alignment for successful treatment. Type V fractures are rare and often result in premature closure of the physis.
The majority of pediatric fractures can be managed with closed methods. Some fractures need closed reduction to improve alignment. Approximately 4% of pediatric fractures require internal fixation. Patients with open physes are more likely to require internal fixation if they have one of the following fractures:
Displaced epiphyseal fractures
Displaced intraarticular fractures
Fractures in a child with multiple injuries
Open fractures
Unstable fractures
The goal of internal fixation is to improve and maintain anatomic alignment. This is usually done with Kirschner wires, Steinmann pins, and cortical screws with subsequent external immobilization in a cast until healing is satisfactory. After healing, the hardware is frequently removed to prevent incorporation into the callus and prevent physeal damage.
External fixation without casting may be necessary for pelvic fractures causing hemodynamic instability. Fractures associated with soft tissue loss, burns, and neurovascular damage may benefit from external fixation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here